Functional Gastrointestinal Disorders: Causes, Symptoms, and Treatments
Explore the causes, symptoms, diagnosis, and management of functional gastrointestinal disorders for improved digestive wellness.
Functional Gastrointestinal Disorders: Causes, Symptoms, Diagnosis, and Treatment
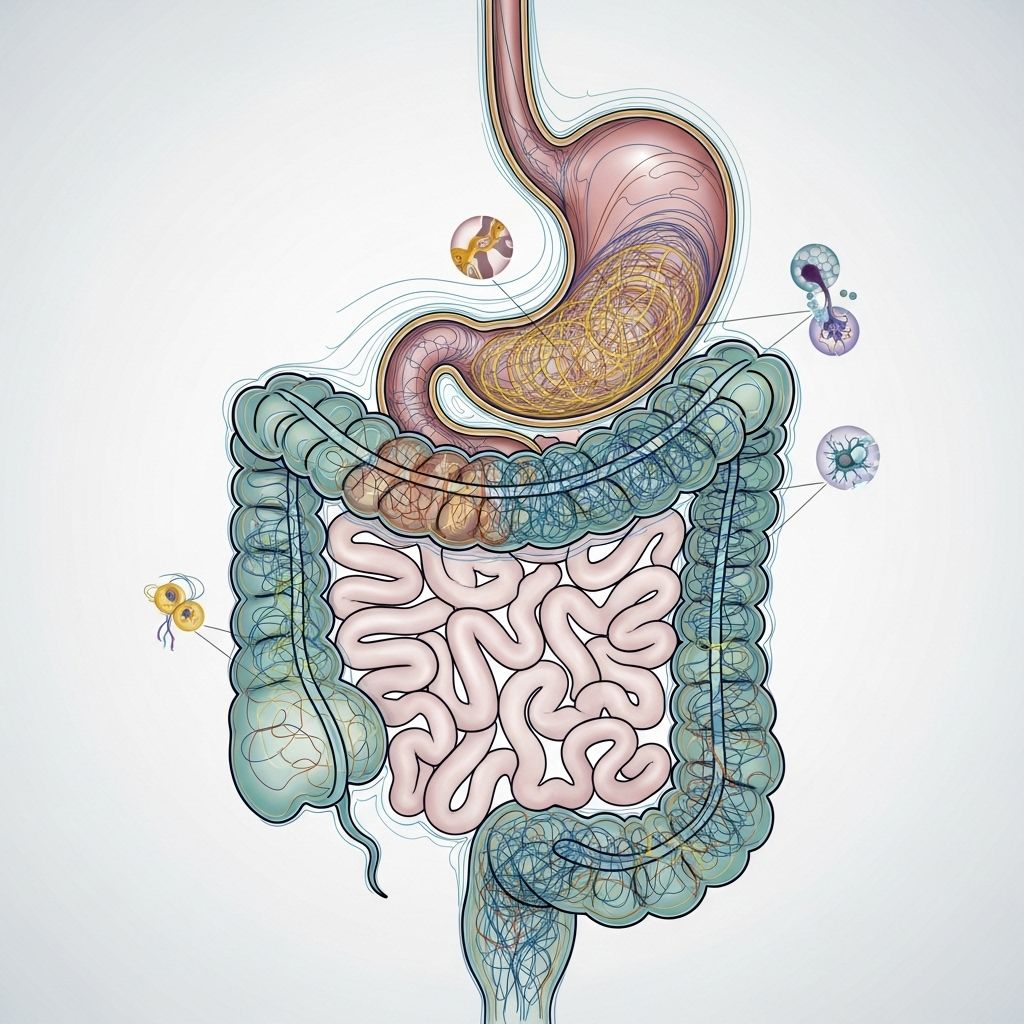
Functional gastrointestinal disorders (FGIDs) are a group of disorders involving persistent and recurring problems in the digestive system. Unlike structural diseases that cause visible changes in organ function or tissue, FGIDs do not have identifiable physical or biochemical abnormalities. Instead, these disorders stem from disruptions in how the gut, brain, and nervous system interact, leading to substantial distress and negative impacts on quality of life.
What Are Functional Gastrointestinal Disorders (FGIDs)?
FGIDs are chronic conditions characterized by gastrointestinal (GI) symptoms without identifiable structural or biochemical causes. These disorders affect how the gut behaves and communicates with the brain and within its own nerve networks, often causing pain and changes in bowel habits.
- FGIDs are diagnosed based on symptom patterns rather than laboratory or imaging abnormalities.
- The most common FGIDs include irritable bowel syndrome (IBS), functional dyspepsia, and functional constipation.
- FGIDs can affect people of all ages, including infants, children, and adults.
How Common Are FGIDs?
FGIDs are among the most frequent complaints in both general and specialized medical practices. Studies estimate that up to 40% of adults globally experience one or more FGID symptoms at some point in their lives. These disorders are a leading cause for visits to gastroenterologists and primary care physicians, and they present significant challenges due to their chronic and recurring nature.
