Genetic Abnormalities in Chronic Myeloid Leukemia: Causes, Signs, and Understanding CML
Explore the genetic roots, key symptoms, and critical facts about chronic myeloid leukemia and the abnormality causing CML.
Chronic myeloid leukemia (CML) is a complex blood cancer largely defined by a distinctive genetic abnormality. This article explores what triggers CML at the molecular level, how those changes lead to the disease, what symptoms and signs to watch for, and answers common questions about chronic myeloid leukemia. Our aim is to provide a comprehensive, up-to-date overview, drawing on expert knowledge and current research to aid understanding for both patients and families.
What Is Chronic Myeloid Leukemia (CML)?
CML is a type of blood cancer that affects the bone marrow and blood. It is called ‘chronic’ because it typically develops slowly over months or years. The disease primarily arises from changes in the genetic material of blood-forming cells, which disrupts normal blood cell production and leads to a buildup of abnormal white blood cells. Crucially, CML is linked to a characteristic genetic defect known as the Philadelphia chromosome.
What Genetic Abnormality Causes CML?
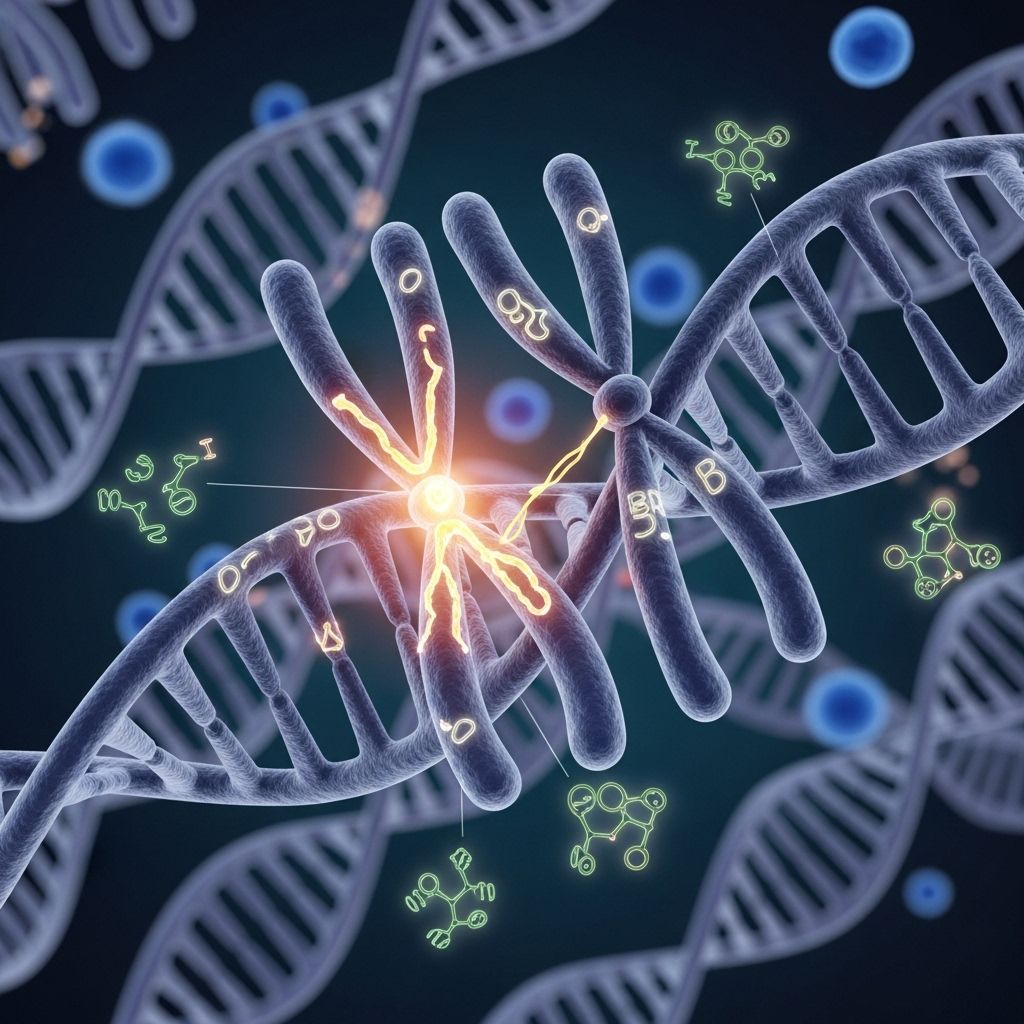
The main cause of CML is a specific genetic alteration called the Philadelphia chromosome (Ph chromosome). This abnormality is formed when segments from two chromosomes — chromosome 9 and chromosome 22 — swap places, a process known as translocation. The resulting change is referred to as t(9;22)(q34;q11).
