How Glaucoma Affects the Optic Nerve and Vision Loss
Understand how glaucoma damages the optic nerve, its symptoms, causes, prevention, and treatment.
Glaucoma is an eye disease that causes progressive damage to the optic nerve, often resulting in irreversible vision loss. This article explores the mechanisms of glaucoma, its impact on the optic nerve, major causes, symptoms, risk factors, diagnostic methods, available treatments, prevention strategies, and answers to frequently asked questions.
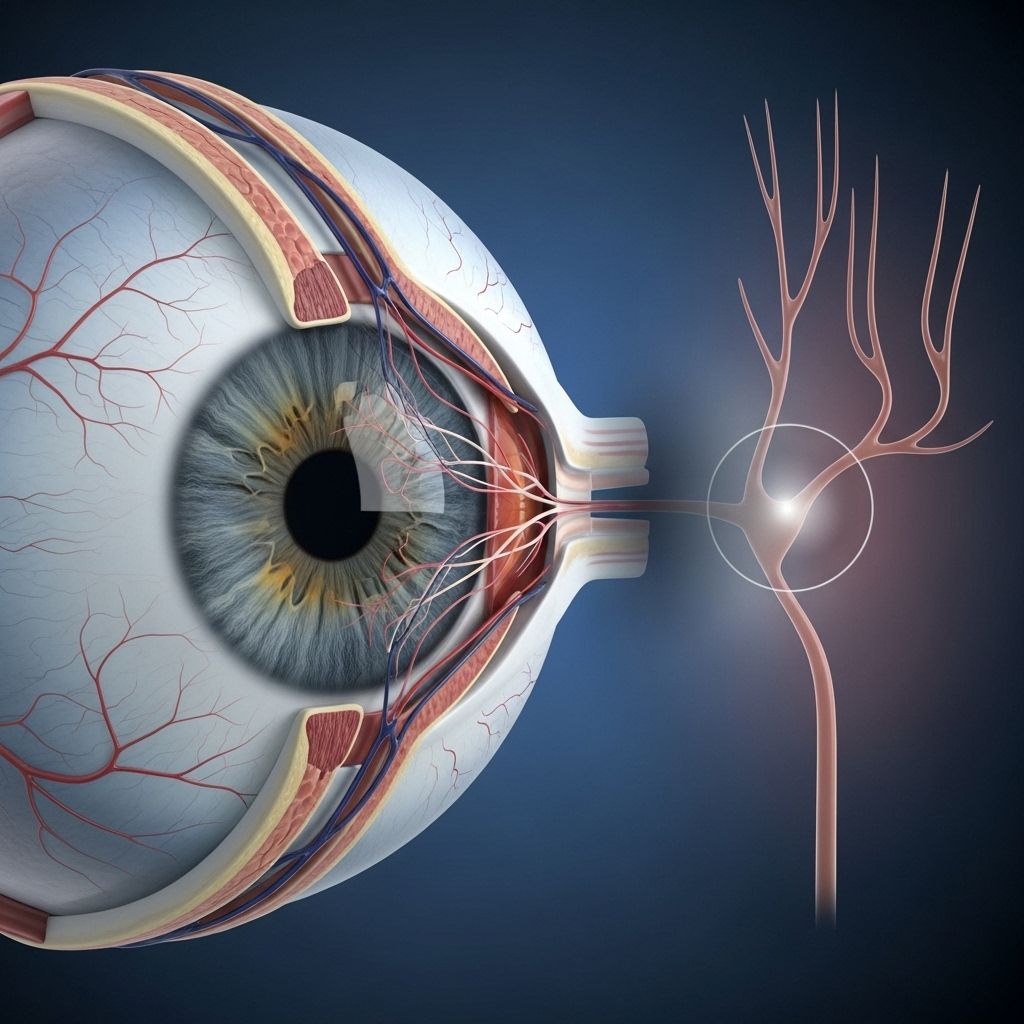
Understanding the Optic Nerve
The optic nerve serves as the communication cable between your eye and brain, transmitting visual information from the retina to the visual cortex. Damage to this nerve, regardless of cause, leads to impaired vision and, if left untreated, permanent blindness.
- The optic nerve contains over a million nerve fibers.
- It connects the back of your eye (retina) to your brain’s visual processing centers.
- Any interruption in this pathway can result in blind spots or total vision loss, depending on the severity and location of the damage.
What Is Glaucoma?
