Glioblastoma: Diagnosis, Advanced Treatments, and Patient Care
Explore the full spectrum of glioblastoma diagnosis, treatment options, and care innovations, guided by the latest clinical expertise.
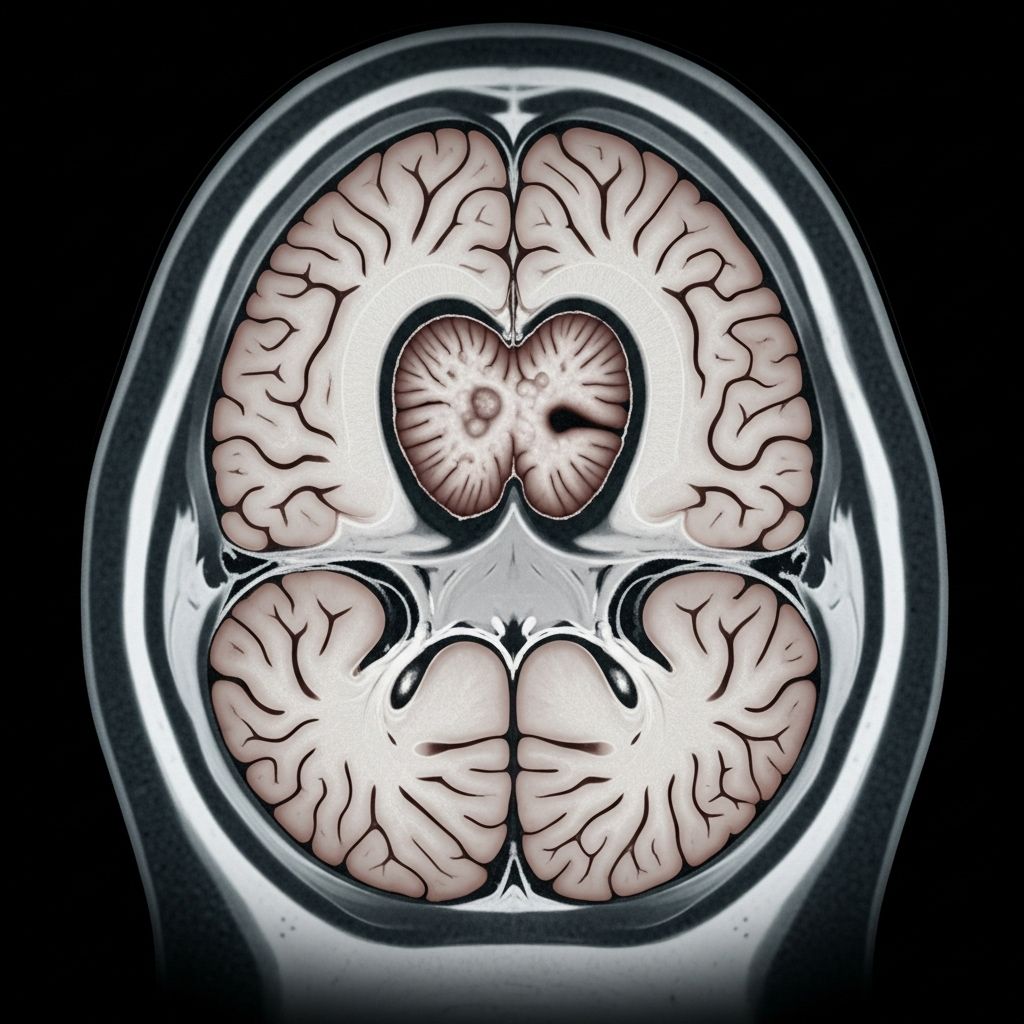
Glioblastoma is an aggressive form of brain cancer, also known as glioblastoma multiforme. It arises from the supportive tissue of the brain and is the most common as well as the most aggressive type of primary malignant brain tumor in adults. The management of glioblastoma poses significant challenges due to its resistance to conventional therapies and its tendency to infiltrate healthy brain tissue.
Diagnosis of Glioblastoma
The diagnostic process for glioblastoma is a comprehensive journey that combines advanced imaging, neurological assessments, and laboratory studies. Accurately determining glioblastoma is essential to guide individualized therapy.
- Imaging Tests:
- MRI (Magnetic Resonance Imaging): The primary imaging tool, utilizing contrast agents to distinguish tumor tissue from healthy tissue. Specialized MRI types, such as functional MRI, perfusion MRI, and magnetic resonance spectroscopy, provide additional details about brain function, blood flow, and chemical composition around the tumor.
