Gastrointestinal Bleeding: Causes, Symptoms, Diagnosis, and Treatment
Understand the causes, warning signs, diagnostic tests, and treatments for gastrointestinal bleeding and the importance of prompt medical care.
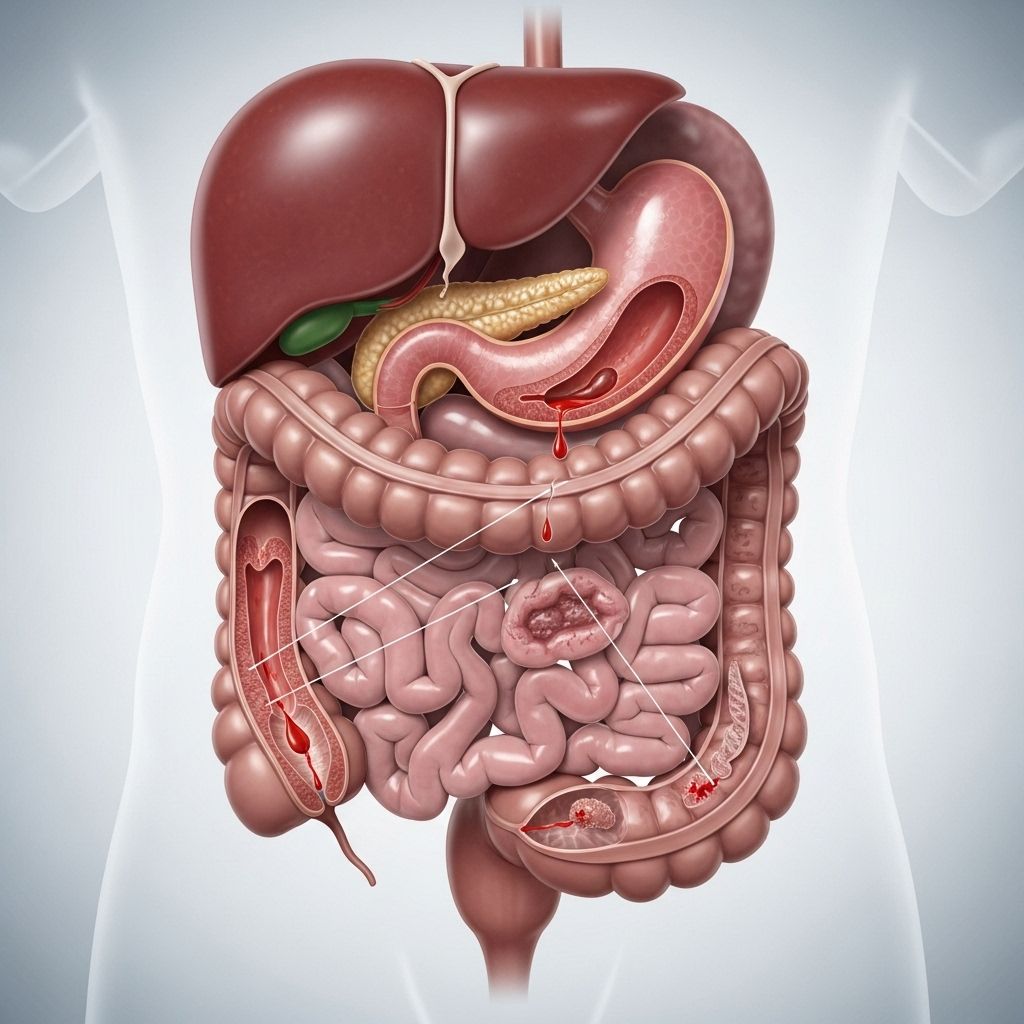
Gastrointestinal (GI) bleeding is a potentially serious condition that occurs anywhere along the digestive tract, from the mouth to the anus. Blood in the stool may signal an urgent health problem, and understanding its causes, warning signs, available tests, and treatment options is crucial for safeguarding your health.
What Is Gastrointestinal Bleeding?
Gastrointestinal bleeding refers to any form of blood loss originating in the digestive tract. The bleeding can be obvious—such as visible blood in stool or vomit—or hidden, detected only through medical tests. GI bleeding is a symptom of a range of underlying conditions, some minor and others potentially life-threatening. Even small amounts of blood loss, over time, can lead to anemia and other complications.
Why Is Blood in the Stool a Sign of Gastrointestinal Bleeding?
The appearance of blood in the stool can result from bleeding at any point in the gastrointestinal tract—from the esophagus to the rectum. Recognizing this symptom quickly and seeking medical attention is critical because:
- Some underlying causes, like peptic ulcers or cancers, can be dangerous if not promptly treated.
- Blood loss (even if subtle) may lead to anemia and reduced oxygen carrying capacity in the blood.
- Prompt diagnosis helps healthcare professionals target and treat the underlying cause before major complications arise.
