Eye Floaters and Detached Retina: Symptoms, Risks, and Treatments
Identify early signs of retinal detachment and eye floaters to protect your vision and prevent severe complications.
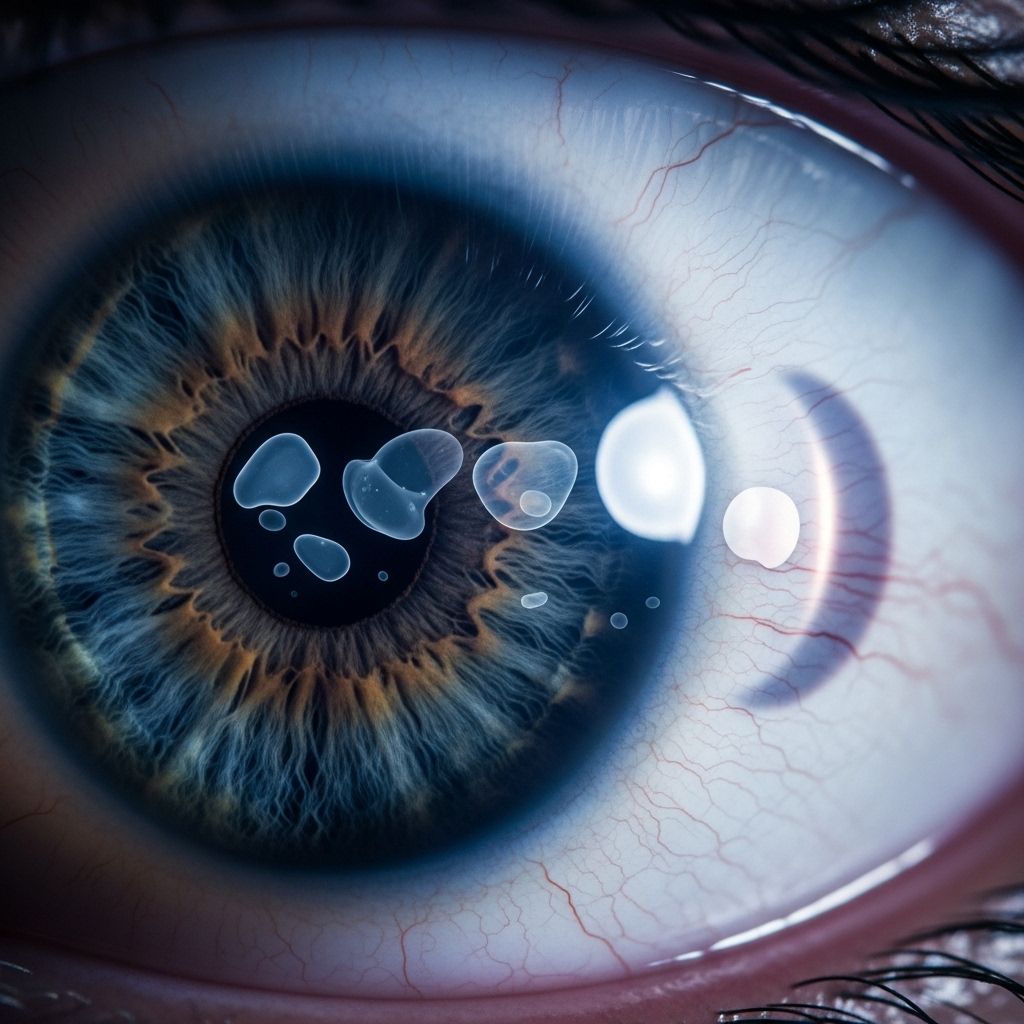
Eye floaters are a frequent visual phenomenon characterized by tiny specks, spots, or cobweb-like shapes drifting across the field of vision. While often harmless, a sudden increase in floaters, especially when accompanied by flashes of light or vision loss, can signal a medical emergency: retinal detachment. Understanding the differences, symptoms, risks, and treatment options for eye floaters and detached retina is crucial for preserving vision.
