Gastroesophageal Reflux Disease (GERD): Symptoms, Causes, Diagnosis, and Management
Understand GERD—its causes, symptoms, complications, and treatment options to manage acid reflux and improve digestive health.
Gastroesophageal Reflux Disease (GERD)
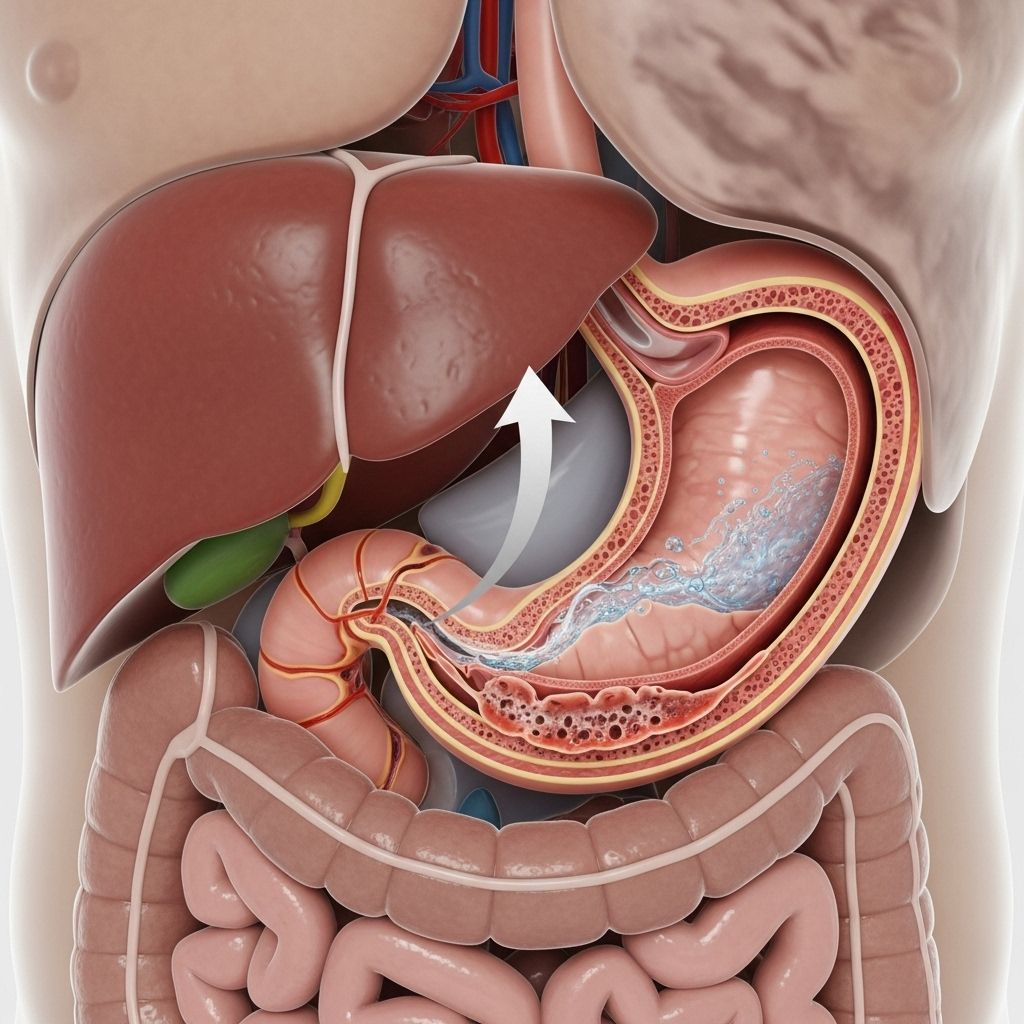
Gastroesophageal Reflux Disease (GERD) is a chronic digestive disorder that affects millions of people worldwide. It occurs when stomach acid frequently flows back into the esophagus, irritating the lining and leading to discomfort and potential long-term complications. With proper understanding and management, individuals affected by GERD can take steps to control symptoms and maintain a healthy quality of life.
What is GERD?
Gastroesophageal Reflux Disease (GERD) is a condition where the acidic contents of the stomach move upward into the esophagus. This backwash, known as acid reflux, can cause a variety of uncomfortable symptoms and, if persistent, may damage the esophageal lining.
How GERD Differs from Occasional Heartburn
While occasional heartburn is common and often resolves on its own, GERD is diagnosed when acid reflux occurs at least twice a week or severely impairs daily life. Chronic reflux exposes the esophagus to acid, which can lead to more serious health issues.
Symptoms of GERD
GERD presents a range of symptoms; some are typical and others are less common. The severity and frequency of these symptoms can vary between individuals.
