Fontan Procedure: Purpose, Steps, Benefits, and Long-Term Outlook
A comprehensive guide to understanding the Fontan procedure, its stages, risks, benefits, and life after surgery.
The Fontan procedure is a complex heart surgery performed primarily on young children with certain congenital heart defects, most notably those who have only one functional ventricle. This article explores the reasons for the Fontan procedure, how the surgery is performed, who needs it, what to expect at each stage, risks and recovery, and life after the operation.
What Is the Fontan Procedure?
The Fontan procedure is a palliative surgical technique for children born with a single functional ventricle. It reroutes blood returning from the body so it flows directly to the lungs, bypassing the heart’s pumping chambers that usually handle this flow. This circulation pattern, called Fontan circulation, helps improve oxygenation and allows the single working ventricle to pump only oxygen-rich blood to the body.
- Main goal: Separate oxygen-rich (red) and oxygen-poor (blue) blood, improving blood oxygen levels.
- Patient group: Typically used in children with single ventricle defects such as hypoplastic left heart syndrome (HLHS), tricuspid atresia, and some cases of double outlet right ventricle.
- Outcome: Not a cure, but a life-extending approach improving quality of life and physical function.
Who Needs the Fontan Procedure?
This surgery is indicated for individuals with congenital heart defects resulting in only one functional ventricle that cannot be addressed by a two-ventricle repair.
Common diagnoses requiring the Fontan procedure include:
- Hypoplastic Left Heart Syndrome (HLHS): The left side of the heart (including the left ventricle and valves) is underdeveloped, making normal oxygenated blood flow to the body impossible.
- Tricuspid Atresia: The tricuspid valve is either missing or abnormally developed, impairing blood flow from the right atrium to the right ventricle.
- Other Complex Single Ventricle Defects: Some rare malformations where one of the ventricles is too small or poorly developed to support circulation.
Typical Age and Surgical Planning
Most children undergo the Fontan operation at 18 months to around 3 years of age, though timing depends on a child’s growth, health status, and how they respond to previous procedures as part of staged reconstruction.
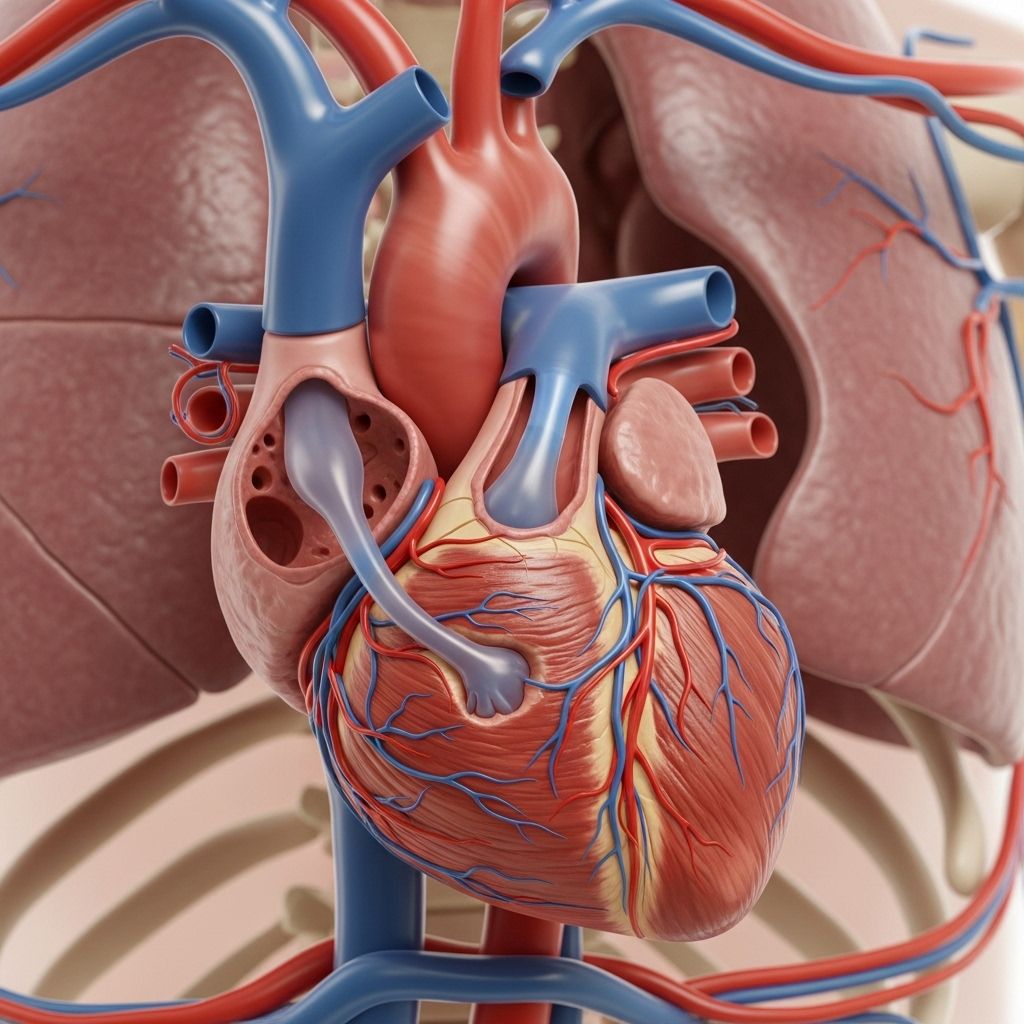
How Does the Normal Heart Work Versus a Single Ventricle Heart?
In a normal heart, two ventricles pump blood:
- Right ventricle: Receives oxygen-poor blood from the body and sends it to the lungs.
- Left ventricle: Receives oxygen-rich blood from the lungs and pumps it to the body.
In a single ventricle heart:
- One ventricle is too small or absent, so both oxygen-rich and oxygen-poor blood may mix.