Common Types of FGIDs
FGIDs cover a broad spectrum of digestive issues, with some of the most prevalent types including:
- Irritable Bowel Syndrome (IBS) : Marked by recurring episodes of abdominal pain with alterations in bowel habits (diarrhea, constipation, or both).
- Functional Dyspepsia : Persistent or recurrent upper abdominal discomfort, bloating, or feeling full quickly after eating, without an identifiable medical cause.
- Functional Constipation : Chronic difficulty with infrequent or hard bowel movements.
- Functional Diarrhea : Ongoing frequent, loose stools without a clear medical trigger.
- Functional Abdominal Pain Syndrome : Frequent abdominal pain or discomfort that cannot be explained by other GI conditions.
- Functional Heartburn : Burning sensation in the chest despite normal endoscopy and pH studies.
Common Causes of Functional GI Disorders
The causes of FGIDs are complex and multifactorial, often involving a combination of genetic, environmental, physiological, and psychological factors. These factors can interact and affect the function of the GI tract in several ways:
- Genetics — A family history of FGIDs increases risk, suggesting inherited factors play a role.
- Abnormal GI Motility — Changes in the rhythmic contractions of the gut can lead to symptoms like diarrhea or constipation.
- Gut Hypersensitivity — Increased sensitivity to normal gut activities causes pain, bloating, and discomfort even without actual injury or inflammation.
- Immune and Inflammatory Factors — Subtle changes in gut immune responses or inflammation may contribute, even in the absence of overt disease.
- Altered Nervous System Processing — Dysfunction in communication between the gut and brain (the “gut-brain axis”) plays a major role.
- Microbiome Changes — Variations in gut bacterial populations are increasingly recognized as factors in FGID development and symptoms.
- Environmental Influences — Diet, infections (such as childhood salmonella), and exposure to toxins can all play a role.
- Psychological Factors — Stress, anxiety, depression, and other emotional factors frequently contribute to onset and worsening of symptoms.
Major Risk Factors
- Family history of GI disorders
- Frequent stress or psychological trauma
- Past gastrointestinal infections
- Smoking, certain dietary patterns, and physical inactivity
- Poor sleep or irregular sleep patterns
Typical Symptoms of FGIDs
Physical symptoms of FGIDs can vary widely and depend on the specific disorder. Common symptoms include:
- Abdominal pain or discomfort
- Bloating and visible distension
- Burping and increased belching
- Constipation or diarrhea (sometimes alternating between both)
- Flatulence (increased intestinal gas)
- Indigestion and early satiety
- Nausea or a sensation of queasiness
- Difficulty swallowing (dysphagia) or vomiting (rare)
It’s important to note that physical and mental symptoms are often intertwined. For example, stress, anxiety, and depression may not only result from FGID symptoms, but also exacerbate them, creating a challenging cycle for patients.
Symptoms of FGIDs in Infants and Children
While most symptoms overlap with adults, infants and children with FGIDs may present in unique ways:
- Persistent or recurrent functional abdominal pain
- Excessive gas or bloating
- Colic (prolonged crying in infants)
- Regurgitation and spitting up
Combined FGIDs in infants (such as in the first 6 months) can impact feeding, weight gain, and overall quality of life. Early identification and management are crucial for growth and development.
Diagnosing Functional Gastrointestinal Disorders
Diagnosing FGIDs requires a careful clinical approach, as no single test can definitively confirm these disorders. Instead, diagnosis is guided by symptom-based criteria and the exclusion of structural diseases. Key steps include:
- Detailed medical history and review of symptoms
- Physical examination
- Use of standardized Rome Criteria to classify FGIDs based on specific patterns and duration of symptoms
- Laboratory tests, endoscopy, or imaging only when needed to rule out other conditions (such as infections, inflammatory bowel disease, or cancer)
Once serious causes for the symptoms are excluded, a diagnosis of an FGID can be confidently made and individualized treatment begun.
Treatment and Management of FGIDs
Treatment approaches for FGIDs focus on symptom relief, improving quality of life, and addressing potential triggers. Because of their complex and multifactorial nature, a comprehensive and individualized approach is often necessary. Common components of management include:
Lifestyle Modifications
- Dietary changes — Trials of increased fiber, elimination diets, or a low-FODMAP diet for irritable bowel syndrome can be helpful.
- Regular physical activity
- Adequate hydration
- Improved sleep hygiene
- Smoking cessation
Stress and Mental Health Management
- Cognitive behavioral therapy (CBT)
- Relaxation exercises and mindfulness
- Stress reduction techniques (such as yoga, meditation, or deep breathing)
- Support groups for chronic illness
Medications
- Antispasmodics for abdominal cramps or pain
- Laxatives or fiber supplements for constipation-predominant FGIDs
- Anti-diarrheal agents for diarrhea-predominant cases
- Medications to modulate gut motility or sensitivity
- Low-dose antidepressants for pain and gut-brain axis symptoms (in select cases)
Role of the Gut Microbiome
Research suggests that probiotics and prebiotics may help balance gut bacteria, which can play a role in reducing symptoms and promoting digestive wellness in some individuals. However, benefits can vary and should be discussed with a healthcare provider.