- Heartburn: A burning sensation in the chest, particularly after eating or when lying down.
- Regurgitation: A sour or bitter-tasting acid backing up into the throat or mouth.
- Chest Pain: Can mimic the pain of heart disease, but is typically non-cardiac.
- Dysphagia: Difficulty or pain while swallowing.
- Sore Throat and Hoarseness: Persistent irritation, often worse in the mornings.
- Chronic Cough or Wheezing: Sometimes worse at night, especially when reflux affects the respiratory tract.
- Bad Breath: Caused by stomach acid and residual food in the esophagus.
- Bloating and Belching: Discomfort or a feeling of fullness in the stomach.
- Other Symptoms: Hiccups, nausea, and a lump-in-throat sensation.
GERD in Children and Infants
- Frequent or effortless vomiting and spitting up
- Chronic cough or wheezing
- Refusing food or difficulty feeding
- Poor weight gain
- Bad breath and excessive burping
- Restlessness or inconsolable crying, especially after feeding
In most infants, symptoms improve as they get older, but persistent or severe symptoms should be evaluated by a healthcare provider.
When to See a Doctor
Consult a healthcare provider if:
- Symptoms occur several times a week
- Over-the-counter medications do not relieve symptoms
- Symptoms are severe or worsening
- There is difficulty or pain with swallowing
- There are alarming symptoms such as:
- Persistent vomiting
- Vomiting blood
- Unintended weight loss
- Anemia (low red blood cell count)
Prompt evaluation can help identify GERD and rule out more serious conditions.
What Causes GERD?
GERD results from the failure of the lower esophageal sphincter (LES), a ring of muscle at the base of the esophagus, to function properly. The LES typically acts as a one-way valve allowing food into the stomach and preventing backflow. When it weakens or relaxes inappropriately, acid escapes upward.
Risk Factors for GERD
- Overweight or Obesity: Increases abdominal pressure, weakening the LES.
- Large Meals or Fatty Foods: Delay stomach emptying and require more acid to digest, increasing reflux risk.
- Certain Foods and Drinks: Coffee, chocolate, peppermint, alcohol, and spicy or acidic foods can relax the LES.
- Smoking: Weakens the LES and reduces saliva, which neutralizes acid.
- Pregnancy: Hormonal changes and increased abdominal pressure promote reflux.
- Hiatal Hernia: Part of the stomach pushes through the diaphragm, impairing LES function.
- Gastroparesis: Delayed stomach emptying can increase reflux.
- Certain Medications: Some blood pressure medications (like calcium-channel blockers), nitrates, and non-steroidal anti-inflammatory drugs (NSAIDs) may trigger or worsen symptoms.
- Stress: May exacerbate symptoms in some people.
- Genetic Factors: Family history can increase risk.
Complications of GERD
Unchecked, GERD can cause significant, long-term complications:
- Esophagitis: Inflammation of the esophageal lining, possibly leading to ulcers and bleeding.
- Esophageal Strictures: Narrowing of the esophagus from scar tissue, making swallowing difficult.
- Barrett’s Esophagus: Pre-cancerous changes in the esophageal lining that increase the risk of esophageal adenocarcinoma.
- Esophageal Cancer: Prolonged damage may rarely lead to cancer.
- Respiratory Problems: Acid may irritate the airways, leading to chronic cough, asthma symptoms, or aspiration pneumonia.
- Dental Erosion: Acid backwash can erode tooth enamel, increasing cavity risk.
Diagnosing GERD
Diagnosis of GERD is usually based on symptom history and response to treatment. In some cases, further testing is required to confirm the diagnosis and assess damage.
- Medical History and Physical Exam: Providers ask about symptoms, triggers, frequency, and impact.
- Trial of Acid Suppression: Improvement with acid-reducing medications often supports the diagnosis.
- Endoscopy (EGD): A flexible camera examines the esophagus for inflammation, ulcers, or Barrett’s esophagus.
- Esophageal pH Monitoring: Measures how often and how long stomach acid enters the esophagus.
- Esophageal Manometry: Evaluates the function of esophageal muscles and sphincters.
- Barium Swallow X-rays: Helps detect structural abnormalities.
Additional tests may be used in children, those with atypical symptoms, or when complications are suspected.
Treatment and Management of GERD
The treatment of GERD focuses on symptom relief, healing the esophagus, and preventing recurrence or complications. Management often involves a combination of lifestyle changes and medications, with surgery as an option for select patients.
Lifestyle and Dietary Modifications
- Eat Smaller Meals: Large meals increase stomach pressure and reflux risk.
- Avoid Trigger Foods and Drinks: Reduce or eliminate coffee, chocolate, spicy foods, alcohol, fatty foods, and peppermint.
