Eye Injections for Diabetic Retinopathy: Benefits, Process, and What to Expect
A comprehensive guide to eye injections for diabetes: benefits, procedure, risks, and frequently asked questions.
Diabetes-related eye complications are a major cause of vision impairment and blindness. In recent years, eye injections—specifically, intravitreal injections—have become a cornerstone in treating vision-threatening diabetic eye diseases. This comprehensive guide explores how these injections work, their potential benefits and risks, the typical procedure, and answers to common patient questions.
Understanding Diabetic Eye Disease
Diabetic eye disease primarily refers to conditions caused by long-term uncontrolled blood sugar, such as:
- Diabetic retinopathy: Damage to the retina due to leaking or abnormal blood vessels.
- Diabetic macular edema (DME): Swelling in a critical part of the retina (the macula) responsible for central vision.
These conditions often do not cause symptoms until they are advanced, making regular screening vital for those with diabetes.
Why Are Eye Injections Used for Diabetic Eye Disease?
Eye injections provide a targeted approach, delivering medication directly into the eye’s vitreous—a gel-like center. This allows high concentrations of medicine to reach affected retinal tissue, offering several key advantages:
- Local, precise therapy: Minimizes systemic (whole-body) side effects because medication is not spread throughout the body.
- Direct action on the retina: Especially important for halting blood vessel leakage and abnormal growth.
- Potential for vision stabilization and improvement: Many patients experience slowed disease progression, and some see measurable visual improvement.
Types of Eye Injections for Diabetic Retinopathy
Several kinds of medications might be injected directly into the eye to address diabetic complications:
Anti-VEGF Injections
Anti-vascular endothelial growth factor (anti-VEGF) drugs are the most common class. VEGF is a protein that stimulates abnormal blood vessel growth and leakage—key problems in diabetic retinopathy and DME. Blocking VEGF can reduce swelling, stop progression, and occasionally improve vision. The main anti-VEGF drugs used include:
- Bevacizumab (Avastin)
- Ranibizumab (Lucentis)
- Aflibercept (Eylea)
- Brolucizumab (Beovu)
- Faricimab (Vabysmo)
These medications are typically the first-line treatment for DME and most proliferative forms of diabetic retinopathy.
Steroid (Corticosteroid) Injections
In some cases, ophthalmologists may recommend steroid injections, especially when anti-VEGF therapy is not effective or suitable. Common steroids used include Triamcinolone, Ozurdex, and Iluvien. These injections:
- Reduce retinal swelling and inflammation.
- May be chosen for certain patients, but carry a risk of increased eye pressure and cataract development.
How Do Eye Injections Work?
Both anti-VEGF and steroid medications:
- Target specific eye problems (abnormal blood vessel growth, leakage, swelling).
- Slow or even stop vision loss by stabilizing or improving retinal thickness and function.
- May require repeat (often monthly) injections for optimal control, depending on individual response.
Research consistently shows that these injections, when started early and continued as indicated, can substantially reduce the risk of severe vision loss in people with diabetic retinopathy.
Effectiveness of Eye Injections for Diabetic Eye Disease
Key evidence highlights:
- Large-scale clinical trials confirm that anti-VEGF therapies and steroids effectively reduce retinal swelling and improve (or stabilize) vision in many patients.
- Patients receiving regular, appropriately-timed injections see a significantly slower rate of disease progression and less severe vision loss compared to those not receiving treatment.
- Some patients report improved visual sharpness and greater quality of life as swelling resolves and retinal function improves.
However, it is essential to note that while injections can halt or slow down vision loss, they are rarely a “cure.” Ongoing diabetes management and eye monitoring remain crucial.
