Glaucoma Risk After Cataract Surgery: Causes, Management & Outlook
Understand the links between glaucoma and cataract surgery, risk factors, symptoms and ongoing management for healthy vision.
Glaucoma After Cataract Surgery: Understanding the Connection
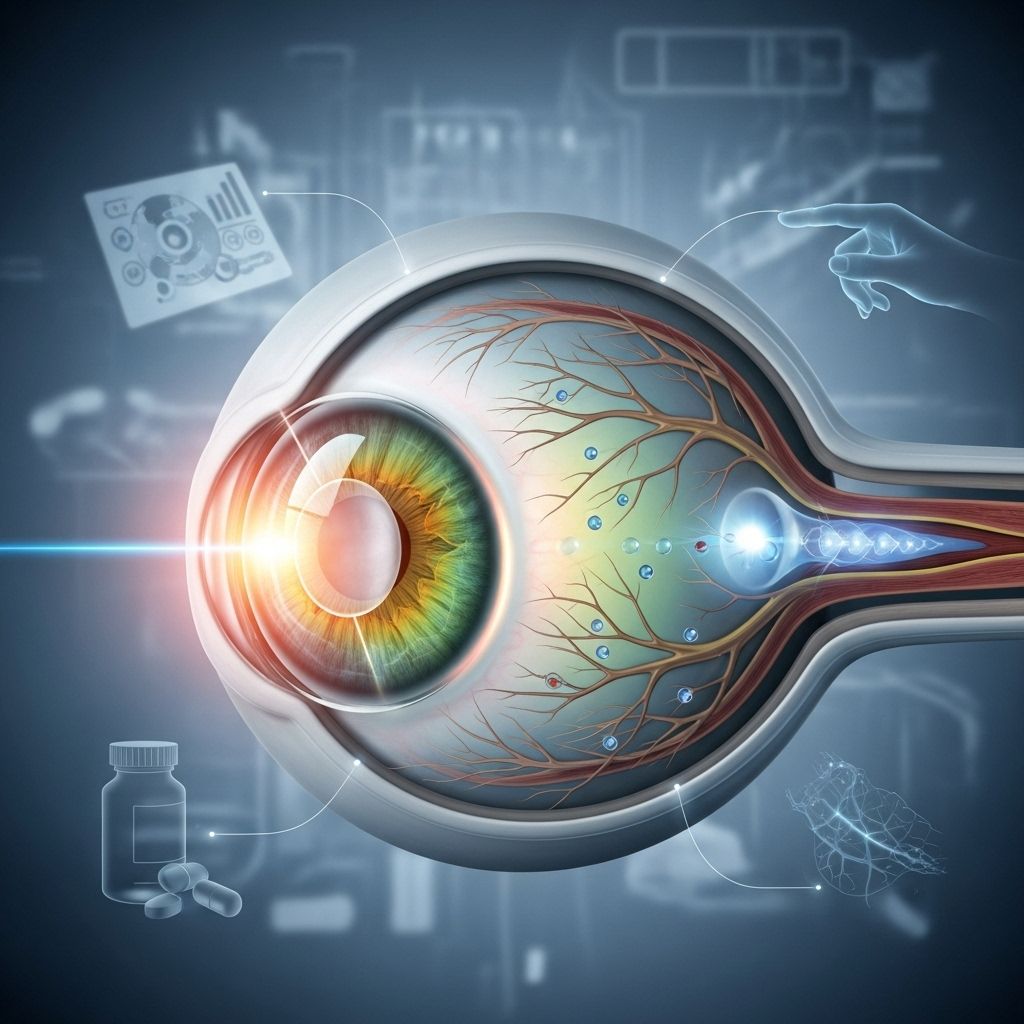
Cataract surgery is one of the most commonly performed procedures to restore vision, but for some, it can lead to complications such as glaucoma. Glaucoma is a group of eye conditions marked by damage to the optic nerve, often linked with increased intraocular pressure (IOP). This article explores the relationship between cataract surgery and subsequent glaucoma risk, with a focus on causes, risk factors, symptoms, diagnosis, management, and long-term outlook.
What Is Glaucoma?
Glaucoma refers to a category of eye disorders that can result in vision loss and blindness due to damage to the optic nerve, most frequently associated with elevated eye pressure. There are several types of glaucoma:
- Primary open-angle glaucoma: Most common; progressive and often symptom-free until late stages.
- Angle-closure glaucoma: Less common, but sudden and acute; requires immediate medical attention.
- Secondary glaucoma: Caused by other eye conditions or events, such as eye surgery.
For people who have undergone cataract surgery, secondary glaucoma is a key concern.