- Philadelphia chromosome: Chromosome 22 becomes abnormally shortened due to an exchange with a part of chromosome 9.
- BCR-ABL1 fusion gene: This new segment on chromosome 22 creates an abnormal gene by combining parts of two genes: BCR from chromosome 22 and ABL1 from chromosome 9.
The result is the BCR-ABL1 fusion gene, which produces an abnormal tyrosine kinase enzyme. This enzyme sends continuous signals telling cells to grow and divide uncontrollably, which is at the heart of CML development.
How the Philadelphia Chromosome Forms
- Translocation between chromosomes 9 and 22 occurs in one blood-forming cell in the bone marrow.
- The abnormal chromosome 22 (Ph chromosome) carries the BCR-ABL1 fusion gene.
- This cell multiplies, creating a large population of cells with the same genetic change.
- These abnormal cells crowd out normal blood cells in the bone marrow and bloodstream.
Why Does This Genetic Abnormality Happen?
Scientists do not fully understand what causes the initial translocation that creates the Philadelphia chromosome. It occurs spontaneously and is not inherited. There are several important points to note:
- Not passed from parent to child: The genetic change occurs after birth and is confined to the affected person’s blood-forming cells.
- Environmental causes: Exposure to very high doses of ionizing radiation increases the risk but otherwise no clear environmental or lifestyle factor is known to directly cause this genetic change.
- Random event: In the majority of cases, the change arises randomly during cell division in bone marrow stem cells.
How Does CML Develop?
The BCR-ABL1 fusion protein acts like an overactive ‘on’ switch for cell growth. This leads to the uncontrolled production of abnormal white blood cells called granulocytes. These cells build up in the blood and bone marrow, crowding out healthy cells and disrupting normal blood production. Over time, this process can result in the various symptoms and complications of CML.
| Step | Description |
|---|---|
| Translocation | DNA segments switch between chromosomes 9 and 22. |
| BCR-ABL1 Fusion | New gene forms on abnormal chromosome 22. |
| Abnormal Tyrosine Kinase | Fusion gene creates a protein that accelerates cell growth. |
| Leukemic Cell Growth | Uncontrolled division leads to accumulation of abnormal white blood cells. |
What Are the Symptoms and Signs of CML?
Many people with CML have no symptoms in the early stages and the condition is often found by chance during routine blood tests. When present, symptoms typically develop gradually and are often vague or mild at first. They can become more pronounced as the disease progresses.
- Fatigue and weakness: Often due to anemia resulting from fewer healthy red blood cells.
- Night sweats and fever: An increased number of abnormal white cells can trigger fever and profuse sweating, especially at night.
- Unexplained weight loss: Body’s energy resources are used up fighting the disease or due to loss of appetite.
- Bone pain: The excessive growth of abnormal cells can expand marrow and cause pain or aches in bones and joints.
- Enlarged spleen (splenomegaly): Spleen may become enlarged as it works to filter abnormal cells, causing dull pain or fullness under the left ribs.
- Fullness or abdominal discomfort: Enlargement of the spleen can press against the stomach, leading to a sense of fullness or decreased appetite.
- Frequent infections: Abnormal white blood cells are ineffective at fighting infection, leading to increased risk.
- Bruising or bleeding easily: Low platelet count can result in frequent nosebleeds, bleeding gums, or easy bruising.
Symptoms are not always present and may mimic those of other less serious illnesses, underlining the importance of regular checkups and blood testing.
Common Signs Detected by Doctors
- Leukopenia: Low number of healthy white blood cells.
- Anemia: Low red blood cell count, contributing to fatigue and pallor.
- Neutropenia: Low neutrophil count, raising infection risk.
- Thrombocytopenia: Low platelet count, causing bleeding problems.
- Thrombocytosis: Some patients may have too many, but dysfunctional, platelets.
How Is CML Diagnosed?
CML is most often discovered during routine or unrelated blood tests. If CML is suspected, several diagnostic steps are followed:
- Complete blood count (CBC): May show high white cell counts, anemia, or abnormal platelets.
- Bone marrow biopsy: Examines marrow cells and determines the degree of abnormal cell proliferation.
- Cytogenetic analysis: Looks specifically for the Philadelphia chromosome and BCR-ABL1 fusion gene, confirming CML diagnosis.