What Are Eye Floaters?
Eye floaters are small, shadowy shapes that move across your field of vision. They are most visible when looking at something bright, such as a clear sky or a white wall.
- Commonly appear as dots, lines, threads, cobwebs, or rings.
- Caused by tiny pieces of debris in the vitreous humor, the gel-like material inside the eye, casting shadows on the retina.
- Most floaters are harmless and are a natural part of aging.
- Some people may rarely notice them, while others see them regularly.
When Should Eye Floaters Be a Concern?
While floaters alone are usually not cause for alarm, you should seek immediate medical attention if you experience:
- A sudden increase in floaters, especially resembling a shower or swarm of new spots.
- Flashes of light (photopsia) in one or both eyes.
- A shadow or curtain effect descending over part of your vision.
- Loss of peripheral (side) vision or blurry vision.
These could be symptoms of a retinal tear or detachment—an urgent condition that can lead to permanent vision loss if not treated rapidly.
Understanding Retinal Detachment
Retinal detachment occurs when the retina—the thin, light-sensitive tissue at the back of the eye—pulls away from its normal position. Once detached from its nourishing blood supply, the retina cannot function correctly, putting your sight at risk.
| Aspect | Details |
|---|---|
| Definition | Separation of the retina from the underlying layer of blood vessels |
| Urgency | Medical emergency requiring immediate care |
| Potential Outcome | Permanent vision loss or blindness if left untreated |
Symptoms of Retinal Detachment
- Sudden appearance of new floaters (dark spots, lines, or shapes)
- Flashes of light in one or both eyes
- Shadow or curtain effect over part of the visual field (can be peripheral or central)
- Blurry or reduced vision
- Loss of vision in the affected area
Note: A detached retina is generally painless, but its symptoms often develop quickly.
What Causes Eye Floaters and Retinal Detachment?
Common Causes of Eye Floaters
- Age-related changes: As people age, the vitreous humor can liquefy and shrink, causing clumps or strands to form.
- Posterior vitreous detachment (PVD): The vitreous gel pulls away from the retina, sometimes causing floaters or flashes.
- Other factors: Inflammation, bleeding within the eye, eye injury, or previous eye surgery.
Causes of Retinal Detachment
- Retinal tears or holes: Often related to vitreous shrinkage, which pulls and tears the retina.
- Fluid accumulation: Fluid leaks through a retinal tear, collecting under the retina and lifting it away from the underlying tissue.
- Scar tissue: Scar tissue on the retina’s surface (from injury, diabetes, or inflammation) may contract and pull the retina from the back of the eye.
Who Is at Risk for Retinal Detachment?
Anyone can develop a detached retina, but certain factors increase risk:
- History of retinal detachment in either eye
- Family history of retinal detachment
- Severe nearsightedness (myopia)
- Previous eye surgery (especially cataract removal)
- History of serious eye injury or trauma
- Other eye conditions:
- Diabetic retinopathy
- Posterior vitreous detachment
- Retinoschisis (retinal splitting)
- Lattice degeneration (thinning of the retina)
How Are Retinal Detachment and Floaters Diagnosed?
If you experience sudden changes in vision, your eye doctor (ophthalmologist) will conduct a comprehensive eye exam, which may include:
- Review of medical and vision history
- Visual acuity tests (measuring sharpness of vision)
- Peripheral (side) vision assessment
- Examination with dilated pupils (for a clear view of the retina)
- Use of an ophthalmoscope or slit lamp to closely examine the retina for tears or detachment
- Eye ultrasound if the eye cannot be fully examined due to cloudiness, small pupils, or bleeding
Treatment Options for Retinal Detachment
Treatment depends on the type, location, and severity of the detachment. Prompt intervention is essential to restore vision and prevent permanent loss.
- Scleral Buckling: A tiny silicone band is attached to the outside of the eye (sclera), gently pushing it toward the detached retina. Fluid may be drained before placing the band to allow the retina to settle back in position.
