Understanding Geographic Atrophy: Causes, Risks, and Management
Explore the stages, risk factors, symptoms, and latest treatments for geographic atrophy, an advanced form of dry macular degeneration.
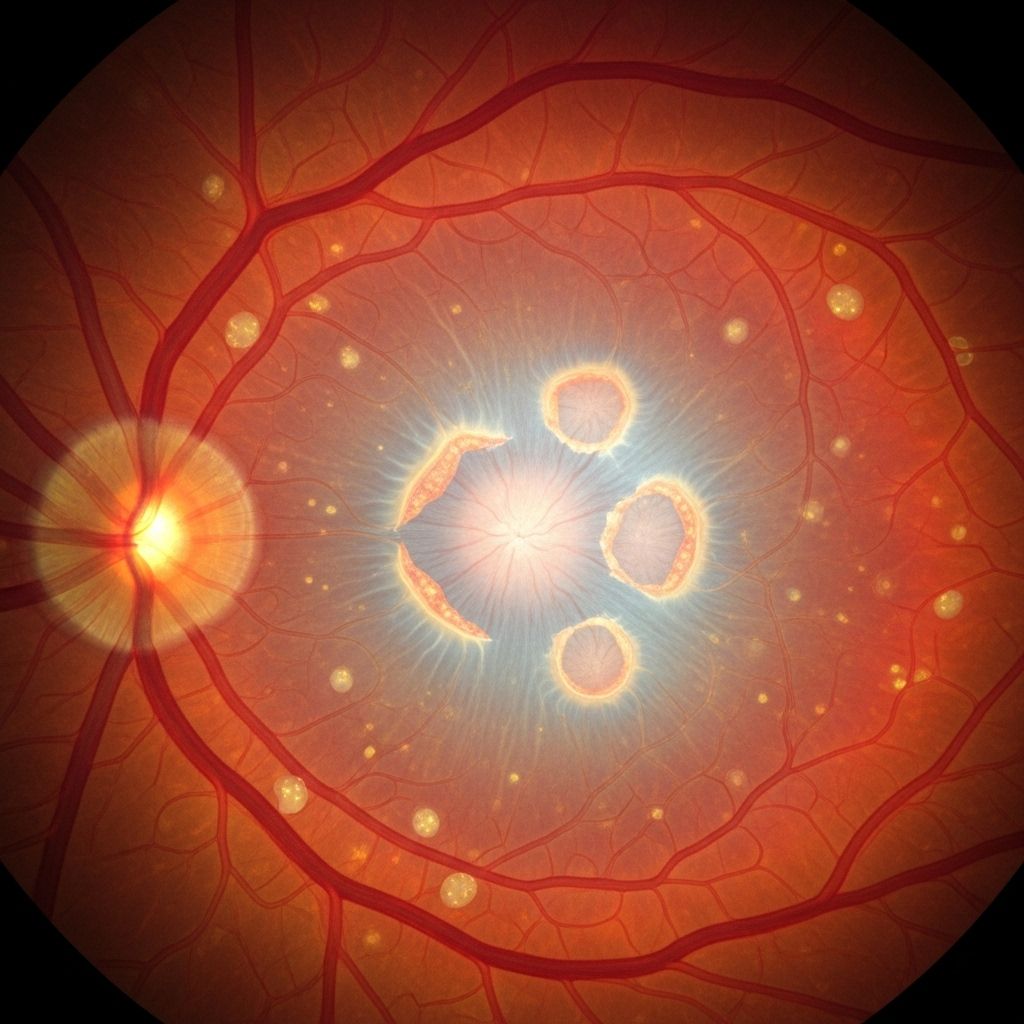
Geographic atrophy (GA) is a late-stage, advanced form of age-related macular degeneration (AMD) that results in irreversible vision loss for millions of people worldwide. Characterized by the progressive loss of key retinal cells, GA leads to sharply demarcated areas of vision loss that expand over time. This article explores the stages, symptoms, risk factors, diagnostic process, prognosis, and emerging therapies for geographic atrophy.
What Is Geographic Atrophy?
Geographic atrophy is a chronic, progressive degeneration of the macula, a central part of the retina responsible for sharp, straight-ahead vision. As the disease progresses, retinal cells and supporting tissues die off, resulting in patches of tissue loss (atrophy) that appear as distinct lesions during eye exams. These areas resemble the outlines of islands on a map, which is why the term “geographic” is used.
- GA is a form of late-stage dry AMD, as opposed to wet (neovascular) AMD, which involves abnormal blood vessel growth.
- GA causes irreversible vision loss as lesions expand, especially when they reach the central macula (fovea).
- The disease can affect one or both eyes; if present in one, the risk is higher in the other.
