Geographic Atrophy: Progression, Symptoms, and Latest Treatments
Understand how geographic atrophy develops, how it affects vision, and the latest treatment options for this advanced eye condition.
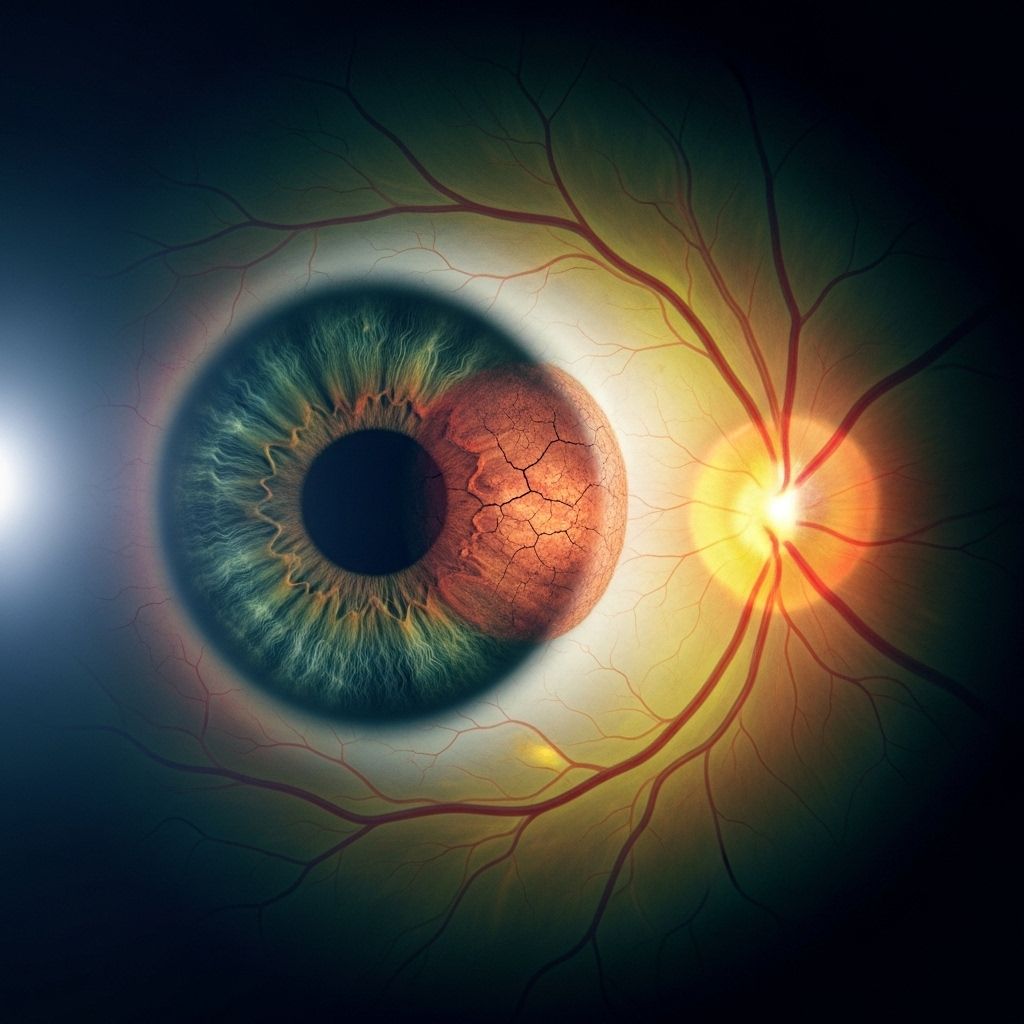
Geographic atrophy is a serious eye condition marked by permanent cell loss in the retina, leading to declining vision. As an advanced form of dry age-related macular degeneration (AMD), geographic atrophy (GA) affects millions worldwide, especially older adults. Understanding GA’s progression, its effects on daily life, and emerging treatments can empower patients to manage their health and preserve vision for as long as possible.
What Is Geographic Atrophy?
Geographic atrophy (GA) is the late, advanced stage of dry age-related macular degeneration (AMD). In GA, certain cells in the macula—the central part of the retina responsible for sharp, detailed vision—die off. When an ophthalmologist examines the retina, these areas of cell loss look like map-shaped patches, giving the condition its name.