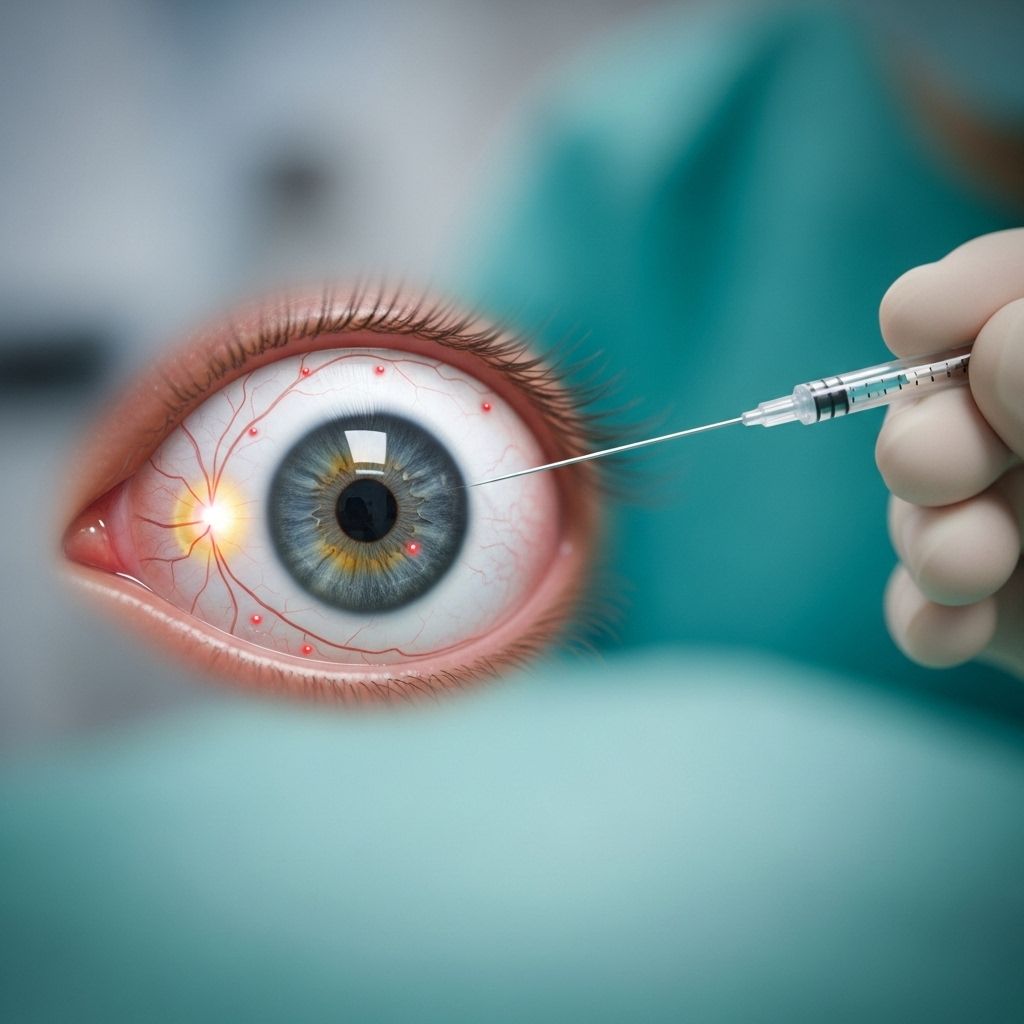
The Eye Injection Procedure: What to Expect
Though the idea of an eye injection may seem daunting, the process is generally quick, minimally painful, and performed in an ophthalmologist’s office:
- Preparation: Your eye and surrounding skin will be cleaned to reduce infection risk. Anesthetic (numbing) drops will be applied.
- Stabilization: A small device or gentle tape may be used to keep your eyelids open.
- The Injection: The eye doctor guides a tiny needle into the white part of your eye (the sclera), delivering the medication into the vitreous gel.
- Duration: The procedure typically finishes in less than 10 minutes.
- Aftercare: You may be monitored briefly for discomfort or complications. Most people resume normal activities within hours.
Will it hurt?
The numbing drops and gentle approach make the procedure nearly painless for most people. You may feel slight pressure, but severe pain is uncommon. Afterwards, some people experience mild irritation, redness, or a sensation of having something in their eye; this typically resolves in a day or two.
Benefits of Eye Injections for Diabetes-Related Eye Disease
Intravitreal injections offer several important benefits in the management of diabetic eye conditions:
- Targeted treatment: Medication is delivered precisely to the affected area, limiting whole-body side effects.
- Prevention of severe complications: Early and appropriate use may prevent progression to advanced diabetic eye disease, retinal detachment or permanent vision loss.
- Potential vision improvement: For some, vision stabilizes or improves, particularly if treated before extensive retinal damage.
- Outpatient, fast recovery: Treatments are performed in-office, with minimal impact on daily activities.
Risks and Side Effects
Like all medical procedures, eye injections carry potential risks. Most complications are mild, but it’s important to recognize and report any symptoms to your eye care team:
- Mild side effects (common):
- Eye redness or irritation
- Watery eyes or mild discomfort
- Temporary blurriness
- Rare but serious complications:
- Eye infection (endophthalmitis)
- Increased eye pressure (especially with steroids)
- Retinal detachment
- Bleeding inside the eye
Your doctor will monitor carefully for these side effects during regular follow-up visits. Prompt reporting of severe pain, vision loss, or intense redness is essential for early management.
How Often Will I Need Eye Injections?
The frequency of injections depends on:
- The specific medication being used
- How quickly your eye disease is responding
- Any side effects experienced
Many patients start with injections every four to six weeks, then “space out” as the retina stabilizes. Some may need ongoing maintenance injections for months or years, while others can eventually stop. Your ophthalmologist will develop an individualized treatment plan.
