How Eye Strain Influences Glaucoma: What You Need to Know
Understanding the connection between eye strain and glaucoma, and what it means for your vision health.
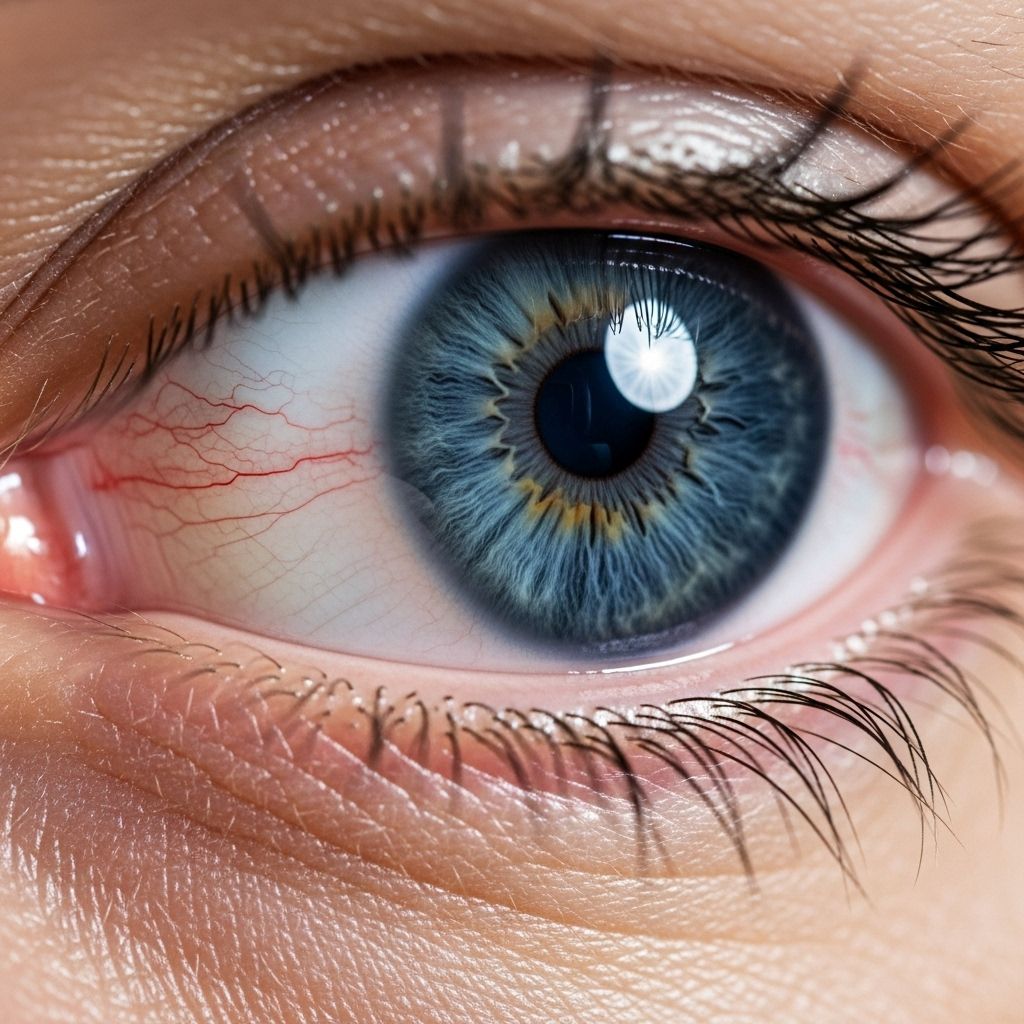
Glaucoma is a progressive eye disease that can lead to irreversible vision loss, primarily due to damage to the optic nerve caused by increased intraocular pressure. While many are aware of glaucoma’s risk factors, the potential role of eye strain has become an area of growing interest. Understanding this relationship is crucial for maintaining optimal eye health and preventing complications.
What Is Glaucoma?
Glaucoma is not a single disease but a group of conditions that damage the optic nerve, typically resulting from elevated pressure inside the eye (intraocular pressure or IOP). Over time, this pressure can hurt your vision, often beginning with peripheral (side) vision and leading to blindness if left untreated.
There are several types of glaucoma, including:
- Open-angle glaucoma: The most common form, where the drainage angle formed by the cornea and iris remains open, but the trabecular meshwork is partially blocked.
- Narrow-angle (or angle-closure) glaucoma: Occurs when the drainage angle closes or becomes very narrow, leading to rapid pressure buildup. This form is especially dangerous and can cause sudden vision loss if not treated immediately.