- GA develops as irregular-shaped regions of atrophy, often first appearing near the fovea (the center of the macula responsible for your clearest vision).
- The damage often begins in the outer areas of the macula and gradually spreads toward the center.
- GA is considered a progressive and irreversible cause of vision loss.
How Geographic Atrophy Progresses
GA is a chronic, slowly worsening condition. While everyone’s experience is unique, researchers have identified general trends in how GA develops within the eye.
- It often stems from the accumulation of tiny fatty deposits called drusen in the macula.
- Initial cell loss usually occurs in the perifoveal (outer macula) area.
- As atrophy expands toward the fovea, central vision may be affected, resulting in more severe sight loss.
- The condition may affect only one eye initially, but often appears in both eyes over time.
- Progression rates vary, but once the fovea is involved, vision can decline rapidly.
The disease usually develops in these stages:
- Early AMD: Small drusen are present, but vision is mostly unaffected.
- Intermediate AMD: Larger drusen or pigment changes appear; patients may notice some vision difficulties, especially in low light.
- Late AMD (GA or Wet AMD): Either geographic atrophy (dry AMD) or neovascular (wet AMD) can occur. Wet and dry forms may sometimes coexist.
Causes and Risk Factors for Geographic Atrophy
While the exact cause isn’t known, several factors contribute to the development of GA:
- Advanced Age: The risk of GA increases significantly with age, affecting people primarily over 60.
- Genetics: Family history of AMD increases risk.
- Complement System Activation: Overactivation of the immune complement system can drive chronic inflammation and retinal cell death.
- Lifestyle: Smoking, high blood pressure, and poor diet increase AMD and GA risk.
- Other Factors: Light exposure, obesity, and certain cardiovascular conditions may also play a role.
GA typically results from ongoing damage related to AMD, and is rarely due to other conditions.
Symptoms and Signs of Geographic Atrophy
Symptoms of GA often develop gradually, making the condition difficult to notice at first. Key symptoms include:
- Difficulty reading or adapting to low light.
- Blurred or dim central vision—often with a gray or dark spot in the center.
- Increasing trouble recognizing faces.
- Decreased contrast sensitivity.
- Visual distortions—sometimes straight lines may appear wavy.
- Color vision changes.
Vision loss from GA is painless. In the early stages, the fovea may be spared. Central vision may remain normal until the atrophy reaches the fovea, at which point patients may notice more severe and sudden sight loss.
Diagnosis of Geographic Atrophy
Diagnosing GA involves a clinical eye examination and advanced imaging methods:
- Ophthalmoscopy: The eye doctor examines the retina for drusen and map-like atrophic areas.
- Fundus photography: Special images of the retina help track changes over time.
- Optical coherence tomography (OCT): Non-invasive, 3D imaging reveals the thickness and integrity of retinal layers, pinpointing atrophy.
- Fundus autofluorescence (FAF): Detects metabolic changes in retinal cells, highlighting areas of degeneration.
- Additional tests may rule out other retinal diseases.
The progression and spread of lesions, especially toward the fovea, can be closely monitored with these technologies.
Impact of Geographic Atrophy on Daily Life
GA can significantly alter a person’s independence and emotional well-being. As the disease advances, it disrupts everyday activities, such as:
- Reading books or newspapers.
- Driving—especially at night or in unfamiliar places.
- Using electronic devices.
- Recognizing faces of friends or loved ones.
- Performing household chores, cooking, or navigating new environments.
Individuals may find adaptation strategies necessary, including:
- Using brighter lighting and contrast-enhancing tools.
- Employing magnifiers or electronic reading aids.
- Seeking low-vision rehabilitation services for independent living.
- Relying on support from family or community resources.
Geographic Atrophy vs. Wet AMD
There are two forms of late-stage AMD:
| Feature | Geographic Atrophy (Dry AMD) | Wet AMD |
|---|---|---|
| Main Problem | Cell death (atrophy) in the retina | Abnormal leaky blood vessels |
| Vision Loss | Gradual, irreversible | May be rapid, sometimes reversible with early treatment |
| Symptoms | Dim or blurred central vision, scotomas | Distorted vision, sudden loss, dark areas |
| Occurrence | ~20% of AMD cases | ~80% of severe vision loss from AMD |
| Treatments | Limited; new drugs emerging | Anti-VEGF injections highly effective |
It’s possible to have both types in the same or both eyes.