Glaucoma refers to a group of eye diseases marked by progressive and irreversible damage to the optic nerve, usually due to increased intraocular pressure (IOP), but it can occur even with normal eye pressure. It’s a major cause of blindness worldwide.
- Most types are chronic and gradually worsen over years.
- The disease is often painless and symptomless at first, earning it the nickname “the silent thief of sight.”
- Glaucoma can affect one or both eyes.
How Glaucoma Damages the Optic Nerve
Damage in glaucoma starts at the point where nerve fibers from the retina converge and exit the eye — known as the optic disc. Increased pressure within the eye damages these delicate fibers, but other factors like poor blood flow or abnormal pressure gradients can also injure the nerve.
- High eye pressure compresses the optic nerve fibers, leading to their gradual degeneration.
- The optic disc develops a characteristic appearance known as “cupping,” where the healthy nerve tissue shrinks and the central hollow becomes larger.
- Retinal ganglion cells die, progressively reducing the quality and quantity of visual signals sent to the brain.
- Vision loss typically starts with peripheral (side) vision and may progress to central vision loss in advanced cases.
Types of Glaucoma
Glaucoma is classified into several major types based on the mechanism of increased eye pressure or optic nerve damage:
- Primary Open-Angle Glaucoma (POAG): Most common form. The drainage angle formed by the cornea and iris remains open, but the trabecular meshwork slowly becomes less efficient at draining fluid, causing pressure to build up.
- Angle-Closure (Closed-Angle) Glaucoma: The drainage angle is suddenly or gradually blocked, causing a rapid or slow rise in eye pressure. Acute angle-closure is an emergency.
- Normal-Tension Glaucoma (NTG): Optic nerve damage occurs despite normal intraocular pressure. Possible explanations include poor blood flow, increased sensitivity of the optic nerve, or abnormal pressure dynamics between the eye and brain.
- Secondary Glaucoma: Results from another disease, injury, medication, or eye condition such as uveitis or advanced diabetes.
- Congenital (Childhood) Glaucoma: Rare, inherited forms that appear in infants or children due to abnormal eye development, often requiring surgery.
What Causes Glaucoma?
The underlying cause in most glaucoma is impaired drainage of aqueous humor—the fluid inside the front chamber of the eye. When this fluid cannot leave the eye efficiently, pressure builds up and damages the optic nerve. However, other factors, such as low blood supply or abnormal pressure gradients between the eye and brain, can also impair nerve health.
Top Causes and Risk Factors for Glaucoma:
- Blocking or narrowing of the eye’s drainage system (trabecular meshwork or angle)
- Genetic predisposition—family history greatly increases risk
- Age—risk rises sharply after age 60
- Ethnicity—African, Hispanic, and Asian descent face a higher risk
- High eye pressure (intraocular pressure)
- Thin corneas
- History of eye injury or surgery
- Use of corticosteroid medications
- Certain medical conditions (e.g., diabetes, hypertension, migraines)
Symptoms of Optic Nerve Damage in Glaucoma
Most forms of glaucoma advance painlessly and without noticeable symptoms in the early stages. Vision loss often occurs slowly, with initial loss of side vision (peripheral vision). As the disease progresses, people may notice:
- Blank spots or blurry patches in the peripheral vision
- Difficulty seeing in low light
- Eventually, tunnel vision (only central vision remains)
- In acute angle-closure glaucoma, symptoms may include severe eye pain, headache, nausea, vomiting, blurred vision, and halos around lights — this is a medical emergency.
How Is Glaucoma Diagnosed?
Because glaucoma causes vision loss so gradually, regular eye exams are the most effective way to detect the condition before significant nerve damage occurs. Diagnosis involves a combination of tests, including:
- Tonometry – Measures intraocular pressure (IOP)
- Ophthalmoscopy – Examines the optic nerve for signs of damage such as cupping
- Perimetry (Visual Field Test) – Assesses peripheral vision for blind spots
- Pachymetry – Measures corneal thickness, which affects IOP readings
- Gonioscopy – Checks the drainage angle structure
- Optical Coherence Tomography (OCT) – Provides a high-resolution image of the optic nerve and retinal layers
Complications of Glaucoma
- Permanent vision loss: Without treatment, glaucoma can lead to total blindness.
- Reduced quality of life: Loss of peripheral vision affects everyday activities such as driving, reading, and navigating stairs.
- Risk of falls and injuries: Visual field loss increases risk of accidents.
Prevention and Early Detection
You can reduce your risk of vision loss by recognizing the factors you can control and following a plan for regular screenings.