- Normal-tension glaucoma: Optic nerve damage occurs despite normal intraocular pressure, indicating that factors beyond eye pressure may play a role.
Glaucoma affects about 3 million Americans and is more common in certain groups, including individuals over 40, African Americans, East Asians, people with a family history, and those with other health risks.
Understanding Eye Strain
Eye strain (also known as asthenopia) describes a collection of symptoms that occur when the eyes are overworked, typically during prolonged focus on digital screens, reading, or other visually-demanding tasks. Symptoms include:
- Dry or watery eyes
- Blurred or double vision
- Headaches
- Eye discomfort or pain
- Difficulty concentrating
- Increased sensitivity to light
Modern lifestyles, dominated by smartphone and computer use, have led to increasing rates of eye strain. While eye strain itself is usually temporary, repeated episodes can exacerbate underlying eye conditions like glaucoma or contribute to their progression.
Can Eye Strain Affect Glaucoma?
While eye strain does not directly cause glaucoma, several mechanisms suggest that intense visual effort may impact eye health in those already at risk or with existing glaucoma:
- Increased intraocular pressure (IOP): Prolonged squinting, staring, or changes in body position can temporarily elevate eye pressure, which may be problematic for glaucoma patients.
- Reduced blood flow: Eye strain can lead to tension in eye muscles and vascular changes, potentially diminishing blood flow to the optic nerve and exacerbating optic nerve damage.
- Symptoms overlap: Some symptoms of glaucoma (such as blurry vision, headaches, and eye fatigue) can be mistaken for or intensified by eye strain, delaying proper diagnosis or management.
Individuals with glaucoma may also be more sensitive to eye strain, as chronic elevated eye pressure makes eyes more susceptible to stress and fatigue.
Symptoms: Eye Strain vs. Glaucoma
| Eye Strain | Glaucoma |
|---|---|
| Dry, tired eyes | Peripheral vision loss |
| Headaches, blurry vision | Elevated intraocular pressure (often silent) |
| Temporary discomfort | Possible eye pain, halos around lights in acute cases |
| Difficulty focusing, light sensitivity | Gradual, irreversible optic nerve damage |
| Usually resolves with rest | Requires ongoing medical management |
Risk Factors for Glaucoma
While anyone can develop glaucoma, several risk factors increase susceptibility:
- Family history: Genetics play a strong role.
- Age: People over 40 are at higher risk; risk increases with every decade.
- Ethnicity: African Americans are five times more likely to develop glaucoma than the general population; open-angle glaucoma is more common in this group, while East Asians are at higher risk for narrow-angle glaucoma.
- Medical conditions: Diabetes, high blood pressure, and certain eye injuries or chronic eye inflammation raise risk.
- Sex: Women are more susceptible to narrow-angle glaucoma than men.
How Digital Eye Strain May Interact with Glaucoma
Because much of modern life involves long hours spent on screens, digital eye strain has become widespread. There are several ways this may interact with glaucoma:
- Screen glare and focusing effort: Extended computer use forces the eyes to focus repeatedly at a fixed distance, which can increase muscular tension around the eye and elevate pressure.
- Reduced blinking: Staring at screens reduces blink rate, leading to dry eyes and aggravating symptoms in glaucoma patients.
- Poor ergonomics: Unsuitable environments (improper lighting, bad posture) further increase the risk of both eye strain and elevated IOP.
- Delayed detection: Overlapping symptoms may mask the early warning signs of glaucoma, postponing diagnosis and treatment.
Acute Angle-Closure Glaucoma and Eye Strain
While acute angle-closure glaucoma is rare, its relationship with eye strain is critical. This form of glaucoma develops when the drainage angle between the iris and cornea suddenly closes, leading to a rapid increase in eye pressure.
- Symptoms are severe and sudden: Intense, one-sided eye pain, nausea, vomiting, headache, blurred vision, and halos around lights.
- Requires urgent treatment: Left unchecked, it can lead to permanent vision loss within hours.
- Can be triggered by certain activities: Prolonged reading in poor lighting, stress, and drug-induced changes to pupil size may increase risk.
Protecting Your Eyes: Practical Tips
Whether you have glaucoma, are at risk, or want to safeguard your eyesight, consider these strategies:
- Schedule regular eye exams: Comprehensive exams, including optic nerve and eye pressure checks, are vital, especially for those over 40 or with risk factors.