Current and Emerging Treatments for Geographic Atrophy
Unlike wet AMD, which has several effective treatments, options for GA have historically been extremely limited. However, recent advances are offering new hope.
- Recently Approved Medications: The US FDA approved injections such as pegcetacoplan that help slow the progression of GA by decreasing the expansion rate of atrophic lesions.
- These drugs target complement pathways in the immune system to reduce chronic inflammation.
- Treatments are delivered via monthly or every-other-month intravitreal injections (injections into the eye).
- Research shows these medicines may work best if started before the atrophy reaches the fovea (extrafoveal atrophy).
There are no therapies currently available that restore lost vision or cure GA. Managing risk factors and closely monitoring disease progression remains critical.
Clinical Trials and Future Research
- Several investigational treatments, such as gene therapies and cell-based therapies, are in clinical trials.
- Ongoing research is seeking ways to better understand the disease mechanisms, slow progression, and preserve vision.
Coping With Geographic Atrophy: Tips and Support
Living with GA can be challenging, but these strategies can help minimize its impact:
- Regular Eye Exams: Ongoing monitoring to track progression, including testing for wet AMD development.
- Optimize Lighting: Increase brightness indoors, use task lights for reading.
- Magnification: Use handheld magnifiers, electronic readers, or large-print books.
- Low-Vision Rehabilitation: Engage with specialists who teach practical skills and adaptive techniques for independent living.
- Community Resources: Local and national vision organizations can help with social support, assistive devices, or legal matters.
- Healthy Lifestyle: Diet rich in leafy greens, omega-3s, and regular exercise may slow progression.
Frequently Asked Questions About Geographic Atrophy
What is the difference between geographic atrophy and AMD?
Geographic atrophy is a late-stage, advanced form of dry AMD. Not everyone with AMD develops GA, and not all vision loss from AMD is due to atrophy. GA refers specifically to well-defined patches of retinal cell death.
Does geographic atrophy always cause blindness?
GA leads to progressive, permanent central vision loss but does not typically cause total blindness, as peripheral vision is usually preserved. However, it can make daily activities very challenging if the central area is affected.
Are treatments available for geographic atrophy?
While no cure exists, new intravitreal injections like pegcetacoplan can slow progression. Early detection and intervention are key, and low-vision aids can help patients maintain independence.
Can lifestyle changes slow the progression of GA?
While lifestyle changes may not stop GA, not smoking, maintaining healthy blood pressure, eating a nutrient-rich diet, and protecting eyes from excessive sunlight may support overall eye health.
How often should I see my eye doctor if I have geographic atrophy?
Routine checkups every 6 to 12 months are recommended for those with GA, possibly more frequently if symptoms change or if wet AMD develops.
Resources and Support
- Macular Society: Offers advice, support, and helplines for those affected by macular disease.
- Vision Loss Support Groups: Find local and national organizations that address adaptation, devices, and education for low-vision living.
- Retinal Specialists: Seek care from ophthalmologists experienced in retinal disease management and the latest clinical trials.
Takeaway
Geographic atrophy is a common, advanced form of dry age-related macular degeneration that leads to gradual, permanent vision loss. It typically starts in the outer central retina and advances toward the fovea, affecting daily activities and quality of life. Regular monitoring, adaptive strategies, and exciting new therapies provide hope for those with GA. Partnering with eye care professionals and support organizations can help maximize remaining vision, maintain independence, and improve quality of life.
References
- https://www.macularsociety.org/macular-disease/macular-conditions/dry-age-related-macular-degeneration/geographic-atrophy/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10408405/
- https://eyewiki.org/Geographic_Atrophy
- https://preventblindness.org/geographic-atrophy/
- https://my.clevelandclinic.org/health/diseases/24890-geographic-atrophy
- https://www.prevention.com/health/health-conditions/a64747557/one-familys-journey-with-geographic-atrophy/
- https://www.southeasternretina.com/blog/geographic-atrophy-symptoms-what-to-watch-for-in-late-stage-amd
- https://www.brightfocus.org/resource/geographic-atrophy-fact-sheet/
- https://www.mdfoundation.com.au/about-macular-disease/age-related-macular-degeneration/geographic-atrophy-dryamd/
Read full bio of medha deb












