Fundoscopy and Wet Macular Degeneration: Screening, Diagnosis, and What to Expect
Understand how fundoscopy uncovers wet macular degeneration, its key findings, differences from dry AMD, and role in the diagnostic process.
Wet macular degeneration, particularly the age-related form (AMD), represents a major cause of vision impairment and blindness worldwide. Timely diagnosis offers the best chance of preserving vision. Among available examination techniques, fundoscopy stands as a critical first-line tool for both screening and diagnosis, helping eye care professionals detect and differentiate forms of macular degeneration. This comprehensive guide explores what fundoscopy is, how it identifies wet macular degeneration, and how this condition is distinguished from other macular diseases.
What is Fundoscopy?
Fundoscopy—also referred to as ophthalmic examination, ophthalmoscopy, or funduscopy—is a direct visual inspection of the back of the eye (the fundus) using a specialized tool called a fundoscope or ophthalmoscope. The retina, macula, optic disc, and retinal blood vessels become visible to the examiner, making this test foundational for detecting a range of retinal diseases.
- Often performed by ophthalmologists but also within the training of many primary care physicians.
- Relatively quick, non-invasive, and painless.
- Typically requires temporary dilation of the pupil using medicated eye drops for better visualization.
During the procedure, the patient may experience temporary blurry vision or sensitivity to light for a few hours.
Purpose of Fundoscopy in Wet Macular Degeneration
The primary aim of fundoscopy in cases of suspected wet macular degeneration is to:
- Spot characteristic retinal changes such as leaking blood vessels, hemorrhages, and fluid accumulation beneath the retina.
- Screen for and differentiate between wet and dry forms of age-related macular degeneration.
- Guide further testing—fundoscopy can suggest areas where more advanced scans (e.g., OCT, fluorescein angiography) should focus.
Macular degeneration causes the central part of your retina (the macula) to break down or sustain damage, impairing detailed central vision necessary for reading and recognizing faces.
How Does Fundoscopy Help Diagnose Wet Macular Degeneration?
In the context of wet macular degeneration (wet AMD), fundoscopy is particularly useful for detecting early abnormalities and guiding urgent referrals to ophthalmological care.
The examination process typically proceeds as follows:
- Pupil Dilation: Special drops are administered to dilate the eyes, providing a better view of the fundus.
- Instrument Use: The examiner uses a hand-held tool called a fundoscope, which shines a beam of light and provides magnification.
- Visual Inspection: From a distance of about 12 inches, the doctor evaluates the retina, macula, and associated blood vessels.
Fundoscopy is not associated with discomfort, though vision may be blurry post-exam due to the effects of dilation.
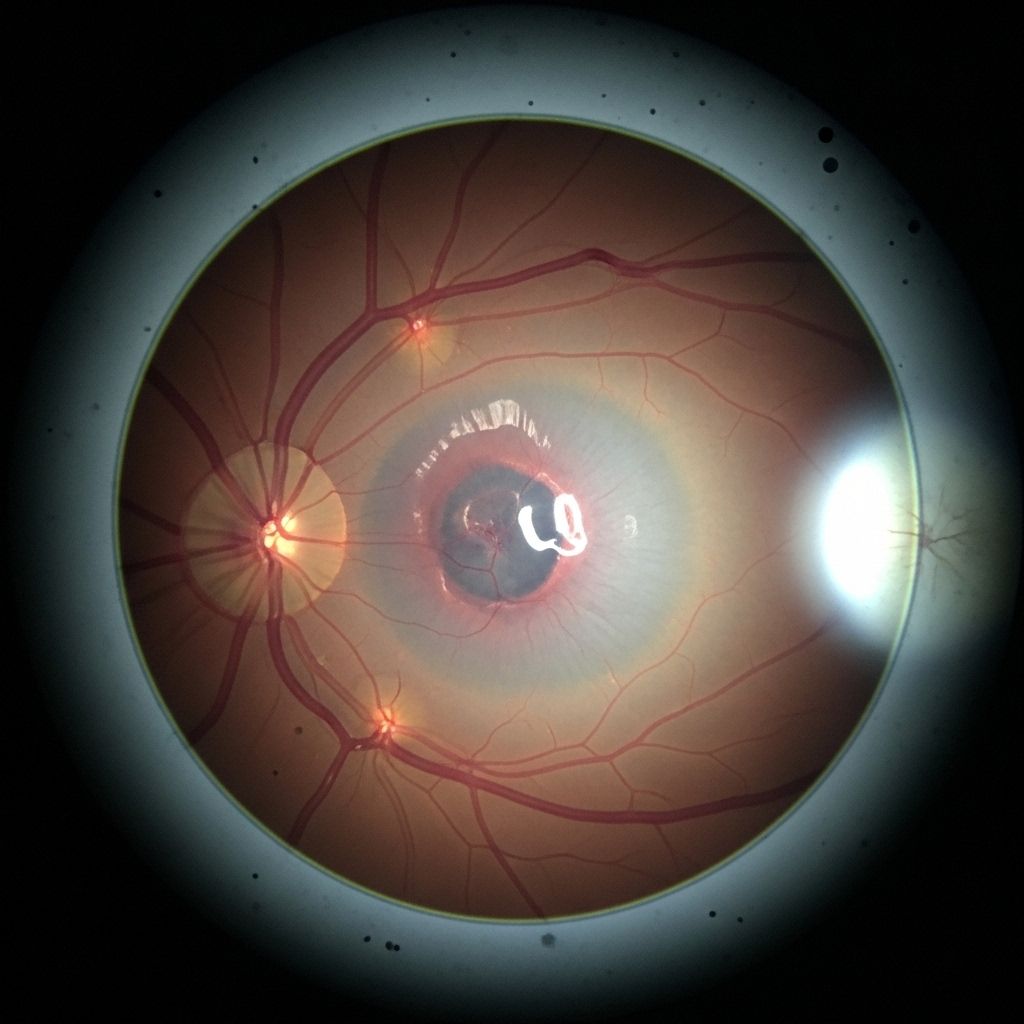