Types of Gastrointestinal Bleeding
GI bleeding is typically classified based on its source in the digestive tract:
- Upper GI bleeding: Originates from the esophagus, stomach, or the first part of the small intestine (duodenum).
- Lower GI bleeding: Stems from the small intestine beyond the duodenum, colon, rectum, or anus.
The color and appearance of the blood depend on its origin and how long it remains in the digestive system:
- Bright red blood in stool (hematochezia) usually indicates lower GI bleeding, such as from the colon or rectum.
- Dark, tarry stools (melena) suggest upper GI bleeding that has been digested as it moved through the intestines.
What Are the Warning Signs of Gastrointestinal Bleeding?
Symptoms of GI bleeding range from subtle to severe, including:
- Visible blood in stool or on toilet tissue
- Black or tarry stools
- Burgundy or maroon-colored stools
- Vomiting blood or material that resembles coffee grounds
- Unexplained fatigue or weakness
- Shortness of breath
- Lightheadedness or fainting spells
- Paleness of the skin
- Unexplained drop in blood pressure (in severe cases)
Sometimes, especially with slow or minor bleeding, you may not notice any immediate symptoms, but over time it can cause iron deficiency anemia, manifesting as persistent tiredness and weakness.
Urgent Symptoms: When to Seek Emergency Care
Call 911 or emergency services if you experience any of the following with GI bleeding:
- Rapid, heavy blood loss (profuse vomiting of blood or passage of large amounts of blood in stool)
- Severe abdominal or rectal pain
- Signs of shock: rapid heartbeat, low blood pressure, confusion, or unconsciousness
- Shortness of breath, chest pain, or palpitations
For any sign of blood in the stool—particularly if unexpected or persistent—schedule an urgent appointment with your healthcare provider. Do not ignore these symptoms, as early intervention can be life-saving.
What Causes Gastrointestinal Bleeding?
The underlying causes vary depending on the location (upper or lower GI tract):
Common Causes of Upper GI Bleeding
- Peptic ulcers: Sores in the lining of the stomach or duodenum, often due to Helicobacter pylori infection or use of NSAIDs (non-steroidal anti-inflammatory drugs). Gas pain, bloating, and pain after eating are common.
- Esophagitis: Inflammation of the esophagus, often from acid reflux (GERD).
- Gastritis and duodenitis: Inflammation in the stomach or duodenum can erode blood vessels.
- Esophageal or gastric varices: Enlarged veins that can rupture, usually due to liver disease (cirrhosis).
- Mallory-Weiss tears: Tears in the esophageal lining, typically from severe vomiting.
- Upper GI tract tumors: Cancers or benign growths in the stomach or esophagus.
- Foreign body ingestion: Damage and bleeding from swallowed items.
- Portal hypertensive gastropathy: Abnormal stomach blood vessels due to liver disease.
Common Causes of Lower GI Bleeding
- Diverticulosis: Pouches that form in the colon wall may rupture blood vessels.
- Hemorrhoids: Swollen blood vessels in the rectum or anus.
- Anal fissures: Small tears in the anal lining due to constipation or trauma.
- Colon polyps or cancer: Abnormal tissue growths that may bleed, especially during or after bowel movements.
- Inflammatory bowel disease (IBD): Includes Crohn’s disease and ulcerative colitis.
- Ischemic colitis: Reduced blood flow to the colon.
- Infectious or radiation-induced colitis: Infections or damage from cancer treatments.
- Rectal varices: Enlarged veins in the rectum, usually from liver disease.
| Common Cause | Typical Origin | Key Symptoms |
|---|---|---|
| Peptic Ulcer | Upper GI | Abdominal pain, dark stools, nausea |
| Hemorrhoids | Lower GI | Bright red blood, anal discomfort |
| Diverticulosis | Lower GI | Painless bleeding |
| Esophageal Varices | Upper GI | Vomiting blood, signs of liver disease |
| Colon Cancer | Lower GI | Blood in stool, changes in bowel habits |
What Tests Are Used to Diagnose Gastrointestinal Bleeding?
Prompt diagnosis requires a combination of clinical evaluation and diagnostic tests. The goal is to determine the location, cause, and extent of bleeding, which guides treatment decisions. Tests include:
- Medical History & Physical Examination: Review of symptoms, medical history, and risk factors.
- Stool tests: Detect blood not visible to the naked eye (occult blood testing).
- Blood tests: Measure hemoglobin, hematocrit, clotting factors, and check for anemia.
- Endoscopy:
- Upper endoscopy (EGD): A thin tube with a camera investigates the esophagus, stomach, and duodenum. Can diagnose and sometimes treat active bleeding.
- Colonoscopy: A camera inserted through the rectum examines the colon and can remove polyps or treat bleeding vessels.
- Capsule endoscopy: A swallowed camera pill visualizes the small intestine, useful for obscure sources not seen in standard endoscopy.
- Imaging tests:
- CT or MRI angiography: Identifies active bleeding by tracking blood flow.