- Schedule comprehensive eye exams — every 2–4 years for adults under 40; every 1–3 years between 40–54; every 1–2 years for those 55–64; and yearly if over 65 or at high risk.
- Know your family eye health history.
- Control chronic conditions such as diabetes and hypertension.
- Follow healthy lifestyle practices, including regular exercise, wearing protective eyewear, and not smoking.
Treatment Options for Glaucoma
Treatment cannot restore vision already lost, but can halt or slow the progression of further damage. Treatment options depend on the type and severity of glaucoma:
- Prescription Eye Drops: First-line therapy for most, these medications reduce eye pressure by either decreasing fluid production or increasing fluid outflow.
- Oral Medications: Sometimes used when drops alone don’t lower IOP, these reduce fluid production.
- Laser Therapy: Procedures such as laser trabeculoplasty (for open-angle glaucoma) or laser iridotomy (for angle-closure glaucoma) can enhance drainage.
- Surgery: Several procedures are available to create new drainage channels, relieve blockages, or insert microscopic tubes (shunts) when medications and laser therapy are insufficient.
With ongoing treatment and monitoring, most people with glaucoma can preserve useful vision throughout life.
Glaucoma Research and Hope for the Future
Ongoing research focuses on new medications, devices, surgical techniques, and neuroprotective therapies aimed at preventing optic nerve damage at the cellular level. Early detection remains the best defense, but future breakthroughs may improve outcomes for those already affected by glaucoma.
- Neuroprotection: Therapies designed to protect or regenerate retinal ganglion cells and optic nerve fibers.
- Gene therapy: Experimental treatments to target genetic risk factors.
- Monitoring technologies: Portable devices for monitoring IOP and optic nerve health at home.
Tips for Living with Glaucoma
- Take all medications exactly as directed to maintain desired eye pressure.
- Keep all follow-up appointments with your eye care professional.
- Inform your ophthalmologist about any changes in your vision, even if they seem minor.
- Adapt your home and work environment for optimal lighting and safety.
- Engage with glaucoma support groups and resources for guidance and encouragement.
Frequently Asked Questions (FAQs)
Q: Can vision lost from glaucoma be restored?
A: Currently, vision loss due to glaucoma is permanent because optic nerve fibers do not regenerate. Early diagnosis and treatment are crucial to prevent further vision loss.
Q: Is high eye pressure always present in glaucoma?
A: No. While elevated intraocular pressure is the most common risk factor, glaucoma can occur at normal eye pressures, such as in normal-tension glaucoma.
Q: Who should be screened for glaucoma?
A: Everyone over age 40 should have regular comprehensive eye exams; those with risk factors may need more frequent screenings.
Q: What warning signs should I look for?
A: Most types have no early symptoms. Acute angle-closure glaucoma can present suddenly with severe eye pain, blurred vision, and nausea—seek emergency care if this occurs.
Q: How can I lower my risk of developing glaucoma?
A: There is no guaranteed prevention, but managing general health, regular eye exams, and early treatment of elevated eye pressure reduce risk of vision loss.
Summary Table: Glaucoma at a Glance
| Aspect | Details |
|---|---|
| What is damaged? | Optic nerve fibers connecting eye to brain |
| Main risk factor | Elevated intraocular pressure |
| Initial symptoms | Often none; peripheral vision loss as disease progresses |
| Diagnosis methods | Eye exam, pressure test, optic nerve imaging, visual field test |
| Treatment | Eye drops, laser therapy, surgery |
| Prevention | Regular eye exams, managing health conditions, family risk awareness |
Key Takeaways
- Glaucoma progressively damages the optic nerve and causes permanent vision loss if untreated.
- Most types progress without warning signs; regular exams are essential for early detection.
- Treatment focuses on lowering eye pressure and preserving remaining vision.
- Advances in research offer hope for future neuroprotective and regenerative therapies.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC2614024/
- https://www.cdc.gov/pcd/issues/2019/18_0534.htm
- https://www.medicalnewstoday.com/articles/narrow-angle-glaucoma
- https://www.brightfocus.org/resource/is-glaucoma-a-brain-disease/
- https://www.healthline.com/health/glaucoma
- https://www.healthlinejournal.org/ojs/healthline/article/view/H565
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/glaucoma
- https://www.healthlinejournal.org/index_pdf/419.pdf
- https://medlineplus.gov/opticnervedisorders.html
Read full bio of medha deb












