Genital Herpes: Causes, Symptoms, Diagnosis, and Treatment
Genital herpes affects millions and understanding its transmission, symptoms, and management is crucial for prevention and care.
Genital Herpes: Overview and Key Facts
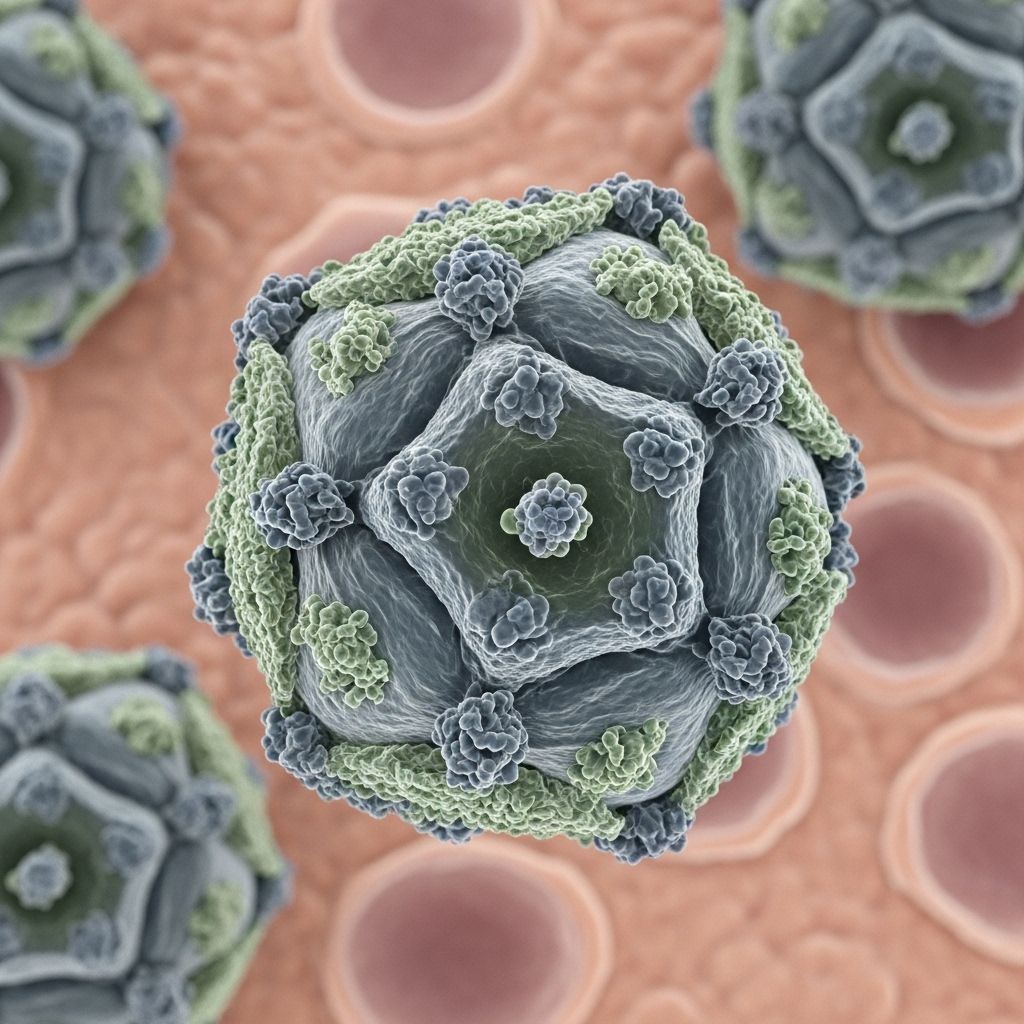
Genital herpes is a common sexually transmitted disease (STD) primarily caused by two closely related viruses in the herpesvirus family: herpes simplex virus type 1 (HSV-1) and herpes simplex virus type 2 (HSV-2). While HSV-2 remains the leading cause of genital herpes worldwide, HSV-1, traditionally known for oral herpes, increasingly contributes to genital infections, especially in developed nations.
Both viruses persist for a lifetime within the body, leading to recurrent outbreaks and posing significant health challenges. Understanding genital herpes involves recognizing its transmission, symptoms, diagnostic processes, potential complications, and treatment or prevention strategies.
What Is Genital Herpes?
Genital herpes is a viral infection that manifests as outbreaks of painful sores, blisters, or ulcers on or near the genitals, rectum, or mouth. After initial infection, the virus remains dormant within the nerve cells, periodically reactivating and causing symptoms throughout the patient’s life.