- Don’t Lie Down After Eating: Wait at least two to three hours before reclining or going to bed.
- Lose Excess Weight: Reduces pressure on the stomach and lowers reflux frequency.
- Quit Smoking: Smoking worsens reflux and delays healing.
- Elevate the Head of Your Bed: Raising the head by 6-8 inches can decrease nighttime symptoms.
- Wear Loose Clothing: Tight clothes can squeeze your stomach and promote reflux.
Medications
- Antacids: Provide quick, short-term relief by neutralizing stomach acid.
- H2 Blockers: Reduce acid production (e.g., famotidine, ranitidine*).
- Proton Pump Inhibitors (PPIs): Stronger acid blockers that help heal esophagitis, recommended for moderate to severe symptoms (e.g., omeprazole, lansoprazole).
- Prokinetics: Help the stomach empty more quickly, reducing reflux (used less often due to side effects).
*Note: Ranitidine has been withdrawn from many markets due to impurity concerns. Always consult your healthcare provider about safe options.
Surgical and Procedural Interventions
- Fundoplication: The upper part of the stomach is wrapped around the LES to strengthen it and stop reflux.
- LINX Device: A small ring of magnetic beads is placed around the LES to reinforce its closure.
- Other procedures or newer approaches may be employed in select cases.
Surgery is usually reserved for those with severe symptoms unresponsive to medication or complications such as strictures or Barrett’s esophagus.
Prevention of GERD
Many of the lifestyle strategies used to manage GERD can also help prevent its onset or reduce recurrences:
- Maintain a healthy weight
- Eat balanced, small meals
- Limit alcohol and caffeine
- Don’t smoke
- Manage stress effectively
- Avoid eating close to bedtime
Living With GERD
Managing GERD is an ongoing process. Most people can control their symptoms with a combination of lifestyle changes and medication. Staying informed, adhering to medical advice, and regular follow-up care are vital for long-term well-being.
Frequently Asked Questions (FAQs) About GERD
Q: Is GERD the same as acid reflux?
A: GERD is a long-term, more severe form of acid reflux that occurs when reflux is frequent or chronic, leading to symptoms or complications.
Q: What are the warning signs that require urgent medical attention?
A: Difficulty or pain on swallowing, persistent vomiting, vomiting blood, unexplained weight loss, or signs of bleeding (black or tarry stools) need prompt evaluation.
Q: Can GERD be cured?
A: While many people can manage symptoms with lifestyle changes and medication, some may have persistent symptoms requiring ongoing treatment. Surgical options can provide lasting relief for some patients.
Q: How is GERD diagnosed in children?
A: Diagnosis in children usually relies on observation of feeding difficulties, growth issues, or respiratory symptoms, but endoscopy and pH monitoring may be needed in select cases.
Q: Are there any long-term risks related to taking GERD medications?
A: Long-term use of proton pump inhibitors (PPIs) may increase the risk for certain side effects like vitamin B12 deficiency, reduced calcium absorption, or rare infections. Always use medications as directed by your healthcare provider.
Summary Table: Key Features of GERD
| Aspect | Key Details |
|---|---|
| Primary Symptoms | Heartburn, regurgitation, chest pain, sore throat, cough |
| Main Risk Factors | Obesity, hiatal hernia, pregnancy, certain foods/meds, family history |
| Diagnosis | History, physical exam, endoscopy, pH monitoring, manometry |
| Complications | Esophagitis, strictures, Barrett’s esophagus, cancer, respiratory issues |
| Treatment | Lifestyle/diet changes, medications, surgery (in select cases) |
Conclusion
Gastroesophageal Reflux Disease is a widespread condition that can impact daily comfort and long-term health. By understanding its causes, recognizing its symptoms, and following evidence-based management strategies, individuals can take active steps toward minimizing symptoms and preventing complications. If you suspect you may have GERD, consult your healthcare provider for an accurate diagnosis and tailored treatment plan.
References
- https://www.nidirect.gov.uk/conditions/heartburn-and-gastro-oesophageal-reflux-disease-gord
- https://www.nhs.uk/conditions/heartburn-and-acid-reflux/
- https://en.wikipedia.org/wiki/Gastroesophageal_reflux_disease
- https://www.ncbi.nlm.nih.gov/books/NBK554462/
- https://www.mayoclinic.org/diseases-conditions/gerd/symptoms-causes/syc-20361940
- https://my.clevelandclinic.org/health/diseases/17019-acid-reflux-gerd
- https://www.aurorahealthcare.org/services/gastroenterology-colorectal-surgery/gastroesohageal-reflux-gerd
Read full bio of medha deb












