Understanding Eustachian Tube Dysfunction: Causes, Symptoms, and Effective Treatments
Learn about Eustachian tube dysfunction, its symptoms, causes, diagnosis, and current treatment options for better ear health.
Eustachian tube dysfunction (ETD) is a common yet often misunderstood condition that affects the passageways connecting the middle ear and the upper throat. It can result in a variety of symptoms, ranging from mild discomfort to severe hearing issues and persistent ear pain. This comprehensive article provides an in-depth exploration of ETD, its causes, symptoms, diagnosis, and the most current treatment approaches available. By understanding ETD, individuals can seek timely care and adopt strategies to manage symptoms effectively.
What Is Eustachian Tube Dysfunction?
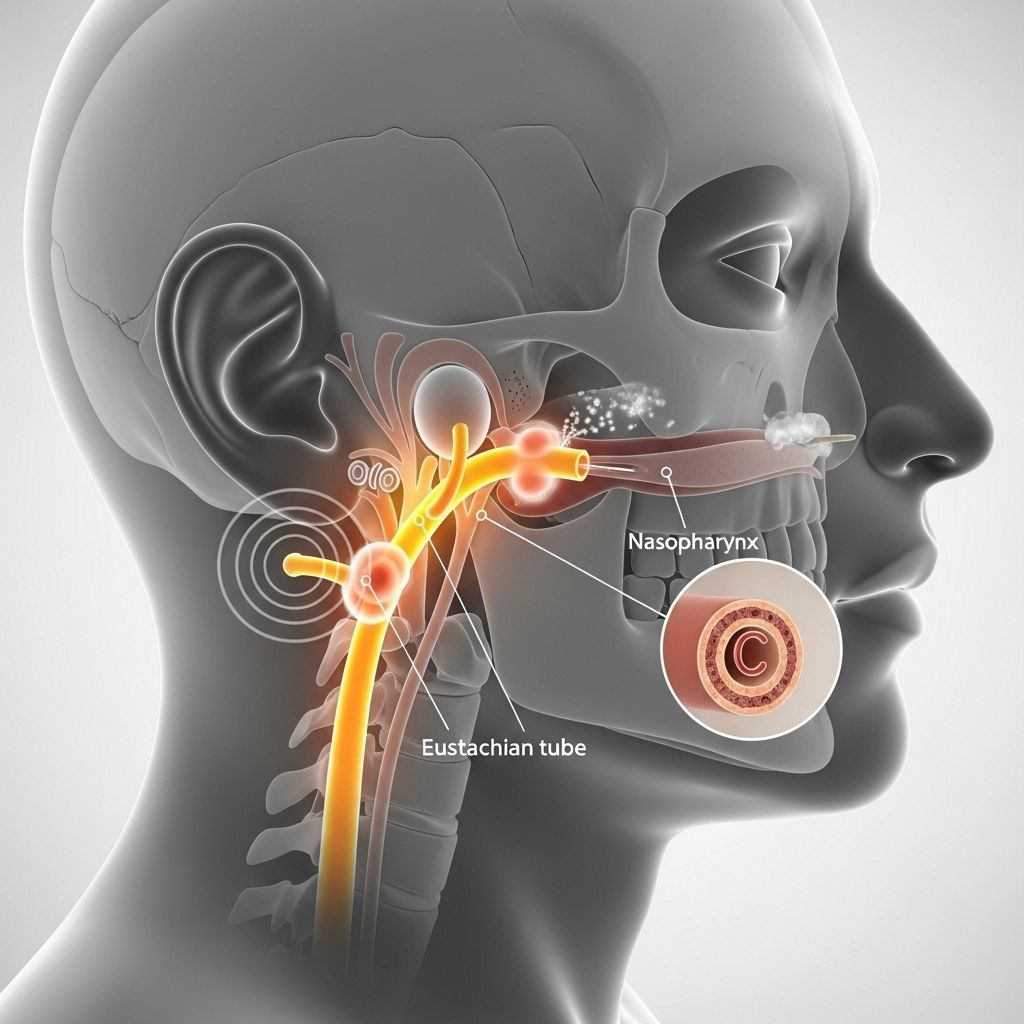
The eustachian tubes are slender canals that connect the middle ear to the back of the nose and upper throat (nasopharynx). Their primary functions include equalizing air pressure across the eardrum, draining fluid from the middle ear, and protecting the ear from nasopharyngeal secretions and sound pressures. Eustachian tube dysfunction occurs when these tubes become blocked, inflamed, or fail to open properly, resulting in abnormal pressure and fluid buildup in the ear.