- This mixing reduces the amount of oxygen delivered to the body, leading to cyanosis (bluish skin) and other health issues.
Staged Surgical Approach Leading to the Fontan
The Fontan is usually the third stage of a complex reconstructive process known as “staged reconstruction” or “single ventricle palliation.” Each stage addresses specific circulatory challenges:
| Stage | Typical Age | Main Objective |
|---|---|---|
| Stage 1: Norwood Procedure | First week of life | Reconfigure the aorta and pulmonary artery; create stable systemic circulation. |
| Stage 2: Glenn or Hemi-Fontan | 4-6 months | Connect superior vena cava (from upper body) directly to pulmonary arteries. |
| Stage 3: Fontan Procedure | 18 months–3 years | Connect inferior vena cava (from lower body) to pulmonary arteries. Complete Fontan circulation. |
How Is the Fontan Procedure Performed?
The core idea is to redirect oxygen-poor blood from the lower body directly into the lungs, bypassing the heart. The surgery is performed under general anesthesia and typically takes several hours.
- Blood is rerouted so that it flows passively, driven by venous pressure, into the lungs for oxygenation.
- The working ventricle now only pumps oxygen-rich blood to the body.
The technique is customized for each patient, but the two main modern types of Fontan procedures are:
- Lateral Tunnel (Intracardiac): Uses a “baffle” (patch) inside the right atrium to guide blood from the inferior vena cava to the pulmonary arteries.
- Extracardiac Conduit: Employs an artificial tube outside the heart to connect the inferior vena cava directly to the pulmonary arteries, minimizing contact with the heart tissue.
Fenestration
Often, a small hole (fenestration) is purposely left in the baffle or tube. This “pop-off” valve allows pressure to escape if it builds up in the lungs and helps prevent complications. Typically, this hole closes naturally over time or is closed later using a catheter-based procedure.
Benefits and Expected Outcomes
- Significant increase in blood oxygen levels, often resulting in noticeably “pinker” skin and improved exercise tolerance.
- Reduction or removal of symptoms such as chronic fatigue, poor growth, and cyanosis.
- Increased life expectancy compared to untreated single ventricle defects, although not equivalent to having a fully normal heart.
- Improved quality of life and better ability to participate in everyday childhood activities.
Risks, Complications, and Limitations
Fontan surgery, while providing significant benefits, carries important short-term and long-term risks:
Short-Term Risks
- Bleeding and blood clots
- Infection at surgical site
- Arrhythmias (irregular heart rhythms)
- Pneumonia or lung complications
- Need for additional surgery due to complications
Long-Term Complications
- Protein-losing enteropathy (PLE): A condition where proteins are lost from the gut, potentially causing swelling and nutritional issues.
