Granulomatous Conjunctivitis: Causes, Symptoms, Diagnosis, and Treatment
Comprehensive guide to granulomatous conjunctivitis: symptoms, causes, diagnosis, and treatment options.
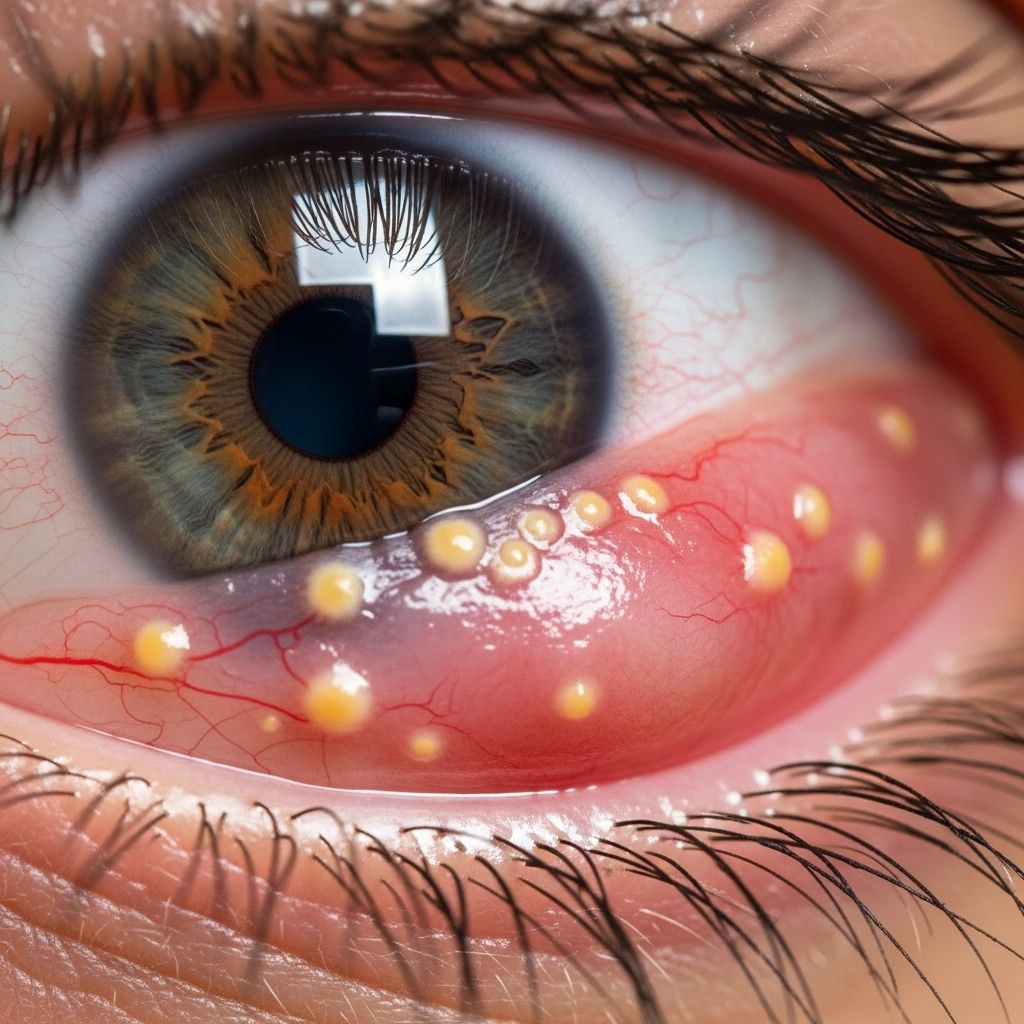
Granulomatous conjunctivitis is a rare but important type of conjunctival inflammation, distinguished by the formation of granulomas—small nodules due to a chronic inflammatory response—in the conjunctiva (the thin, transparent membrane that lines the inside of the eyelids and the white part of the eye). While most cases of conjunctivitis are acute and self-limiting, granulomatous conjunctivitis signals a more complex underlying cause that often requires specialized attention and management.
What is Granulomatous Conjunctivitis?
Granulomatous conjunctivitis is an ocular condition in which the conjunctiva—the clear tissue covering the white of your eyes and the inside of your eyelids—develops granulomas. Granulomas are small, nodular clusters of immune cells formed as a result of chronic inflammation. They can develop when the body’s immune system attempts to wall off substances it perceives as foreign but cannot eliminate, such as certain infections or irritants.
This type of conjunctivitis is considered uncommon and typically serves as a clue for doctors that the cause may be something more significant than viral or bacterial conjunctivitis, often pointing toward chronic infections, immune-related conditions, or exposures to certain irritants.