Key facts about genital herpes:
- Caused mainly by HSV-2, but HSV-1 also contributes to cases through oral-genital contact.
- Highly prevalent globally, affecting millions of sexually active individuals of all backgrounds.
- Cannot be cured, but symptoms are manageable and outbreaks can often be reduced with antiviral medications.
How Common Is Genital Herpes?
Genital herpes ranks among the most widespread STDs across the globe. The World Health Organization estimates that:
- HSV-2 affects about 491 million people aged 15-49 worldwide, roughly 13% of this age group.
- HSV-1 infects about 3.7 billion people under 50, with an increasing proportion causing genital symptoms.
- Women have a higher seropositivity rate for HSV-2 than men.
- In the United States, genital herpes is among the most frequently reported sexually transmitted diseases.
What Causes Genital Herpes?
Genital herpes is caused by infection with:
- Herpes simplex virus type 2 (HSV-2): Primarily spreads via genital-to-genital contact during vaginal, anal, or oral sex.
- Herpes simplex virus type 1 (HSV-1): More commonly associated with oral herpes but can infect the genital area, especially through oral-genital contact.
After exposure, the virus invades epithelial cells and travels to nearby nerve ganglia, establishing a dormant (latent) infection. Reactivation leads to periodic shedding and symptomatic outbreaks. Triggers for reactivation may include stress, illness, ultraviolet light exposure, or immunosuppression.
How Does Genital Herpes Spread?
Genital herpes is transmitted primarily through direct skin-to-skin contact during sexual activity. This includes:
- Vaginal, anal, and oral sex with an infected partner
- Contact with infected sores, genital secretions, or mucous membranes—transmission can occur even when symptoms are absent
Because both HSV-1 and HSV-2 may be shed from the skin or mucosa without visible lesions (asymptomatic shedding), infection can occur even when a partner displays no signs of active disease.
Key risk factors for genital herpes transmission:
- Multiple sexual partners
- Previous or existing sexually transmitted infections
- First sexual activity at an early age
- Immunocompromised status (e.g., HIV infection, organ transplantation, cancer therapy)
Signs and Symptoms: What Are the Symptoms of Genital Herpes?
Symptoms can vary widely—with some individuals experiencing significant discomfort during outbreaks, while others remain asymptomatic. After the initial (primary) infection, recurrent episodes are usually less severe.
Primary Infection Symptoms:
- Painful genital ulcers or blisters
- Itching, burning, redness or tingling in affected area
- Flu-like symptoms (fever, muscle aches, swollen lymph nodes)
- Difficulty urinating (rare)
Progression of Lesions:
- Lesions typically begin as small papules and macules
- Evolve to form vesicles and pustules, which rupture and become shallow ulcers
- Crusting and healing occur within several days to weeks
Recurrent Outbreaks:
- Similar lesions, usually milder and shorter in duration
- Outbreaks may be triggered by stress, illness, menstruation, or other factors
- Many infected individuals have only mild or unnoticeable recurrences
Gender Differences:
- Women may have more frequent outbreaks and are more likely to develop ulcers than men
- Men tend to experience longer-lasting vesicular phases when affected
Who Is at Risk for Genital Herpes?
Anyone engaging in sexual activity with an infected partner can contract genital herpes. There is no cure; the virus remains in the body for life, often reactivating intermittently. People at highest risk include:
- Individuals with multiple sexual partners or new partners
- Women (higher susceptibility)
- Those with compromised immune function
Having genital herpes increases the risk of other sexually transmitted diseases like HIV. Ulcers and inflammation in the genital region facilitate HIV entry and transmission.
Complications Associated With Genital Herpes
While many cases are mild and manageable, genital herpes can lead to significant complications in specific populations:
- Neonatal herpes: Can result when a baby is exposed to HSV during childbirth. It can cause severe, potentially fatal disease in newborns and is a major concern for pregnant women with active genital herpes.
- Severe disease in immunocompromised patients: Individuals with weakened immune systems may experience extensive, long-lasting outbreaks or dangerous complications such as encephalitis (brain infection) or disseminated infection.
- Increased HIV transmission: Genital ulcers associated with herpes facilitate HIV acquisition and transmission during sexual activity.
- Social and psychological impacts: Anxiety, depression, relationship stress, and stigma can negatively affect affected individuals.
Diagnosis: How Is Genital Herpes Diagnosed?