- Arrhythmias: Heart rhythm abnormalities may develop months or years after the procedure.
- Liver complications: Chronic congestion and increased pressure can cause liver problems over time.
- Pulmonary arteriovenous malformations, reduced exercise capacity, and increased risk of stroke or heart failure in adulthood.
- Potential need for heart transplantation later in life.
Recovery After the Fontan Procedure
Hospital recovery typically takes 2 to 3 weeks, depending on the child’s response and absence of complications.
- Initial care usually occurs in the pediatric intensive care unit (PICU).
- Children may require mechanical ventilation (breathing support) for several days after surgery.
- Medications to manage heart function, fluid, and anticoagulation (blood thinners) are common.
- Clear fluids and nutrition are provided, moving gradually back to a normal diet as tolerated.
Before discharge, care teams educate families on:
- Signs of infection, heart failure, or poor circulation to watch for
- How to give medications and use home monitoring equipment
- Follow-up schedule for cardiac checkups and testing
Life and Long-Term Care After the Fontan Procedure
Fontan patients require lifelong, specialized cardiac care. Survival rates and outcomes have steadily improved, but ongoing medical management is critical:
- Routine heart monitoring with echocardiogram, ECG, and sometimes MRIs or cardiac catheterization as the child grows.
- Anticoagulation (“blood thinning”) medications to prevent clots.
- Regular assessment of liver function and screening for protein loss or arrhythmias.
- Encouragement of moderate activity, good nutrition, and avoiding dehydration.
- Transition of care planning into adulthood, as increased numbers of Fontan patients now reach their 20s, 30s, and beyond.
Potential Complications and Red Flags to Watch For
While most children do well after Fontan surgery, certain symptoms should prompt urgent medical attention:
- Unexplained swelling in the abdomen, legs, or face
- Increased fatigue or shortness of breath
- New bluish discoloration, especially of the lips or nails
- Decreased urine output, persistent cough, or signs of infection
- Abdominal pain or vomiting
Frequently Asked Questions (FAQs) About the Fontan Procedure
What are the signs that my child might need the Fontan procedure?
Children with single ventricle heart defects who develop cyanosis (bluish discoloration due to low oxygen), show poor growth, or have oxygen saturations well below normal usually need staged reconstructive surgery, culminating in the Fontan.
Is the Fontan procedure a cure for congenital heart disease?
No. The Fontan procedure does not cure the underlying defect but restructures blood flow to improve quality and length of life with continued long-term risks.
How long do children live after the Fontan procedure?
Most children survive into adulthood and many live decades after their operation thanks to advances in care. However, lifelong specialized follow-up is needed to manage late complications.
Can a child live a normal life after the Fontan procedure?
Many Fontan patients can attend school, engage in recreational activities, and lead active lives, though certain limits and precautions are necessary and intense sports may not be safe.
Will my child need more surgery after the Fontan?
Some children may need further interventions if complications occur (e.g., arrhythmias, baffle blockage, protein-losing enteropathy) or if the Fontan circulation fails later in life. Rarely, a heart transplantation may be necessary.
What is the long-term outlook for children after the Fontan procedure?
With expert, life-long care, the majority of Fontan patients enjoy substantial improvements but face potential late complications, including arrhythmias, liver changes, and increased risk for heart failure or organ problems as adults. Ongoing advances continue to improve these outcomes.
References
- https://en.wikipedia.org/wiki/Fontan_procedure
- https://www.mottchildren.org/conditions-treatments/ped-heart/treatment/fontan-operation
- https://www.cincinnatichildrens.org/health/f/fontan-procedure
- https://www.chop.edu/treatments/staged-reconstruction-heart-surgery
- https://my.clevelandclinic.org/health/treatments/24545-fontan-procedure
- https://www.ncbi.nlm.nih.gov/books/NBK558950/
- https://www.youtube.com/watch?v=hIpvCUwml3c
- https://www.ahajournals.org/doi/10.1161/circulationaha.106.676445
Read full bio of Sneha Tete