Symptoms of Granulomatous Conjunctivitis
Granulomatous conjunctivitis may present with symptoms similar to other types of conjunctivitis but has distinctive features due to the underlying granulomatous process. Common symptoms include:
- Redness: Persistent redness in one or both eyes.
- Eye discomfort: Mild to moderate pain, irritation, or a gritty sensation.
- Eyelid swelling: Sometimes the eyelids become puffy or swollen.
- Foreign body sensation: Feeling as though something is in the eye, often due to nodular lesions on the conjunctiva.
- Excessive tearing or discharge: Watery or sometimes mucopurulent (pus-like) discharge.
- Visual changes: Blurred vision can occur if inflammation spreads or if there is significant discharge.
- Granulomas: Visible lumps or nodules in the conjunctiva; these may be yellowish, gray, or pinkish in color and can be single or multiple.
Depending on the underlying cause, other systemic symptoms such as fever, skin lesions, or swollen lymph nodes may also be present.
Possible Causes of Granulomatous Conjunctivitis
Granulomatous conjunctivitis is not a disease in itself but a manifestation of various underlying conditions. The causes can be broadly classified into infectious and non-infectious categories:
Infectious Causes
- Tuberculosis (Mycobacterium tuberculosis): Ocular tuberculosis can produce granulomas in the conjunctiva, especially in endemic regions.
- Cat-scratch disease (Bartonella henselae): Transmitted by scratches or bites from cats, this infection is a key infectious cause.
- Syphilis (Treponema pallidum): This sexually transmitted infection can rarely cause granulomatous conjunctivitis as part of systemic disease.
- Parinaud oculoglandular syndrome: An umbrella term for conditions where granulomatous conjunctivitis is accompanied by swollen lymph nodes in front of the ear (preauricular lymphadenopathy), often due to Bartonella or less commonly tularemia or tuberculosis.
- Fungal or parasitic infections: Rare but can be seen in immunocompromised patients.
Non-Infectious Causes
- Sarcoidosis: A systemic inflammatory disease that can cause granulomas in various organs, including the eye.
- Foreign bodies: Prolonged exposure to certain plant or animal materials, dust, or other foreign substances can invoke granuloma formation.
- Contact allergy: Chronic reactions to eye drops or preservatives may occasionally result in granulomatous changes.
- Other immune-mediated diseases: Including granulomatosis with polyangiitis (formerly Wegener’s granulomatosis).
Risk Factors
Although anyone can develop granulomatous conjunctivitis, certain groups are at increased risk, including:
- People with weakened immune systems: For example, individuals with HIV/AIDS, those on immunosuppressive medications, or patients with other chronic health conditions.
- Residents of or travelers to areas endemic for tuberculosis, cat-scratch disease, or certain fungal infections.
- Individuals in close contact with cats or other animals: Especially children or those who work with animals regularly.
- People with a history of autoimmune or inflammatory disorders: Such as sarcoidosis or granulomatosis with polyangiitis.
How is Granulomatous Conjunctivitis Diagnosed?
Because the symptoms can overlap with those of more common types of conjunctivitis, diagnosing granulomatous conjunctivitis involves a careful history, physical examination, and often specialized tests. Steps may include:
- Clinical Evaluation: An eye doctor will assess the type and appearance of conjunctival lesions, their size, color, and associated signs (such as lymph node swelling).
- Detailed Medical History: Questions about recent travel, animal exposures, sexual history, past medical conditions, current medications, and any trauma or foreign body exposure.
- Laboratory Tests: These may include:
- Conjunctival swabs or scrapings for bacterial, viral, or fungal cultures.
- Special stains and cultures for tuberculosis or fungi.
- Blood tests for syphilis (RPR, FTA-ABS), Bartonella, or HIV if indicated.
- Imaging studies (e.g., chest X-ray) if systemic disease is suspected, such as tuberculosis or sarcoidosis.
- Biopsy of the conjunctival nodule in persistent or unclear cases.
Early and accurate diagnosis is essential because some causes can threaten vision or signal serious systemic illness.