- Normal eustachian tube function allows the ear to adapt to changes in external pressure—such as during flying, climbing elevations, or diving.
- Dysfunction prevents adequate pressure equalization and drainage, resulting in discomfort or hearing issues.
Symptoms of Eustachian Tube Dysfunction
ETD can present differently across individuals, but several symptoms are common. These symptoms may range from mild irritation to more pronounced problems and can be persistent or intermittent.
- Fullness or pressure sensation in the ears
- Pain or discomfort, often felt during altitude changes
- Feeling as if ears “need to pop”
- Muffled hearing or partial hearing loss in one or both ears
- Popping, clicking, or crackling sounds inside the ear, especially when swallowing or yawning
- Mild imbalance or feeling off-balance
- Ringing in the ears (tinnitus), which may become more noticeable
- Episodes of vertigo or dizziness in some cases
Severe or prolonged ETD may lead to:
- Chronic ear pain
- Recurring ear infections (otitis media)
- Permanent damage or changes to the eardrum, including possible perforation
Causes of Eustachian Tube Dysfunction
Many factors can contribute to eustachian tube dysfunction, often acting together to cause symptoms. The most frequent causes include:
- Allergies: Allergic reactions leading to swelling and congestion in the nasal passages can block the eustachian tubes.
- Upper respiratory infections: Colds, sinus infections, and flu can increase mucus production and swelling.
- Sinusitis: Chronic or acute sinus inflammation is a key trigger for ETD.
- Rapid changes in altitude: Traveling by airplane, mountain climbing, or scuba diving may disturb normal pressure equalization.
- Gastroesophageal reflux disease (GERD): Chronic acid reflux may cause inflammation around the eustachian tubes.
- Structural problems: Enlarged adenoids, tumors, or anatomical abnormalities can directly block the tubes.
- Chronic nasal congestion: Environmental irritants, smoke exposure, or prolonged colds can cause ongoing symptoms.
Who Is at Risk?
While ETD can affect anyone, certain populations are at greater risk:
- Children: Children’s eustachian tubes are shorter, narrower, and more horizontally oriented, making them prone to blockage and dysfunction.
- Individuals with allergies or frequent sinus infections: These conditions increase the likelihood of ETD.
- Divers and frequent flyers: Activities involving rapid pressure changes raise the risk.
- People exposed to tobacco smoke: Smoke irritates nasal tissues, exacerbating inflammation.
- Individuals with weakened immune systems: Conditions or medications that reduce immune function can also increase susceptibility.
How Is Eustachian Tube Dysfunction Diagnosed?
A comprehensive diagnosis involves both a medical history and physical examination conducted by a healthcare provider, usually an ear, nose, and throat (ENT) specialist.
- The provider will discuss your symptoms, including the onset, duration, and triggers.
- A physical exam will include visual inspection of the ear canals and eardrums, nasal passages, and the back of the throat.
- In some cases, additional tests may be ordered, such as tympanometry, hearing tests (audiometry), or imaging studies if anatomical blockage is suspected.
It is important to seek a professional diagnosis for persistent or severe symptoms to rule out other causes of ear pain and hearing loss and to determine the most appropriate treatment.
Treatment Options for Eustachian Tube Dysfunction
Treatment for ETD depends on the underlying cause, symptom severity, and whether symptoms are acute or chronic. In many cases, symptoms resolve on their own and do not require medical intervention. However, when symptoms are persistent or severe, several approaches may be employed.
Self-Care and Home Remedies
- Swallowing, yawning, or chewing gum: These actions help activate the muscles that open the eustachian tubes.
- Valsalva maneuver: Take a deep breath, pinch your nostrils shut, and gently “blow” without letting air out. This can help equalize pressure.
- Steam inhalation: Breathing in moist air may thin mucus and relieve congestion.
- For infants: Feeding or providing a pacifier can stimulate the swallowing reflex, helping to open the tubes.