Additional Treatments for Diabetic Eye Disease
While eye injections are highly effective, they may be combined with other interventions for optimal results, including:
- Laser therapy (photocoagulation): Seals leaking blood vessels or reduces abnormal vessel growth.
- Surgery: Used for severe bleeding (vitrectomy) or retinal detachment.
- Optimal diabetes management: Blood sugar, blood pressure, and cholesterol control remain fundamental.
These treatments are complementary, and your eye care team will recommend a holistic approach tailored to your needs.
Preparing for Your Eye Injection Visit
- Arrange for transportation, especially if your vision may be blurry immediately after the appointment.
- Bring a list of all medications and supplements.
- Mention any history of allergies or medication reactions.
- Ask any questions you may have, and share your concerns or fears with your care team—they’re there to help.
Frequently Asked Questions (FAQs)
Q: Are eye injections safe long-term?
Yes, extensive clinical research and long-term use have shown anti-VEGF and steroid injections to be generally safe when performed by qualified eye specialists. The risk of significant side effects, such as infection or retinal detachment, is low but real; that’s why ongoing monitoring is required.
Q: Will the injections restore lost vision?
While eye injections can prevent further vision loss and, in some cases, improve vision, they cannot always reverse damage that has already occurred, especially if the disease is advanced. Early detection and intervention provide the best chances for preserving sight.
Q: Do the injections hurt?
The procedure uses numbing drops and is usually well tolerated. Most people report only mild pressure or brief discomfort. Severe pain during or after the procedure is uncommon and should prompt immediate medical attention.
Q: How quickly will I notice improvements?
Many people experience some improvement or stabilization after a few injections, but this varies significantly. Your eye doctor will regularly monitor your progress to determine the best ongoing treatment strategy.
Q: What if I miss a scheduled injection?
Missing an injection may allow the disease to progress and worsen vision problems. Notify your doctor if you cannot make a scheduled visit, so a new appointment can be arranged promptly.
Q: Can eye injections be combined with other treatments?
Absolutely. Eye injections are frequently combined with laser therapy, surgery, and optimized systemic management of diabetes for maximum effectiveness.
Summary Table: Anti-VEGF vs. Steroid Eye Injections
| Feature | Anti-VEGF Injections | Steroid Injections |
|---|---|---|
| Primary Use | First-line for DME, proliferative retinopathy | When anti-VEGF is inadequate or not tolerated |
| Common Medications | Avastin, Lucentis, Eylea, Beovu, Vabysmo | Triamcinolone, Ozurdex, Iluvien |
| Benefits | Proven to reduce swelling, slow disease, improve/stabilize vision | Effective at reducing inflammation & macular edema |
| Main Risks | Low risk of infection, mild discomfort | Increased eye pressure, cataract risk, infection |
| Treatment Schedule | Often monthly, may be spaced out with improvement | Often less frequent, depending on response |
Key Takeaways
- Eye injections are a highly effective, research-backed option for preserving vision in diabetic retinopathy and DME.
- Anti-VEGF medications are the most commonly used, with steroids reserved for specific cases.
- The procedure is quick, minimally painful, and performed in an office setting.
- Regular follow-up and communication with your eye doctor are crucial for safe, effective treatment.
- Managing blood sugar, blood pressure, and cholesterol remains fundamental alongside eye injections.
When to Contact Your Eye Doctor
If you experience any of the following after an injection, contact your ophthalmologist promptly:
- Increased vision loss or severe vision changes
- Severe or increasing eye pain
- Persistent redness or swelling
- Flashes of light, new floaters, or curtain-like vision changes (possible signs of retinal detachment)
Final Words
Diabetic retinopathy and macular edema are serious, but timely use of eye injections offers real hope for preserving vision and protecting quality of life. If you have diabetes, regular eye exams and early intervention are the keys to lifelong eye health. Speak with your retina specialist about your individual needs and concerns—there are effective treatments available, and a personalized care plan can make all the difference.
References
- https://www.retinaeyecenter.com/blog/understanding-retinal-injections-for-diabetic-eye-disease-what-to-expect
- https://resources.healthgrades.com/right-care/eye-health/what-to-expect-with-eye-injections-for-diabetic-retinopathy
- https://www.willseye.org/diabetic-retinopathy-treatment/
- https://www.gulfcoastretinacenter.com/blog/the-benefits-of-intravitreal-injections-saving-sight-and-improving-vision.html
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/diabetic-retinopathy/injections-treat-eye-conditions
- https://midatlanticretina.com/2023/03/16/eye-injections-for-diabetic-retinopathy/
- https://www.mdfoundation.com.au/about-macular-disease/diabetic-eye-disease/treatment-for-diabetic-retinopathy/
- https://www.nhs.uk/conditions/diabetic-retinopathy/
- https://www.asrs.org/patients/retinal-diseases/33/intravitreal-injections
Read full bio of Sneha Tete