Detecting the Philadelphia chromosome is essential to distinguish CML from other forms of leukemia and to guide treatment decisions.
Who Is at Risk for Developing CML?
CML is considered rare. It can affect people of any age but is most common in adults, particularly those over age 60. Some risk factors include:
- Age: Risk increases with age.
- Gender: Males are slightly more affected than females.
- Exposure to high-dose radiation: Rare, but those exposed (such as nuclear accident survivors) have a higher risk.
However, in the vast majority of cases, CML arises without any identifiable risk factor.
How Is CML Treated?
The discovery of the Philadelphia chromosome and its role in CML directly led to targeted therapies that have dramatically improved patient outcomes. Treatment options include:
- Tyrosine kinase inhibitors (TKIs): Drugs like imatinib, dasatinib, and nilotinib specifically block the abnormal BCR-ABL1 enzyme, slowing or stopping the growth of leukemic cells.
- Stem cell transplantation: In some cases, a bone marrow or stem cell transplant may be recommended.
- Supportive treatments: These include antibiotics for infection, blood transfusions for anemia, and medications to manage symptoms.
Most patients respond well to TKIs, allowing many to live a near-normal lifespan with proper medical care and ongoing monitoring.
Frequently Asked Questions (FAQs) About CML
Q: What is the Philadelphia chromosome and how does it cause CML?
A: The Philadelphia chromosome is an abnormal chromosome 22 created by a translocation with chromosome 9. This change leads to the BCR-ABL1 fusion gene, which makes a signaling protein that drives uncontrolled cell growth and causes CML.
Q: Is CML inherited from parents?
A: No, the genetic abnormality in CML develops after birth and is not passed from parent to child. Most cases arise from a random error during cell division.
Q: What early symptoms should I watch for?
A: Early CML may not cause symptoms, but key warning signs include persistent fatigue, unexplained weight loss, night sweats, pain or fullness below the left ribs, frequent infections, and easy bruising or bleeding.
Q: Can environmental factors like chemicals or lifestyle cause CML?
A: The only strongly established environmental risk factor for CML is exposure to high doses of ionizing radiation. Other factors, such as diet or chemical exposures, have not been clearly linked to CML development.
Q: How effective are today’s treatments for CML?
A: Modern treatments, particularly tyrosine kinase inhibitors, allow most CML patients to maintain excellent long-term control of the disease, often with few symptoms and normal life expectancy.
Key Facts and Takeaways
- CML is caused by a genetic translocation that creates the Philadelphia chromosome and BCR-ABL1 fusion gene.
- The resulting abnormal protein triggers uncontrolled growth of white blood cells.
- Symptoms often develop gradually and may be mild or absent at first.
- CML diagnosis relies on blood tests, bone marrow analysis, and detection of the Philadelphia chromosome.
- Targeted treatment options have transformed outcomes, making CML a highly treatable disease.
When to Seek Medical Advice
If you experience unexplained, persistent symptoms like significant fatigue, night sweats, persistent low-grade fever, or sudden bruising and bleeding, schedule an appointment with your healthcare provider. While these symptoms can have many causes, early detection and diagnosis improve CML outcomes significantly.
Conclusion
Understanding the genetic underpinnings of chronic myeloid leukemia empowers patients and families. The discovery of the Philadelphia chromosome not only clarified the cause of CML but also opened a pathway for highly effective, targeted treatments. With ongoing advancements in research and care, the prognosis for individuals with CML continues to improve.
Related Resources
- Leukemia & Lymphoma Society – Support, doctor directories, patient stories
- Cancer Research UK – Patient information on diagnosis, treatments, and recovery
- City of Hope – Symptoms and expert-led clinical guidance for CML
References
- https://www.cityofhope.org/clinical-program/chronic-myeloid-leukemia/symptoms
- https://www.cancer.org/cancer/types/chronic-myeloid-leukemia/detection-diagnosis-staging/signs-symptoms.html
- https://bloodcancerunited.org/signs-and-symptoms
- https://www.cancerresearchuk.org/about-cancer/chronic-myeloid-leukaemia-cml/symptoms
- https://my.clevelandclinic.org/health/diseases/21845-chronic-myelogenous-leukemia-cml
- https://www.mayoclinic.org/diseases-conditions/chronic-myelogenous-leukemia/symptoms-causes/syc-20352417
- https://www.mountsinai.org/health-library/diseases-conditions/chronic-myelogenous-leukemia-cml
- https://www.cancertherapyadvisor.com/factsheets/chronic-myeloid-leukemia-cml/
Read full bio of Sneha Tete