How Cataract Surgery Works
Cataracts cloud the eye’s natural lens, leading to blurred or diminished vision. During cataract surgery, the cloudy lens is removed and replaced with a clear artificial lens implant. The surgery is generally safe and can restore vision quickly, with most patients recovering within weeks (see ).
Link Between Cataract Surgery and Glaucoma
Although cataract surgery restores sight for most, it is associated with potential changes in the eye’s structure and pressure. These alterations can raise the risk of secondary glaucoma—a form of glaucoma triggered by factors other than genetics or longstanding disease.
- Short-term changes: Cataract surgery may transiently increase or decrease intraocular pressure.
- Long-term risks: Structural changes in the eye post-surgery may increase susceptibility to elevated IOP, especially in those who already have risk factors for glaucoma.
Pressure spikes are common in the days right after surgery and are usually managed with medicine, but some cases can lead to lasting pressure changes, contributing to optic nerve damage (see ).
Who Is at Risk?
Risk factors for developing glaucoma after cataract surgery include:
- History of glaucoma or ocular hypertension
- Advanced age
- Pediatric cataract surgery (children are at much higher risk for late-onset glaucoma, often decades after surgery) (see )
- Family history of glaucoma
- Complex or complicated cataract surgeries
- Other eye diseases (e.g., inflammation, diabetes)
According to recent studies, up to 47.7% of individuals who undergo cataract surgery in childhood may develop glaucoma or ocular hypertension by age 70 (see ).
Why Can Glaucoma Develop After Cataract Surgery?
Glaucoma after cataract surgery arises due to several mechanisms:
- Altered fluid drainage: Surgery can affect the trabecular meshwork (responsible for draining fluid) or block drainage pathways, causing pressure build-up.
- Inflammation: Post-surgery inflammation can raise IOP either temporarily or permanently.
- Lens particle or capsule remnants: Leftover lens material may provoke immune responses, clog drainage pathways, or cause scarring.
- Pre-existing risk: Those with borderline or elevated eye pressure prior to surgery are more susceptible.
Secondary glaucoma developing after surgery is often termed pseudophakic glaucoma (after lens implantation) or aphakic glaucoma (after lens removal only).
Signs and Symptoms of Glaucoma After Surgery
Glaucoma is sneaky: early stages are often symptom-free. Possible signs following surgery include:
- Blurred or progressively worsening vision
- Halos around lights
- Eye pain or headache (especially with angle-closure glaucoma)
- Redness or discomfort
- Nausea or vomiting (in acute angle-closure cases)
Since many people do not notice symptoms until damage is advanced, regular follow-up visits with eye pressure checks are crucial.
How Is Glaucoma Diagnosed After Cataract Surgery?
Diagnosis combines clinical tools and patient history:
- Tonometer measurement: Checks intraocular pressure.
- Optic nerve exam: Assesses for signs of damage.
- Visual field test: Maps peripheral vision loss.
- OCT scanning: Imaging for nerve fiber layers.
- Slit lamp exam: Looks for anatomical changes or inflammation.
A history of cataract surgery is important to mention, as it can influence the choice of diagnostic tests and interpretation.
Management and Treatment Options
If glaucoma is diagnosed after cataract surgery, management is tailored to the severity and underlying cause.
- Eye drops: The first-line therapy to lower intraocular pressure; multiple classes are available.
- Oral medications: Occasionally prescribed for more severe or resistant pressure elevations.
- Laser therapy: Laser trabeculoplasty may aid fluid outflow; laser procedures are also used to clear cloudy lens capsules if present (see ).
- Surgical intervention: Several types of glaucoma surgery can be performed, sometimes alongside additional cataract surgery or other repairs if applicable.
- Combined procedures: For those with both cataracts and glaucoma, doctors may recommend simultaneous surgery to address both conditions (see ).
| Surgery Type | Indications | Risks/Considerations |
|---|---|---|
| Laser Trabeculoplasty | Open-angle glaucoma, post-cataract surgery pressure rise | Temporary rise in pressure, irritation |
| Micro-invasive Glaucoma Surgery (MIGS) | Glaucoma plus cataract, mild to moderate cases | Lower risk, can combine with cataract surgery |
| Trabeculectomy | Advanced glaucoma with failed medical management | Infection, excessive pressure drop, scarring |
| Tube Shunt Surgery | Severe or complex glaucoma, prior surgery | Discomfort, infection risk |
Laser procedures, such as capsulotomy, may also be performed to clear any cloudy membrane left post-cataract operation, restoring vision without requiring further invasive surgery (see ).
Managing Medications and Vision
Glaucoma medications can impact vision in those with cataracts or artificial lenses:
- Adrenergic agonist drops (e.g., epinephrine): May increase glare by dilating the pupil, exposing the cataract or implant edge (see ).