Stages and Progression of AMD and GA
Age-related macular degeneration is a progressive disease with distinct stages. Not every patient with AMD progresses to geographic atrophy, but understanding the continuum helps clarify the impact of GA:
| Stage | Key Features | Impact on Vision |
|---|---|---|
| Early AMD | Small deposits (drusen) under the retina; often found during routine eye checks. | Usually no noticeable symptoms. |
| Intermediate AMD | Bigger/more drusen; possible pigment changes in the macula. | Some people may have minor difficulties with low-light conditions. |
| Late AMD (Geographic Atrophy) | Patches of cell death (atrophy) expand gradually, usually starting outside the fovea. | Progressive, irreversible loss of central visual field. |
| Late AMD (Wet AMD) | Abnormal blood vessel growth, bleeding, and leaking. | Rapid, severe, and sometimes sudden vision loss. |
Geographic atrophy and wet AMD represent two advanced forms of the disease. They may occur separately or even coexist in the same eye. GA typically develops slowly but accelerates as it encroaches on the central macular region.
Causes and Pathophysiology of Geographic Atrophy
The exact mechanisms underlying GA are complex and not fully understood. Several interrelated processes contribute to its development:
- Chronic inflammation: Overactivation of the complement system leads to an ongoing inflammatory response within the retina, damaging essential retinal cells.
- Cellular degeneration: Key structures affected are the photoreceptors (light-sensing cells), the retinal pigment epithelium (RPE, supporting cell layer), and the choriocapillaris (tiny blood vessels beneath the retina).
- Genetic susceptibility: Variants in genes regulating inflammation, tissue repair, and metabolism can elevate risk.
- Oxidative stress: Accumulated cellular damage from oxidative byproducts can weaken and kill retinal cells over time.
As the retinal pigment epithelium and overlying photoreceptors die, sharply defined lesions develop. These lesions are visible in eye imaging, marking the areas of vision that will not recover.
Symptoms of Geographic Atrophy
Geographic atrophy causes a variety of visual symptoms, most of which worsen as the disease progresses. Early symptoms can be subtle and may overlap with those of less advanced AMD, making regular eye exams crucial for early identification.
- Blurry or distorted central vision
- Difficulty reading, especially small print
- Trouble recognizing faces
- Missing letters or parts of words during reading
- Blind spots (scotomas) in the central visual field
- Poor adaptation to low light or transitions from light to dark
As GA lesions enlarge and approach the fovea, central vision becomes increasingly impaired. Peripheral vision is typically retained, but tasks requiring sharp focus become challenging.
Who Is at Risk?
Several well-established and emerging factors raise the likelihood of developing geographic atrophy. These include:
- Age: The risk increases sharply after age 60. Most GA cases develop in individuals older than 70.
- Family history: Those with a parent or sibling diagnosed with AMD are at increased genetic risk.
- Genetic mutations: Certain gene variants (esp. in complement pathway genes such as CFH, C3) are associated with higher risk of progression to GA.
- Smoking: Strongly associated with both developing AMD and progression to GA.
- Race/ethnicity: AMD, and therefore GA, is somewhat more common among people of European descent.
- Cardiovascular health: High blood pressure, high cholesterol, and cardiovascular disease may contribute to disease progression.
- Obesity and diet: Poor nutrition (esp. low in leafy greens and antioxidant vitamins) and obesity increase the risk.
- Other factors: Long-term exposure to ultraviolet (UV) light, low exercise levels, and high levels of blue light exposure from screens may play supporting roles, though evidence is mixed.
Although anyone can theoretically develop GA, a combination of these risk factors—especially advanced age, family history, and smoking—substantially increases likelihood.
Diagnosis of Geographic Atrophy
Early diagnosis of geographic atrophy is key to optimizing management. GA cannot be self-diagnosed at home; diagnosis requires a comprehensive eye exam with a qualified optometrist or ophthalmologist.
- Visual acuity testing assesses overall central vision.
- Dilated eye exams allow direct visualization of the retina using specialized equipment.
- Imaging tests include fundus autofluorescence (FAF), optical coherence tomography (OCT), and sometimes fluorescein angiography. These show characteristic atrophic lesions and help monitor disease over time.
GA lesions can be seen as sharply demarcated, pale or yellow patches on the macula, sometimes with clear borders and atrophy that starts away from but eventually involves the central fovea.
Impact on Vision and Daily Life
Geographic atrophy can significantly impair key aspects of independent living and quality of life, especially as the central vision deteriorates:
- Reading: Increasing difficulty with small print, even with glasses or magnification.
- Driving: Reduced ability to see road signs, pedestrians, and hazards – eventually making driving unsafe and inadvisable.
- Recognizing faces: Central blind spots hinder identification, which can affect social interactions.
- Performing household tasks: Diminished fine vision makes activities like cooking, sewing, and using appliances challenging.
- Watching television or screens: Visual details may be lost or missing, significantly reducing enjoyment.
- Low-light navigation: Vision impairment in low illumination or glare can increase fall and accident risk.
Peripheral vision generally remains functional, but loss of central vision may lead to legal blindness even if some ability to see around the edges is preserved. The psychological impact, including loss of independence and increased risk of depression, should not be underestimated.
Prognosis: How Fast Does Geographic Atrophy Progress?
The progression of GA varies widely between individuals. Typically, lesions start outside the fovea and encroach on this vital central region over time. Once the fovea is involved, vision loss can accelerate.
- Lesion growth rate: Most lesions grow slowly at first, with median time from non-foveal to foveal involvement of 1.4 to 2.5 years, but this can vary.
