What Is the First Sign of Diabetic Retinopathy?
Understand the earliest signs, progressive symptoms, and modern treatments for diabetic retinopathy before it threatens your vision.
Medically reviewed by Kelly Wood, MD — Written by Christine Fallabel
Diabetic retinopathy is a major complication that can affect anyone living with diabetes — often silently in its early stages. Detecting the initial signs is crucial for prompt intervention and preserving vision. This guide uncovers the earliest signs of diabetic retinopathy, how it progresses, and what you can do if you notice symptoms.
Understanding Diabetic Retinopathy
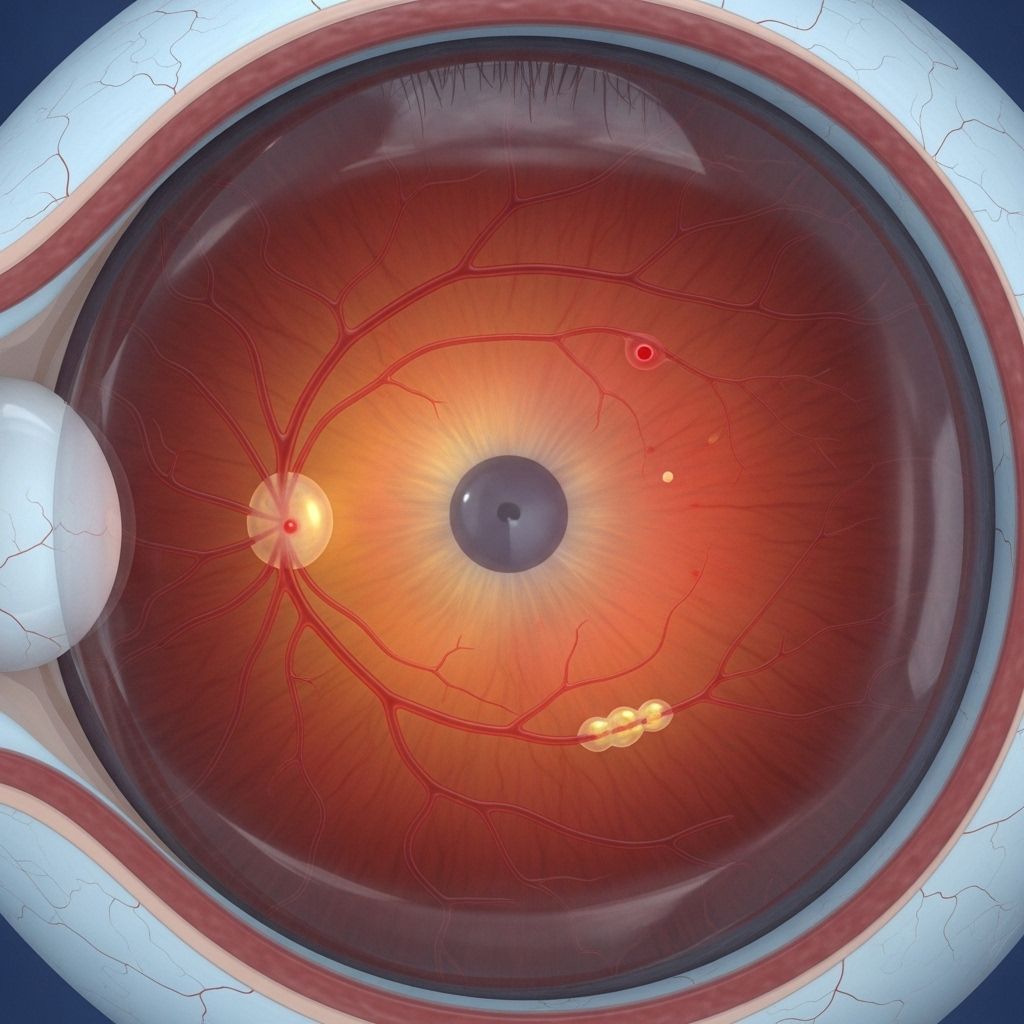
Diabetic retinopathy is an eye condition that results from high blood sugar levels damaging the small blood vessels in the retina — the light-sensitive tissue at the back of the eye. Over time, this can cause vision problems and, if untreated, lead to blindness. Diabetic retinopathy affects both type 1 and type 2 diabetes, and is a leading cause of vision loss in working-age adults.