- CT (Computed Tomography) Scans: Useful when MRI is not an option; provides rapid cross-sectional images of the brain.
- Positron Emission Tomography (PET): Sometimes used to map tumor metabolic activity. Advanced imaging, such as 18F-DOPA PET scans, may help distinguish tumor activity and guide targeted therapies.
- Biopsy: A critical step, performed either during surgery or as a separate procedure. Tissue samples are examined under a microscope to definitively diagnose glioblastoma and characterize genetic markers that can guide therapy.
- Neurological Evaluation: Assessment of vision, hearing, balance, coordination, strength, and reflexes is conducted to gauge the impact of the tumor and tailor treatment strategies.
Treatment Options for Glioblastoma
Planning glioblastoma treatment requires a multidisciplinary approach. The care team considers tumor size, location, genetic profile, and the patient’s health and preferences to develop a personalized plan.
Surgery to Remove Glioblastoma
Surgical removal (resection) is often the initial step. The goal is to eliminate as much tumor as safely possible; however, due to the tumor’s tendency to invade surrounding healthy tissue, complete removal is typically not possible.
- Neurosurgical Techniques:
- Traditional and Computer-Assisted Surgery: Surgeons use advanced navigation systems to distinguish tumor from healthy tissue.
- Intraoperative MRI (iMRI): MRI scans during surgery help guide tissue removal in real time, increasing precision and reducing risk.
- Awake Brain Surgery: For tumors near functional areas, the patient may remain awake for part of the surgery, enabling surgeons to preserve critical abilities such as speech and movement.
- Laser Surgery: Thermal ablation can target small or deep-seated tumors with minimal damage to healthy brain structures.
Most patients need additional treatments after surgery to address remaining cancer cells.
Radiation Therapy
Radiation uses high-energy beams to destroy tumor cells. The therapy is almost always recommended after surgery and may be used in combination with chemotherapy. Advanced radiation techniques improve tumor targeting while minimizing damage to healthy brain tissue.
- Standard External Beam Radiation: Includes X-rays and, in some cases, proton therapy that can precisely focus radiation on the tumor.
- Advanced Techniques:
- 3D Conformal Radiation Therapy
- Image-Guided Radiation Therapy (IGRT)
- Intensity-Modulated Radiation Therapy (IMRT): Modulates beam intensity to shape dose delivery.
- Proton Beam Therapy: Delivers focused proton beams, sparing more normal tissue. Promising results have been seen with short-course, hypofractionated (higher dose, fewer sessions) proton therapy using advanced imaging to target metabolically active tumor regions in older patients.
- Treatment Duration: Traditional radiation is given over three to six weeks, but some new protocols allow treatment in as little as one to two weeks for select patients.
Chemotherapy
Chemotherapy uses drugs to kill or slow the growth of cancer cells. It is often administered orally or intravenously and may be delivered during or after radiation therapy.
- Temozolomide: The main chemotherapy drug for glioblastoma, generally taken by mouth, often in tandem with radiation for added effect.
- Other Agents: Various drugs or drug combinations may be considered if glioblastoma progresses or recurs.
Targeted Drug Therapy
Targeted therapies focus on specific abnormalities within cancer cells. For some patients, especially those with certain tumor mutations, these drugs may be recommended. These approaches are typically available through clinical trials.
- Bevacizumab: A monoclonal antibody that targets vascular endothelial growth factor (VEGF) to reduce the tumor’s blood supply, approved for use in certain cases of recurrent glioblastoma.
Clinical Trials and Emerging Therapies
Participation in clinical trials offers access to pioneering treatments not yet widely available.
- Immunotherapy: Investigating ways to harness the immune system against glioblastoma cells.
- Gene Therapy: Seeks to alter tumor genetics to control growth or enhance treatment response.
- Novel Drug Delivery Techniques: Using next-generation formulations to better penetrate the blood-brain barrier.
- Short-Course Proton Therapy: Mayo Clinic’s research demonstrates significant survival benefit and improved quality of life in older patients by combining proton therapy with advanced imaging.
Rehabilitation and Supportive Care
The aggressive nature of glioblastoma and its treatment can have substantial effects on physical and cognitive function. Rehabilitation and supportive care services are vital for preserving quality of life and maximizing independence.
- Physical Therapy: Assists with regaining strength, balance, and coordination.
- Occupational Therapy: Helps with daily living activities and adapting to new limitations.
- Speech and Language Therapy: Supports language, communication, and swallowing functions as needed.