A healthcare provider typically diagnoses genital herpes based on clinical symptoms and may confirm the infection through laboratory tests. Key steps include:
- Physical examination: Visual inspection for characteristic lesions in the genital or anal areas
- Swab tests: Sample of blister fluid or ulcer base for direct detection of viral DNA (PCR) or viral culture
- Blood tests: Serologic testing for HSV-1 and HSV-2 antibodies, useful if symptoms are absent but risk or exposure is suspected
Laboratory confirmation helps distinguish between HSV-1 and HSV-2 and guides treatment planning and counseling.
Treatment: How Is Genital Herpes Treated?
There is no cure for genital herpes, but antiviral medications effectively manage symptoms, reduce the frequency of outbreaks, and lower the risk of transmission.
Main classes of antiviral medications:
- Acyclovir
- Famciclovir
- Valacyclovir
These medications are most effective when started early during an outbreak and can be prescribed for either acute outbreak management or as suppressive therapy to minimize recurrent episodes and reduce asymptomatic viral shedding.
Other Management Strategies:
- Pain relief with topical or oral agents
- Warm baths or compresses for comfort
- Good hygiene to prevent secondary infections
Prevention Tips:
- Consistent condom use significantly reduces but does not eliminate transmission risk
- Avoid sexual contact during outbreaks or when symptoms are present
- Inform sexual partners about infection; they should be aware of risk and prevention strategies
- Pregnant women should discuss herpes history and exposure risk with their health provider to manage risk to the newborn
Can Genital Herpes Be Prevented?
Prevention strategies center around reducing exposure and transmission:
- Practicing protected sex and regular STI testing
- Communicating openly with sexual partners
- Suppressive therapy for infected individuals with frequent outbreaks or those in discordant relationships
Research for a herpes vaccine is ongoing, with no approved vaccine yet available, though promising candidates are currently in clinical trials.
Living With Genital Herpes
For most, genital herpes is a manageable, though chronic, condition. Recurrences typically decline in frequency and severity over time. With proper care and open communication, affected individuals can maintain healthy relationships and high quality of life.
Emotional Health and Support
- Joining support groups for individuals living with herpes can help manage trauma, anxiety, and stigma.
- Close communication with partners and healthcare professionals is critical.
Frequently Asked Questions (FAQs)
Q: Can I get genital herpes without having sex?
A: While genital herpes most commonly spreads through sexual activity, transmission can occur through other forms of skin-to-skin contact with infected areas or secretions. However, such cases are rare.
Q: Does genital herpes mean I’m more likely to get HIV?
A: Yes, the presence of genital ulcers and inflammation caused by herpes increases susceptibility to HIV if exposed.
Q: Is there any cure for genital herpes?
A: No, there is currently no cure. Antiviral medications manage symptoms, decrease outbreak frequency, and reduce transmission risk.
Q: What can trigger a herpes outbreak?
A: Common triggers include stress, illness, injury, menstruation, and immunosuppression.
Q: How do I protect my partner from genital herpes?
A: Use condoms, avoid sexual activity during outbreaks, and consider daily suppressive therapy if advised by your healthcare provider.
Comparison Table: HSV-1 vs HSV-2 Infection
| Feature | HSV-1 | HSV-2 |
|---|---|---|
| Primary Location | Mouth, lips (oral herpes); can affect genitals | Genitals (genital herpes) |
| Transmission | Oral-to-oral, oral-genital | Genital-to-genital, genital-oral, genital-anal |
| Recurrence Rate (Genital) | Less frequent | More frequent |
| Common Age of Infection | Childhood | Adolescence/adulthood |
| Global Prevalence | ~67% under 50 years | ~13% ages 15–49 |
Key Takeaways
- Genital herpes is a lifelong viral infection caused by HSV-1 or HSV-2.
- Most infected individuals have no symptoms or infrequent mild recurrences, but outbreaks can cause significant discomfort and emotional distress.
- Diagnosis is straightforward with clinical evaluation and lab testing.
- Effective management includes antiviral medications and safe sex practices.
- Ongoing research aims to produce effective vaccines and new therapies for herpes prevention and treatment.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9966607/
- https://pure.johnshopkins.edu/en/publications/herpes-simplex-virus-infection-as-a-risk-factor-for-human-immunod-4
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10675801/
- https://www.hopkinsguides.com/hopkins/view/Johns_Hopkins_HIV_Guide/545092/all/Herpes_simplex
- https://www.hopkinsguides.com/hopkins/view/Johns_Hopkins_ABX_Guide/540242/all/Herpes_Simplex_Virus
Read full bio of Sneha Tete