Dietary Approaches
- Low FODMAP diet (fermentable oligo-, di-, monosaccharides and polyols) has shown benefit, especially in IBS.
- Some find relief with gluten restriction, though this is not universally effective or necessary.
- No single diet is recommended for all; dietary adjustments should be personalized.
Prognosis and Long-term Outlook
FGIDs are chronic disorders that may fluctuate over time with periods of remission and exacerbation. While not life-threatening, they can significantly impact daily activities, social functioning, and mental well-being. With appropriate management—especially targeting both gastrointestinal and psychosocial factors—most individuals can achieve substantial improvement in symptoms and quality of life.
Can FGIDs Be Prevented?
There is no known way to entirely prevent FGIDs, but certain lifestyle measures may reduce risk or severity:
- Healthy diet rich in fiber, fruits, and vegetables
- Regular exercise and physical activity
- Effective stress management
- Prompt treatment of gastrointestinal infections
- Avoidance of smoking and excessive alcohol consumption
Frequently Asked Questions (FAQs)
What are the most common functional gastrointestinal disorders?
The most common FGIDs are irritable bowel syndrome (IBS), functional dyspepsia, and functional constipation. Other types include functional diarrhea, functional abdominal pain syndrome, and infant colic.
Are FGIDs dangerous?
FGIDs are not life-threatening but can significantly affect quality of life. They do not increase the risk for cancer or other serious organic diseases, but severe cases can cause profound disruption to daily functioning.
Can children have FGIDs?
Yes. FGIDs are common in children and can present with abdominal pain, bloating, constipation, diarrhea, and regurgitation. Infants may experience colic, gas, or feeding difficulties. Early management can improve outcomes.
How do mental health factors influence FGIDs?
Anxiety, depression, and chronic stress can worsen FGID symptoms through effects on the “gut-brain axis.” Addressing mental health is a key component of effective FGID management.
Can changing my diet help with FGIDs?
Many find symptom relief by modifying their diet (such as following a low-FODMAP diet, increasing fiber, or avoiding trigger foods). Dietary changes should be individualized and best undertaken with a healthcare provider or dietitian’s input.
Do probiotics help FGID symptoms?
Some probiotic strains can help ease bloating, gas, and irregularity, likely by balancing gut bacteria. Effectiveness varies by individual, and it is best to discuss with a healthcare professional before starting.
When to See a Doctor
Consult a healthcare provider if you experience:
- New or worsening abdominal pain, especially with fever or weight loss
- Blood in stool
- Severe or persistent diarrhea or vomiting
- Unexplained weight loss
Early evaluation can help rule out other causes and design the most effective management plan.
Quick Reference Table: FGID Comparison
| Disorder | Key Symptoms | Usual Age | Main Triggers | Primary Treatments |
|---|---|---|---|---|
| Irritable Bowel Syndrome (IBS) | Abdominal pain, bloating, diarrhea, constipation | Teens & adults | Stress, diet, gut microbiome | Diet, stress management, medications |
| Functional Dyspepsia | Upper abdominal pain, fullness, nausea | Teens & adults | Diet, stress | Diet, acid suppressants, prokinetics |
| Functional Constipation | Hard stools, straining, infrequent BM | Children, adults | Low fiber, inactivity | Fiber, hydration, laxatives |
| Infant Colic | Excessive crying, gas, fussiness | Infants (0–6 mo) | Unknown, feeding changes | Feeding advice, soothing |
Additional Resources
- International Foundation for Gastrointestinal Disorders (IFFGD)
- American College of Gastroenterology
- Rome Foundation for Functional GI Disorders
References
- https://www.healthline.com/health/digestive-health/functional-gastrointestinal-disorder
- https://en.wikipedia.org/wiki/Functional_gastrointestinal_disorder
- https://www.mayoclinic.org/diseases-conditions/irritable-bowel-syndrome/symptoms-causes/syc-20360016
- https://www.med.unc.edu/ibs/wp-content/uploads/sites/450/2017/10/What-Is-Functional-GI.pdf
- https://www.ynhh.org/services/digestive-health/functional-gastrointestinal-disorders
- https://iffgd.org/gi-disorders/functional-gi-disorders/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7850201/
- https://gi.org/topics/functional-gastrointestinal-disorders-in-pediatric-and-adolescent-patients/
- https://www.fda.gov/files/about%20fda/published/The-Voice-of-the-Patient–Functional-Gastrointestinal-Disorders.pdf
Read full bio of medha deb