What Does a Funduscopic Exam Reveal in Wet AMD?
During wet macular degeneration, new, abnormal blood vessels (choroidal neovascularization) grow beneath the retina and macula. These fragile vessels leak blood or fluid, causing swelling, damage, and rapid deterioration of central vision.
The main funduscopic findings associated with wet AMD include:
- Retinal Hemorrhages: Patches or dots of blood under or near the macula, indicating bleeding from leaky vessels.
- Subretinal Fluid: Visible as swelling around or under the macula due to the escape of fluid from abnormal vessels.
- Exudates: Yellowish or whitish deposits of protein or lipid material, arising from leaky vasculature.
- Retinal Pigment Epithelium Detachment: A raised area where the retina is separating from the underlying tissue, sometimes seen as a dome-shaped elevation.
- Fibrous or Scar Tissue: Advanced cases may show gray-white patches from scar formation as the eye attempts to heal the damaged macular area.
Wet vs. Dry Macular Degeneration: Fundoscopic Differences
Age-related macular degeneration occurs in two main forms—dry and wet. Fundoscopy helps clinicians distinguish between them, which is critical for prognosis and treatment planning.
| Feature | Dry AMD | Wet AMD |
|---|---|---|
| Prevalence | ~85-90% of AMD cases | ~10-15% of AMD cases |
| Progression | Slow, gradual loss of central vision | Rapid, possibly severe vision loss |
| Key Fundoscopic Findings | Drusen (yellow deposits), RPE atrophy | Hemorrhages, subretinal/exudative fluid, neovascularization |
| Symptoms | Blurry or faded central vision, distortion, difficulty adapting to low light | Sudden loss of central vision, metamorphopsia (visual distortion) |
| Treatment Approach | Lifestyle, supplements, monitoring | Urgent anti-VEGF therapy, possible laser treatment |
By recognizing patterns such as hemorrhages (wet AMD) versus drusen (dry AMD), fundoscopy informs next steps and urgency of intervention.
Other Tests Used Alongside Fundoscopy for Wet Macular Degeneration
While fundoscopy is a valuable first-line assessment, further tests are important for a definitive diagnosis, to assess disease extent, and to guide treatment. Key complementary tests include:
- Optical Coherence Tomography (OCT): Provides cross-sectional, highly detailed images of the retinal layers, showing fluid accumulation or structural distortion in wet AMD.
- Fluorescein Angiography: Involves injecting dye into a vein and photographing retinal blood vessels as the dye flows through, clearly showing leaking or new vessels.
- Visual Acuity Testing: Measures the sharpness of central vision loss, helps monitor treatment effects.
- Amsler Grid: A handheld grid test the patient can use at home or in the office to detect the onset of vision distortion or wavy lines (metamorphopsia).
These diagnostic tools, especially OCT and fluorescein angiography, are considered gold standards for confirming neovascularization and guiding therapy.
Fundoscopic Images: What Might a Doctor See?