- Tagged red blood cell scans: Nuclear medicine scan for slow or intermittent bleeding.
How Is Gastrointestinal Bleeding Treated?
The severity, location, and underlying cause of GI bleeding dictate the best treatment:
- Mild or stopped bleeding: Monitoring and supportive care. Sometimes, no treatment is needed if the bleeding stops on its own.
- Endoscopic treatment: During endoscopy, doctors may:
- Inject medications that constrict blood vessels (like epinephrine).
- Apply thermal energy to cauterize bleeding vessels.
- Place clips or bands to stop bleeding vessels or treat varices.
- Remove polyps or tumors causing the bleeding.
- Medications:
- Proton pump inhibitors (PPIs): Suppress stomach acid to promote healing and stop bleeding, usually for upper GI bleeding.
- Antibiotics (for infections like H. pylori causing ulcers).
- Discontinuation of blood thinners or NSAIDs if safe to do so (as instructed by your doctor).
- Blood transfusions: For severe blood loss or dangerously low red cell counts.
- Surgery: Reserved for bleeding that cannot be controlled with endoscopy or interventional radiology.
- Interventional radiology: Minimally invasive procedures to embolize (block) bleeding vessels.
The treatment approach is tailored to the specific cause and location of bleeding and often involves a multidisciplinary medical team.
Preventing Future Bleeding
- Control chronic conditions (such as liver disease, IBD, or peptic ulcer disease).
- Practice careful use of NSAIDs and blood thinners (consult a doctor first).
- Follow a high-fiber diet to prevent constipation and straining.
- Seek prompt medical attention for new or persistent gastrointestinal symptoms.
- Limit alcohol and avoid tobacco use, both of which can damage GI lining.
Potential Complications of Gastrointestinal Bleeding
- Anemia: Chronic blood loss can result in iron deficiency anemia, with symptoms like fatigue, pallor, and weakness.
- Shock: Rapid or profuse bleeding can drop blood pressure to dangerous levels, causing organ failure.
- Death: Rare, but possible if severe bleeding is untreated.
- Complications from underlying disease: Such as cancer, cirrhosis, or inflammatory bowel disease.
- Complications from procedures: In rare cases, tests or treatments may lead to perforation, infection, or further bleeding.
Frequently Asked Questions (FAQs)
Q: What are some common warning signs of gastrointestinal bleeding?
A: Watch out for bright red blood in the stool, black or tarry stools, vomiting blood, and unexplained fatigue. Seek medical attention promptly if these occur.
Q: Is blood in the stool always a medical emergency?
A: Not always—it may be caused by less dangerous conditions such as hemorrhoids. However, it’s important to have new, persistent, or heavy bleeding evaluated urgently to rule out serious problems.
Q: What steps can I take to lower my risk of GI bleeding?
A: Use NSAIDs sparingly, treat chronic conditions that affect digestive health, quit smoking, limit alcohol, and get regular screenings for polyps and cancers if you’re over age 45 or at higher risk.
Q: Can gastrointestinal bleeding recur?
A: Yes, especially if the underlying cause (such as ulcers, varices, or polyps) is not fully addressed. Follow your doctor’s recommendations and attend follow-up appointments for monitoring.
Q: What should I do if I have iron deficiency anemia from chronic GI bleeding?
A: Iron supplements and dietary adjustments may be needed, along with treatment of the cause of bleeding. Ongoing monitoring with your healthcare provider is important.
Takeaway Message
Gastrointestinal bleeding can be caused by a wide range of digestive conditions, from minor hemorrhoids to serious cancers or ulcers. Early recognition and prompt treatment are essential to prevent complications. If you notice blood in your stool or vomit, or experience unexplained fatigue or symptoms of blood loss, contact your healthcare provider promptly. Routine screenings and lifestyle modifications can help prevent many cases of digestive tract bleeding.
References
- https://windsordigestivehealth.com/gastrointestinal-bleeding-causes-symptoms-and-treatment-options/
- https://www.mayoclinic.org/diseases-conditions/gastrointestinal-bleeding/diagnosis-treatment/drc-20372732
- https://www.steris.com/healthcare/knowledge-center/therapeutic-endoscopy/gi-bleeding-sign-symptoms-and-causes
- https://www.ncbi.nlm.nih.gov/books/NBK537291/
- https://www.healthline.com/health/gastrointestinal-bleeding
- https://www.niddk.nih.gov/health-information/digestive-diseases/gastrointestinal-bleeding/symptoms-causes
- https://www.mayoclinic.org/diseases-conditions/gastrointestinal-bleeding/symptoms-causes/syc-20372729
- https://my.clevelandclinic.org/health/diseases/23391-gastrointestinal-gi-bleeding
- https://www.mountsinai.org/health-library/symptoms/gastrointestinal-bleeding
- https://www.nyp.org/digestive/gastrointestinal-gi-bleeding
Read full bio of medha deb