- Pneumatic Retinopexy: A gas bubble is injected into the vitreous, pressing the retina against the wall of the eye. The patient positions their head to keep the bubble in place as the retina reattaches. Often used for smaller, uncomplicated detachments.
- Vitrectomy: The vitreous gel is removed and replaced with a gas bubble or silicone oil. This method is often used for more complex or larger detachments.
- Cryotherapy: Uses extreme cold to seal retinal tears or holes with scar tissue.
- Laser Photocoagulation: Focuses a laser to create small burns around a retinal tear, forming scarring that helps reattach the retina.
Often, a combination of these techniques may be used for best outcomes. Follow-up visits are crucial to monitor healing and catch any recurrence.
Treatment for Eye Floaters
Most floaters do not require treatment unless they significantly impair vision or result from serious eye conditions. Treatment options include:
- Observation: Regular monitoring unless symptoms worsen or new floaters appear suddenly.
- Vitrectomy (rare): Surgical removal of the vitreous may be considered for severe, persistent floaters.
However, most eye doctors advise against surgery unless floaters are extremely disturbing, as the risks may outweigh the benefits.
Prevention and Early Detection
While you can’t always prevent retinal detachment, you can reduce your risk and best preserve your sight through:
- Regular comprehensive eye exams—especially if you are at higher risk
- Promptly reporting changes in vision, new floaters, or flashes to your eye doctor
- Protecting eyes from injury by wearing appropriate safety eyewear during sports or risky activities
- Managing systemic diseases such as diabetes
- Avoiding eye trauma as much as possible
Living With Floaters or After Detached Retina Treatment
For most people, floaters tend to become less bothersome over time as the brain adapts and learns to ignore them. However, if you have undergone treatment for a retinal detachment:
- Follow your ophthalmologist’s instructions carefully.
- Attend all recommended follow-up visits.
- Watch for symptoms in the other eye—those with one affected eye are at increased risk in the other.
- Avoid heavy lifting, straining, or activities that can cause eye injury during recovery.
Frequently Asked Questions (FAQs)
What is the difference between an eye floater and a sign of retinal detachment?
Eye floaters are typically harmless and part of normal aging. However, a sudden burst of floaters, especially with flashes of light or vision loss, can signal a retinal tear or detachment—a medical emergency requiring immediate care.
Can retinal detachment cause blindness?
Yes, if left untreated, retinal detachment can result in permanent vision loss or blindness. Rapid intervention significantly improves the chance of saving vision.
Are there ways to reduce the risk of detached retina?
Although you can’t control all risk factors, regular eye exams, protecting your eyes from injury, controlling blood sugar in diabetes, and being vigilant about new symptoms help lower your risk or ensure early detection.
Is retinal detachment painful?
No, retinal detachment is generally painless. The most common signs are sudden changes in vision, floaters, flashes, or a curtain-like shadow.
What should I do if I suddenly notice a large number of floaters or flashes?
Seek urgent medical attention from an eye doctor or go to the emergency room. Quick diagnosis and treatment are crucial to saving sight.
Key Takeaways
- Sudden vision changes—like a burst of floaters, flashes, or vision loss—demand immediate attention.
- Retinal detachment is a medical emergency but prompt treatment can prevent permanent damage.
- Regular eye exams and understanding your risk factors are the best prevention.
- Monitor your vision, especially if you have a personal or family history of eye problems, diabetes, or severe nearsightedness.
References
- https://www.health.harvard.edu/diseases-and-conditions/detached-retina-a-to-z
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/retinal-detachment
- https://www.mayoclinic.org/diseases-conditions/retinal-detachment/symptoms-causes/syc-20351344
- https://www.healthline.com/health/eye-floaters
- https://www.medicalnewstoday.com/articles/325781
- https://www.ncbi.nlm.nih.gov/books/NBK470420/
- https://my.clevelandclinic.org/health/symptoms/14209-eye-floaters-myodesopias
- https://www.eurekahealth.com/resources/what-does-it-mean-when-you-see-floaters-en
Read full bio of medha deb