Research suggests the prevalence is significant:
- Up to 75% of people with type 1 diabetes and 50% of those with type 2 diabetes will develop some degree of retinopathy in their lifetime.
- Diabetic retinopathy accounts for over 80% of vision loss in people with diabetes.
Yet, the first symptoms are often subtle, making regular screening vital for those living with diabetes.
Early Symptoms: What Is Usually the First Sign?
The earliest signs of diabetic retinopathy can be easy to miss. Most people do not experience noticeable symptoms in the very early stages, which is why annual eye screenings are so important. When symptoms do appear, blurry vision is often the first and most common warning sign. Others may notice dark spots or floaters in their field of vision.
Common Early Symptoms Include:
- Blurred vision — Objects may appear out of focus or hazy, especially when blood sugar levels fluctuate.
- Floaters — Small, dark shapes or specks that drift through your vision, caused by bleeding or fluid leakage in the retina.
- Dark spots — Patchy or shadowed areas that obscure parts of your sight, especially in one or both eyes.
These changes are often gradual and may come and go, especially if your blood glucose levels are not well-managed. Not everyone will notice symptoms early, so people with diabetes should not wait for noticeable vision changes before seeking assessment.
Why Diabetic Retinopathy Develops
Diabetic retinopathy is directly driven by prolonged high blood sugar. Over time, this damages the tiny blood vessels in the retina, causing them to leak fluid or bleed. This initial stage, called nonproliferative diabetic retinopathy (NPDR), can progress to more severe forms if not detected and managed early.
- High blood sugar weakens capillary walls in the retina.
- Leaky vessels lead to swelling, bleeding, and fluid build-up.
- Retinal tissue may become deprived of oxygen, triggering the growth of abnormal new blood vessels (proliferative phase).
While anyone with diabetes is at risk, poor blood sugar control and longer duration of diabetes raise the odds significantly. High blood pressure and cholesterol levels also contribute to risk.
Other Signs of Retinopathy as the Disease Progresses
As retinopathy advances, symptoms become more apparent. Vision changes may interfere with daily activities such as reading, recognizing faces, or driving. The main progressive signs include:
- Increasingly blurry vision — Persistent or worsening haziness despite glasses or contacts.
- Fluctuating vision — Vision quality changes from day to day or throughout the day.
- Poor night vision — Difficulty seeing in low light or at night.
- Trouble distinguishing colors — Particularly blue-yellow discrimination.
- Blank or dark areas — Section of the visual field that appears missing or shadowed.
- Sudden, severe vision loss — Can occur if blood vessels rupture and bleed into the eye (vitreous hemorrhage).
- Difficulty with reading or recognizing details — Fluid accumulation in the retina’s center (macular edema) can blur central vision.
- Eye pain or pressure — Rare, usually in advanced, sight-threatening stages.
Symptoms can vary between individuals and often affect both eyes. Some people may also notice:
- Poor peripheral vision — Trouble seeing objects to the side.
- Wavy or distorted vision — Straight lines may appear bent or rippled.
Stages of Diabetic Retinopathy
| Stage | Characteristics | Symptoms |
|---|---|---|
| Nonproliferative (NPDR), mild/moderate | Small areas of swelling, leaking, and bleeding; no new vessel growth | Usually minimal or no symptoms |
| Nonproliferative (NPDR), severe | Blockage of many retinal blood vessels; worsening swelling/bleeding | Blurry vision, more frequent floaters |
| Proliferative (PDR) | Abnormal new blood vessel growth; risk of retinal detachment | Sudden severe vision changes, risk of blindness |
| Diabetic macular edema | Swelling at the center of the retina (macula) | Distorted or loss of central vision |
Vision Loss: Can It Be Reversed?
Unfortunately, vision loss from advanced diabetic retinopathy is challenging to reverse. However, early detection and prompt treatment can significantly slow progression and, in some cases, restore part of lost vision.
The following interventions can help:
- Tight blood sugar control — Reduces the risk of developing or worsening retinopathy.