- Psychosocial Support: Counseling, social work, and patient support groups address emotional and psychological needs for both patients and families.
Care at Mayo Clinic
Mayo Clinic’s approach to glioblastoma care integrates expertise across multiple specialties, ensuring innovative and patient-centered treatment.
- Multidisciplinary Team: Including neuro-oncologists, neurosurgeons, neurologists, oncologists, radiation oncologists, pathologists, and radiologists, working in close collaboration.
- Fast Access to Evaluation and Treatment: Scheduling and test results are coordinated for efficient care, often compressing evaluation and treatment timelines from months to days.
- Cutting-Edge Technology:
- Advanced MRI imaging, functional assessments, and precision-guided surgical and radiation techniques are routinely available.
- Mayo Clinic is a National Cancer Institute-designated comprehensive cancer center, recognized for its scientific excellence and multidisciplinary approach.
- Innovative Research: Active involvement in national clinical trials, such as those sponsored by the Alliance for Clinical Trials in Oncology, expands access to novel therapies and helps drive advances in glioblastoma treatment.
Prognosis and Outlook
Glioblastoma remains one of the most challenging brain tumors to treat. The prognosis depends on several factors, including age, overall health, tumor location, the extent of surgical removal, and specific genetic characteristics of the tumor.
- Typical median survival with standard therapy is around 12–15 months. Without treatment, survival is only a few months.
- Emerging therapies, such as short-course proton beam treatment and targeted approaches, are providing longer survival and improved quality of life for select patient groups.
- Participation in clinical trials may open the door to new options as research continues to advance the field.
Self-Care and Coping Strategies
Living with glioblastoma can be overwhelming. Patients and families are encouraged to seek support and develop coping strategies to manage the emotional and practical challenges of this diagnosis.
- Education: Staying informed about the disease and its treatments empowers active participation in care choices.
- Emotional Support: Engage with support groups—either in-person or online—to connect with others in similar situations.
- Advance Planning: Discuss goals of care, advance directives, and legal matters to ensure that personal wishes are respected throughout treatment.
- Lifestyle Modifications: Emphasize nutrition, physical activity as tolerated, and adequate rest to support strength and well-being.
Frequently Asked Questions (FAQs)
Q: How is glioblastoma diagnosed?
A: Diagnosis is based on neurological evaluation, advanced imaging (MRI and sometimes PET or CT), and often a biopsy to confirm the tumor type and assess for genetic markers.
Q: What is the standard treatment for glioblastoma?
A: Standard treatment typically includes maximal safe surgical removal, followed by radiation therapy often combined with the chemotherapy drug temozolomide. Emerging approaches may incorporate targeted therapies or clinical trials for new treatments.
Q: Are there new, promising therapies for glioblastoma?
A: Yes. Mayo Clinic researchers are investigating hypofractionated proton beam therapy (shorter, intensified regimens), advanced molecular imaging, targeted treatments, and personalized medicine approaches that show improved survival and quality of life in selected patients.
Q: What support resources are available for patients and families?
A: Mayo Clinic and many cancer centers offer multidisciplinary rehabilitation, psychological support, social work, and patient support groups, in addition to educational resources for managing life with glioblastoma.
Q: Can glioblastoma be cured?
A: At present, glioblastoma cannot generally be cured. However, treatment strategies can significantly extend survival, alleviate symptoms, and improve quality of life. Participation in clinical trials may provide access to cutting-edge therapies.
References
- https://www.mayoclinic.org/diseases-conditions/glioblastoma/diagnosis-treatment/drc-20569078
- https://www.mayoclinic.org/diseases-conditions/glioma/diagnosis-treatment/drc-20350255
- https://www.mayoclinic.org/diseases-conditions/glioblastoma/care-at-mayo-clinic/mac-20569080
- https://www.mayoclinic.org/diseases-conditions/glioblastoma/symptoms-causes/syc-20569077
- https://www.mayo.edu/research/clinical-trials/diseases-conditions/glioblastoma
- https://cancerblog.mayoclinic.org/2025/01/16/breakthrough-in-treatment-approach-showing-promise-in-the-fight-against-glioblastoma/
- https://www.youtube.com/watch?v=DP7p09z_mOY
- https://www.mayoclinic.org/diseases-conditions/glioma/care-at-mayo-clinic/mac-20350259
- https://www.mayoclinic.org/diseases-conditions/brain-tumor/diagnosis-treatment/drc-20350088
Read full bio of medha deb