- Functional impact: Even before foveal involvement, vision loss can interfere with daily life, especially at near and intermediate distances.
- Later stages: Expansion and merging of lesions may lead to nearly complete central vision loss over several years.
Can Geographic Atrophy Be Prevented?
While there is no proven way to fully prevent GA, certain strategies may lower the risk of developing AMD or slow progression in those already diagnosed.
- Don’t smoke: Smoking is the most significant modifiable risk factor for progression.
- Maintain a balanced diet: Diets high in leafy greens, colorful vegetables, healthy fats, and omega-3 fatty acids are associated with lower risk.
- Take prescribed supplements: For people with intermediate or advanced AMD, AREDS/AREDS2 supplements (with antioxidants and zinc) may slow progression.
- Manage health conditions: Controlling blood pressure, cholesterol, and cardiovascular disease lowers risk.
- Protect eyes from UV and blue light: Wear sunglasses and limit excessive screen time.
- Regular eye exams: Early detection allows for monitoring and emerging treatment options.
Current and Emerging Treatments
Until recently, there were no approved treatments for slowing or reversing geographic atrophy. However, new therapies are starting to change the landscape:
- Intravitreal injections: The FDA has recently approved drugs targeting the complement pathway, such as pegcetacoplan and avacincaptad pegol, for GA secondary to AMD. These drugs may slow the spread of atrophy, especially when started before the fovea is affected.
- Frequency: Most patients require monthly or every-other-month injections delivered directly into the eye.
- Effectiveness: Greatest benefits seen in patients with atrophy away from the fovea (extrafoveal involvement), preserving central vision longer.
Supportive strategies include:
- Vision rehabilitation—techniques and training to maximize remaining vision.
- Use of magnifying devices, electronic readers, and adaptive technologies.
- Community and psychological support to address the impact of vision loss.
Ongoing Research
Researchers are investigating:
- Additional drug candidates targeting inflammation and cell survival pathways.
- Stem cell therapies to replace damaged retinal pigment epithelium.
- Gene therapies aiming to address underlying genetic causes.
Living With Geographic Atrophy
A diagnosis of geographic atrophy can feel overwhelming, but many people maintain independence and quality of life by combining medical strategies with adaptive approaches. Helpful tips include:
- Enrolling in vision rehabilitation programs to learn adaptive techniques.
- Using high-contrast, large-print materials, and good lighting when reading or doing detailed work.
- Seeking counseling or support groups for coping and mental health care.
- Discussing driving safety regularly with an eye care provider.
- Engaging with loved ones and staying active to prevent social isolation.
Frequently Asked Questions (FAQs)
What is the difference between geographic atrophy and wet AMD?
Geographic atrophy is a late-stage form of dry AMD, involving gradual loss of retinal cells. Wet AMD involves rapid, abnormal blood vessel growth and leakage below the retina that leads to sudden and sometimes severe vision changes. Both can coexist in the same eye, but their management and progression differ.
Can geographic atrophy cause complete blindness?
GA causes loss of central vision, which is crucial for most daily activities. Total blindness is rare because peripheral vision is typically preserved, but the impact on quality of life can be profound.
Are there treatments that can restore lost vision in GA?
No treatments are currently available to restore areas of vision lost to GA. Newly emerging drugs can slow further progression but cannot reverse existing damage. Vision rehabilitation can help people maximize the vision that remains.
How often should people with AMD or GA have their eyes examined?
Patients with AMD or GA should have comprehensive eye exams as recommended by their eye doctor, typically every 6–12 months, or sooner if vision changes are noticed.
Can healthy lifestyle choices help with geographic atrophy?
Yes. Not smoking, maintaining good nutrition, protecting eyes from UV exposure, managing chronic health conditions, and regular exercise are all associated with reduced risk of developing or worsening AMD and GA.
When to Seek Medical Advice
Prompt eye evaluation is crucial if you notice:
- Sudden change or worsening in central vision
- Difficulty seeing in low light that develops rapidly
- New or enlarging blind spots
- Visual distortions, such as straight lines appearing wavy
Early diagnosis and monitoring can help preserve independence and allow timely access to new treatment options as they become available.
Takeaway
Geographic atrophy is a serious, progressive eye disease affecting millions of older adults. The landscape of treatment and research is rapidly evolving, offering new hope to patients and families. Healthy lifestyle choices, regular eye care, and access to specialized support resources remain vital for managing risk and maintaining quality of life.
References
- https://www.macularsociety.org/macular-disease/macular-conditions/dry-age-related-macular-degeneration/geographic-atrophy/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10408405/
- https://www.macular.org/about-macular-degeneration/geographic-atrophy
- https://eyewiki.org/Geographic_Atrophy
- https://www.brightfocus.org/resource/what-is-geographic-atrophy/
- https://my.clevelandclinic.org/health/diseases/24890-geographic-atrophy
- https://www.southeasternretina.com/blog/geographic-atrophy-symptoms-what-to-watch-for-in-late-stage-amd
- https://preventblindness.org/geographic-atrophy/
Read full bio of Sneha Tete