- Manage screen time: Take frequent breaks using the 20-20-20 rule (every 20 minutes, look at something 20 feet away for 20 seconds).
- Optimize your environment: Use adequate lighting, reduce screen glare, and maintain good posture.
- Stay hydrated: Dry eyes exacerbate discomfort and may worsen glaucoma symptoms.
- Eat a balanced diet: Nutrients such as vitamins A, C, E, and minerals like zinc benefit eye health.
- Protect your eyes from injury: Wear sunglasses and goggles when appropriate.
- Don’t ignore symptoms: Seek prompt medical attention for persistent eye pain, sudden loss of vision, or other unexplained issues.
Managing Eye Strain When You Have Glaucoma
If you live with glaucoma, minimizing eye strain can help keep your vision stable and improve comfort:
- Use lubricating eye drops (prescribed or recommended by your doctor).
- Set reminders to rest your eyes throughout the day.
- Adjust device settings (brightness and contrast) for easier viewing.
- Wear prescription glasses or corrective lenses if needed.
- Practice stress reduction: Mindfulness and relaxation exercises can reduce tension affecting eyes.
- Avoid over-the-counter medications that may elevate eye pressure (consult your eye doctor).
Diagnosis and Treatment of Glaucoma
Early diagnosis is paramount. A comprehensive eye exam for glaucoma includes:
- Tonometry: Measuring intraocular pressure.
- Ophthalmoscopy: Examining the optic nerve for damage.
- Perimetry (visual field test): Assessing peripheral vision.
- Gonioscopy: Checking the angle where the iris meets the cornea to determine drainage efficiency.
Treatment options may include:
- Medicated eye drops: To lower IOP.
- Laser therapy: Improves fluid drainage.
- Surgery: In severe cases, to create new drainage channels.
- Lifestyle adjustments: Managing blood pressure and overall health supports eye function.
Frequently Asked Questions (FAQs)
Q: Does eye strain cause glaucoma?
A: No, eye strain by itself does not cause glaucoma. However, increased stress on the eyes may temporarily elevate pressure and worsen symptoms in those already at risk or living with the disease.
Q: Can screen time lead to glaucoma?
A: There is no direct evidence that screen use causes glaucoma. Extended screen time can lead to eye strain, which may contribute to discomfort and symptom overlap in glaucoma patients.
Q: What are the earliest signs of glaucoma?
A: Open-angle glaucoma often develops silently, with peripheral vision loss occurring before central signs. Acute angle-closure glaucoma causes severe pain, blurry vision, and halos around lights.
Q: How often should I get my eyes checked?
A: Adults over age 40 should have comprehensive eye exams every 1–2 years, or more frequently if at higher risk due to health conditions or family history.
Q: How can I reduce eye strain daily?
A: Take regular breaks, use screens at comfortable brightness, maintain good posture, hydrate, and practice stress-reduction techniques. Consider blue light filters and ensure your workspace is well-lit.
Key Takeaways
- Eye strain does not directly cause glaucoma, but can worsen symptoms in those at risk.
- Glaucoma is a serious condition; early detection and treatment prevent irreversible vision loss.
- Regular eye exams and lifestyle choices, including managing screen time and stress, help safeguard eye health.
- If you notice changes in vision or experience severe eye pain, seek medical attention immediately.
References and Prevention Tips
- Follow the advice of your ophthalmologist and schedule routine checks.
- Manage systemic health conditions (diabetes, blood pressure) for optimal eye support.
- Eat nutrient-rich foods and avoid smoking.
- Practice safe habits: wear protective eyewear in risky situations.
- Educate yourself about glaucoma risk and advocate for eye health in your community.
By understanding the interplay between eye strain and glaucoma, individuals can make informed decisions, pursue timely medical care, and maintain healthy vision throughout life.
References
- https://www.medicalnewstoday.com/articles/narrow-angle-glaucoma
- https://californiahealthline.org/news/article/eye-health-glaucoma-asking-never-hurts/
- https://www.healthlinedme.com/Resource-Center/Medical-Health-Issues?issue=Glaucoma&id=246
- https://www.medicalnewstoday.com/articles/foods-to-avoid-if-you-have-glaucoma
- https://www.healthline.com/health/eye-health/eye-strain
- https://www.healthline.com/health/video/how-to-get-rid-of-bags-under-eyes
- https://www.webmd.com/eye-health/good-eyesight
- https://www.youtube.com/watch?v=o68WOH-qGC0
Read full bio of medha deb