- Areas of dark red (blood) in or near the macula (retinal hemorrhage).
- Pale or yellowish areas indicating exudate or subretinal fluid.
- Irregular elevation of the macula, suggesting subretinal or intraretinal fluid.
- Evidence of fibrous tissue or scarring in chronic or treated wet AMD.
These visual patterns allow the examiner to distinguish active disease, monitor progression, or assess post-treatment changes.
Frequently Asked Questions (FAQs)
What exactly is wet macular degeneration?
Wet AMD is a form of age-related macular degeneration where abnormal blood vessels grow under the retina and leak fluid or blood, causing rapid and significant central vision loss.
Does fundoscopy hurt?
No, fundoscopy is painless. The dilating drops may sting briefly, and your vision will be blurry temporarily afterwards.
Can a primary care doctor detect wet AMD with fundoscopy?
Yes, particularly if trained, but ophthalmologists provide more comprehensive retinal examinations and access to advanced imaging techniques for confirmation and monitoring.
Are other diseases detectable with fundoscopy?
Yes. Fundoscopy also screens for diabetic retinopathy, retinal vein occlusions, hypertensive changes, and other retina-affecting disorders.
How soon should someone see a doctor if central vision worsens?
Immediately. Sudden loss of central vision, distortion, or dark spots require prompt ophthalmologic evaluation to preserve vision.
Treatment Implications and Next Steps if Wet AMD is Detected
If fundoscopy or other diagnostic tools confirm wet macular degeneration, rapid intervention is crucial:
- Anti-VEGF Injections: Medications injected into the eye suppress abnormal vessel growth, limit leakage, and can stabilize or improve vision in many cases.
- Photodynamic Therapy (PDT): A light-activated drug is administered intravenously and then activated in the eye to close abnormal vessels—used in select cases.
- Laser Photocoagulation: Seals abnormal vessels, though less commonly used today because of scarring risks and newer options.
- Low Vision Rehabilitation: For advanced disease—training and devices to maximize remaining vision and adapt to central vision loss.
Patient education and regular follow-up are essential for monitoring disease progression and treatment response.
Summary Table: Diagnostic Steps for Wet Macular Degeneration
| Step | Purpose | Typical Findings |
|---|---|---|
| Fundoscopy | Initial screening/examination | Hemorrhages, fluid, exudates, neovascularization |
| OCT | High-resolution cross-sectional imaging | Subretinal/intraretinal fluid, macular elevation |
| Fluorescein Angiography | Visualization of vessel leakage/new vessels | Leakage, neovascular areas, detailed vessel analysis |
| Visual Acuity Test | Assesses degree of central vision loss | Blurred/absent central vision |
| Amsler Grid | Detects visual distortion at home or in clinic | Wavy, missing, or distorted grid lines |
When Should You Seek a Fundoscopic Exam?
If you or someone you know is experiencing new or worsening symptoms such as:
- Blurring or dimming of central vision
- Dark or empty spots in the center of vision
- Distortion of straight lines (metamorphopsia)
- Difficulty reading or recognizing faces
Prompt fundoscopic examination is warranted. Early detection through fundoscopy or advanced imaging can help prevent irreversible vision loss through timely treatment.
Key Takeaways
- Fundoscopy is a safe, fundamental tool that plays an essential role in the diagnosis and monitoring of wet macular degeneration.
- It helps distinguish between wet and dry forms of AMD, detect characteristic retinal changes, and guide further workup and treatment.
- Abnormal retinal blood vessels, fluid accumulation, and hemorrhages are hallmark findings in wet AMD.
- Patients with sudden, unexplained loss or distortion of central vision should be evaluated without delay.
- Early intervention offers the best chance at preserving vision—regular eye exams are critical, especially for those over 50 or at increased risk.
References
- https://www.mayoclinic.org/diseases-conditions/wet-macular-degeneration/diagnosis-treatment/drc-20351113
- https://www.willseye.org/wet-amd/
- https://www.healthline.com/health/eye-health/wet-macular-degeneration-fundoscopy
- https://www.ncbi.nlm.nih.gov/books/NBK572147/
- https://my.clevelandclinic.org/health/diseases/wet-macular-degeneration
- https://www.mayoclinic.org/diseases-conditions/wet-macular-degeneration/symptoms-causes/syc-20351107
- https://www.youtube.com/watch?v=YoDR0A9xo8I
- https://www.retinaeye.com/contents/common-diseases/macular-conditions/wet-age-related-macular-degeneration
Read full bio of Sneha Tete