Treatment Options for Granulomatous Conjunctivitis
Treatment of granulomatous conjunctivitis depends entirely on the underlying cause. Managing the root issue is critical for symptom resolution and preventing complications. The following table summarizes some common causes and their treatments:
| Cause | First-line Treatment | Additional Notes |
|---|---|---|
| Tuberculosis | Anti-tuberculosis antibiotics (multi-drug therapy) | Consult infectious disease specialist; monitor systemic involvement |
| Cat-scratch disease | Azithromycin (antibiotic) | May be combined with symptomatic eye care |
| Syphilis | Penicillin (intramuscular or intravenous) | Requires reporting and follow-up for other systemic effects |
| Sarcoidosis | Corticosteroids (topical, oral, or injection) | Monitor for systemic complications; may require rheumatology involvement |
| Foreign body/irritants | Removal of the offending agent; supportive care | Topical steroids rarely needed; ensure injury risk is eliminated |
| Allergic or immune-mediated causes | Antihistamines; corticosteroids (topical or systemic) | Allergy testing and avoidance may be recommended |
- Symptomatic care may include the use of lubricating eyedrops for comfort, cool compresses, and in certain cases, topical steroids to reduce inflammation after infection has been excluded.
- Follow all medical advice and complete the full course of treatment.
- Self-medication is strongly discouraged because using the wrong type of medication—such as steroids in the presence of an infection—can worsen outcomes.
Potential Complications
- Vision loss: Untreated or severe cases may lead to scarring or spread of infection, potentially affecting vision.
- Chronic discomfort: Ongoing inflammation may result in persistent foreign body sensation or irritation.
- Spread of infection: Some infections can affect other parts of the eye (cornea, uvea), or even become systemic and life-threatening.
- Scarring: Granulomas may heal with scarring, possibly affecting the appearance or function of the eye.
- Medication side effects: Prolonged steroid use carries a risk of increased intraocular pressure or cataract formation.
When to See a Doctor
Since granulomatous conjunctivitis can indicate a severe or chronic underlying issue, it is critical to consult an eye doctor promptly if you experience:
- Persistent eye redness or irritation lasting more than a few days
- Visible lumps, nodules, or unusual lesions on the eye surface
- Blurred vision, visual changes, or pain
- Swelling of the lymph nodes in front of the ears
- Associated systemic symptoms such as fever, rashes, fatigue, or weight loss
Early evaluation by an ophthalmologist can help rule out dangerous causes, ensure proper management, and reduce the risk of lasting complications.
Prevention
While many causes of granulomatous conjunctivitis are not entirely preventable, some steps can lower your risk:
- Practice good hand hygiene to reduce spread of infectious agents.
- Avoid touching or rubbing your eyes, especially with unwashed hands or after handling pets.
- Seek immediate care for eye injuries or when a foreign body enters the eye.
- Protect your eyes in dusty, windy, or high-risk environments.
- Control and monitor systemic diseases such as tuberculosis or sarcoidosis.
- Avoid contact with sick animals or those likely to scratch (especially for children).
Frequently Asked Questions (FAQs)
What is the prognosis for granulomatous conjunctivitis?
With timely and appropriate treatment, most people recover fully. The prognosis depends on the underlying cause and speed of diagnosis and management. Complications are rare when the source is identified early and managed properly.
Can granulomatous conjunctivitis spread to others?
The underlying cause determines the risk of transmission. Some infections (such as tuberculosis or cat-scratch disease) can be contagious, while noninfectious causes or those linked to autoimmune conditions are not.
Can I use over-the-counter eye drops for granulomatous conjunctivitis?
Over-the-counter lubricating drops may provide temporary relief, but they do not treat the underlying cause. Never self-treat persistent eye redness, pain, or nodules—see an eye care provider for evaluation.
Is granulomatous conjunctivitis dangerous?
If left untreated, it can lead to serious complications, including vision loss or spread of systemic illness. Prompt professional management is essential for a safe recovery.
Can children get granulomatous conjunctivitis?
Yes, while rare, children can develop this condition, particularly if exposed to animals carrying relevant infections or in high-risk environments.
Key Takeaways
- Granulomatous conjunctivitis is a rare form of conjunctival inflammation characterized by nodular lesions and usually signals a significant underlying health issue.
- Prompt diagnosis and treatment are vital to prevent complications, including vision loss or systemic involvement.
- The condition may be caused by infections (such as tuberculosis or cat-scratch disease), immune diseases (like sarcoidosis), or reactions to foreign bodies and irritants.
- Treatment targets the underlying cause and may include antibiotics, anti-inflammatory medications, and supportive care.
- Consult an ophthalmologist for persistent symptoms, as they may indicate a need for specialized care.
References
- https://eyewiki.org/Conjunctivitis
- https://en.wikipedia.org/wiki/Conjunctivitis
- https://www.ncbi.nlm.nih.gov/books/NBK541034/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6402948/
- https://www.mayoclinic.org/diseases-conditions/pink-eye/symptoms-causes/syc-20376355
- https://www.allaboutvision.com/conditions/pyogenic-granuloma/
- https://my.clevelandclinic.org/health/diseases/pink-eye-conjunctivitis
Read full bio of medha deb