- Miotic drops (e.g., pilocarpine): Shrink the pupil, further dimming vision in already cloudy eyes.
- No proven medicinal cure for cataracts: Cataracts can only be treated surgically; ongoing medication is directed at managing glaucoma.
Patients facing increased glare or reduced clarity should discuss alternative treatments with their eye doctors, including medicine adjustments, laser therapy, or even combined operations.
Prevention and Reducing Risk
While not all cases can be prevented, risks may be lowered by:
- Attending all scheduled follow-ups after cataract surgery.
- Reporting any vision changes, discomfort, or new symptoms quickly.
- Managing underlying health issues (diabetes, hypertension).
- Maintaining a healthy lifestyle to support eye health.
- Understanding family history risk and alerting your care team.
For pediatric cases, lifelong monitoring is essential, as glaucoma may not present until several decades post-surgery (see ).
Long-Term Outlook
Most people recover well from cataract surgery, but the possibility of glaucoma means vigilance is crucial. With early detection and effective management, vision loss can usually be minimized, but untreated or advanced glaucoma remains a leading cause of irreversible blindness.
Patients who underwent cataract surgery in childhood require lifelong eye care to monitor changes in pressure and optic nerve health. Adults should expect regular check-ups, especially if they have concurrent glaucoma or major risk factors (see ).
Modern surgical techniques, medications, and laser procedures have improved outcomes greatly, allowing many to retain functional vision for many years following surgery and treatment.
Frequently Asked Questions (FAQ)
Q: Can glaucoma develop immediately after cataract surgery?
A: Immediate pressure spikes can occur postoperatively but are often transient and manageable. Long-term glaucoma risk may depend on individual factors and the nature of the surgery.
Q: Are children more likely to get glaucoma after cataract surgery?
A: Yes, studies indicate children are at significantly higher risk for late-onset glaucoma following cataract removal and need lifelong monitoring (see ).
Q: Can both cataract and glaucoma surgeries be done together?
A: Yes. Combined surgeries (especially micro-invasive ones) are increasingly used for people with both conditions, improving recovery and vision outcomes (see ).
Q: How will my vision be after surgery?
A: Most regain clear vision post-cataract surgery unless glaucoma has caused extensive nerve damage. Ongoing monitoring is crucial for maintaining sight (see ).
Q: What symptoms should I watch for?
A: Blurred vision, eye pain, halos, headache, redness, or any unexplained visual changes warrant immediate medical attention for potential glaucoma.
Q: Is glaucoma preventable after cataract surgery?
A: No guaranteed prevention, but early detection and management reduce the risk of vision loss. Attending follow-up appointments is critical (see ).
Summary Table: Cataract Surgery vs Glaucoma
| Feature | Cataract Surgery | Glaucoma |
|---|---|---|
| Cause | Clouding of natural lens | Optic nerve damage, often due to eye pressure |
| Vision Changes | Blurred, dimmed; usually reversible | Peripheral loss, often irreversible without treatment |
| Treatment | Surgery replaces lens | Medications, laser, surgery to control pressure |
| Post-op Risk | Potential short-term pressure rise or drop, rare complications | May worsen if not recognized early after surgery |
Tips for Patients with Cataracts or Glaucoma
- Follow all post-surgical instructions carefully.
- Attend every follow-up visit; regular pressure checks are essential.
- Communicate any change in vision or symptoms immediately.
- Discuss all medications and possible side effects with your eye doctor.
- Maintain a healthy lifestyle: regular exercise, nutritious diet, and managed systemic diseases can help protect your sight.
Key Takeaways
- Glaucoma can develop after cataract surgery due to pressure changes or structural alterations.
- Pediatric cataract surgery patients face especially high long-term risk.
- Ongoing monitoring and early intervention are vital for preserving vision.
- Combined surgery for cataracts and glaucoma is increasingly available and effective.
Protecting your vision after cataract surgery requires informed follow-up and an open dialogue with your eye care team. Recognize risk factors, attend scheduled appointments, and act promptly for any visual disturbances.
References
- https://pubmed.ncbi.nlm.nih.gov/38233733/
- https://glaucoma.org/articles/cataracts-and-glaucoma
- https://glaucoma.responsumhealth.com/glaucoma-surgery-options
- https://www.morningtoneye.com.au/cataract-vs-glaucoma/
- https://www.healthline.com/health/eye-health/cataract-surgery-complications
- https://californiahealthline.org/news/article/eye-health-glaucoma-asking-never-hurts/
- https://sunexpresspharmacy.com/are-you-at-risk-of-glaucoma/
- https://armadale-eye.com.au/food-not-to-eat-after-cataract-surgery/
- https://www.medicalnewstoday.com/articles/157510
Read full bio of medha deb