- Anti-VEGF injections — Medications such as ranibizumab or aflibercept block a protein that promotes abnormal blood vessel growth, helping reduce fluid leakage and swelling. Some people experience modest vision improvement.
- Laser therapy — Targets and seals leaking blood vessels, sometimes recovering partial vision.
- Vitrectomy surgery — Removes blood and scar tissue in severe cases, potentially restoring some vision.
Lifestyle changes are also vital in managing and limiting visual damage:
- Maintain steady blood glucose.
- Manage blood pressure and cholesterol.
- Do not smoke.
- Adopt a healthy diet and regular exercise.
Screening and Eye Care Recommendations
Because early diabetic retinopathy is usually symptomless, regular eye exams are essential. Many countries offer annual diabetic eye screening for people with diabetes aged 12 and above. These screenings often involve:
- Retinal photography to detect damage before symptoms arise.
- Comprehensive dilated eye exams by an eye care specialist.
If you experience any of the following, you should schedule an urgent appointment with your doctor or an eye care professional:
- Sudden or significant vision loss
- Increase in floaters or dark spots
- Persistent blurred vision that does not improve with glasses
- Trouble seeing at night or in low light
Prompt treatment can prevent most severe complications. Do not wait for multiple symptoms to appear before seeking care.
Frequently Asked Questions (FAQs)
What is the very first sign of diabetic retinopathy?
For many, blurred vision or the appearance of floaters (moving dark spots) are the earliest signs. However, some people may not notice any symptoms until the disease is more advanced and vision is affected.
Can diabetic retinopathy be cured?
While the damage from advanced retinopathy is often permanent, early detection and modern treatments — such as anti-VEGF injections or laser therapy — can halt progression and in some cases may recover some lost vision.
How often should people with diabetes have their eyes examined?
Adults and children aged 12 or older with diabetes should have comprehensive eye exams every year, even in the absence of symptoms. Early screening can detect changes before vision is affected.
What increases the risk of developing diabetic retinopathy?
Risk factors include:
- Poorly controlled blood sugar
- Long duration of diabetes (over 10 years)
- High blood pressure
- High cholesterol
- Smoking
Is diabetic retinopathy always bilateral (in both eyes)?
Yes, diabetic retinopathy usually affects both eyes, although one eye can be more affected than the other.
Take Action to Protect Your Vision
If you have diabetes, regular eye checks, good blood sugar control, and prompt attention to new vision changes give you the best chance of avoiding vision loss. Do not wait for symptoms to develop. Early intervention saves sight.
- See an eye care professional annually, or sooner if you notice any changes in vision.
- Report symptoms such as blurry vision, floaters, or trouble seeing in low light promptly.
- Adopt healthy lifestyle habits to reduce complications.
Summary Table: Key Points about Diabetic Retinopathy
| Aspect | Details |
|---|---|
| Earliest sign | Blurry vision or new floaters |
| When to screen | Yearly eye exam for all with diabetes age 12+ |
| Treatment options | Blood sugar control, anti-VEGF injections, laser, surgery |
| Progression risk | Increases with longer disease duration, poor sugar control |
| Vision restoration | Possible if treated early; less likely in advanced stages |
Resources
- Contact your diabetes care team or an eye specialist if you suspect vision changes.
- For urgent symptoms (sudden vision loss, significant increase in floaters), seek medical attention immediately.
- Learn more about managing diabetes and eye health through licensed health organizations and regular screenings.
References
- https://changeyegroup.com/warning-signs-of-diabetic-retinopathy-you-cant-afford-to-miss/
- https://www.universityhealth.com/blog/signs-of-diabetic-retinopathy
- https://www.nhs.uk/conditions/diabetic-retinopathy/
- https://www.healthline.com/health/diabetes/what-is-the-first-sign-of-diabetic-retinopathy
- https://utswmed.org/medblog/diabetic-eye-disease-how-spot-signs-early/
- https://www.mayoclinic.org/diseases-conditions/diabetic-retinopathy/symptoms-causes/syc-20371611
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/diabetic-retinopathy
- https://www.pennstatehealth.org/services-treatments/diabetic-retinopathy
Read full bio of medha deb