Medical and Pharmacologic Treatments
- Decongestants: Oral or nasal decongestants may reduce nasal and tube swelling in acute cases.
- Antihistamines and corticosteroid nasal sprays: Prescribed for patients with allergic triggers to reduce inflammation.
- Pain relievers: May provide temporary relief for discomfort.
Note: The use of medication—especially in children—should always follow professional guidance.
Procedural and Surgical Interventions
For symptoms that persist despite conservative treatments, or when fluid retention is causing significant hearing loss or recurrent infection, procedural approaches may be recommended:
- Myringotomy: A tiny incision is made in the eardrum to drain fluid. The eardrum typically heals within a few days.
- Insertion of ear tubes (tympanostomy tubes): Small tubes are placed in the eardrums to allow fluid drainage and pressure equalization. These are often used in children with recurrent ear infections and remain in place for up to 18 months before falling out on their own.
- Balloon eustachian tuboplasty (balloon dilation): A thin catheter with a small balloon is inserted through the nose into the eustachian tube. The balloon is inflated to open the passage, allowing mucus and air to flow more freely, then removed.
- Treatment of underlying sinus or nasal obstruction: Addressing nasal polyps, chronic sinusitis, or adenoid hypertrophy may relieve ETD.
Important Warning: Avoid Ear Candling
The U.S. Food and Drug Administration (FDA) strongly advises against using ear candles—an alternative therapy that involves inserting a hollow candle into the ear canal. There is no scientific evidence supporting their effectiveness, and they pose serious risks, including burns and ear damage.
When Should You Seek Medical Advice?
Although many cases of ETD resolve on their own, you should consult a healthcare provider if:
- Symptoms persist for more than two weeks
- You experience severe ear pain, hearing loss, or fluid drainage from the ear
- There are symptoms of infection: fever, redness, or swelling around the ear
- Problems start after head trauma or severe upper respiratory infection
Timely intervention can help prevent permanent hearing loss or damage to the eardrum.
Can Eustachian Tube Dysfunction Be Prevented?
Prevention strategies largely revolve around reducing the risk of nasal congestion or infection and managing allergy symptoms. Strategies may include:
- Treating seasonal allergies with prescribed medication or avoiding known triggers
- Practicing good hand hygiene to reduce respiratory infection risk
- Avoiding smoking and exposure to secondhand smoke
- Using saline nasal sprays to keep nasal passages and eustachian tubes clear
For travelers, practicing pressure-equalizing actions during ascent and descent, staying well-hydrated, and using decongestant sprays (with professional guidance) before flights may minimize symptoms.
Living with Eustachian Tube Dysfunction
Most people with mild ETD can manage symptoms with lifestyle strategies and occasional use of over-the-counter medications. Chronic or severe cases may require long-term management or specialist interventions. Maintaining regular follow-up with an ENT specialist can optimize outcomes and reduce the risk of complications.
Frequently Asked Questions (FAQs)
What does eustachian tube dysfunction feel like?
It often feels like pressure or fullness in the ears, muffled hearing, or as if the ears need to “pop.” These sensations may be accompanied by discomfort, clicking, or crackling sounds.
Can eustachian tube dysfunction cause hearing loss?
Yes, muffled hearing and temporary hearing loss are common, especially if fluid accumulates in the middle ear. Permanent hearing loss is rare but can occur if the condition is left untreated for long periods.
What is the best treatment for eustachian tube dysfunction?
Treatment depends on the cause and severity. Many cases resolve with simple actions like swallowing or yawning. Persistent symptoms may need medication or procedural interventions such as ear tubes or balloon dilation.
Are children more at risk of eustachian tube dysfunction?
Yes, due to anatomical differences, children are more prone to eustachian tube blockages. This is why recurrent ear infections and fluid in the ears are more common in young children.
How long does it take for eustachian tube dysfunction to go away?
Symptoms often resolve within a few days to a couple of weeks. Prolonged or severe cases should be evaluated by a healthcare provider.
Table: Comparison of Treatment Options
| Treatment Method | How It Works | Ideal For | Potential Risks |
|---|---|---|---|
| Swallowing, yawning, chewing gum | Muscle activation opens tubes | Mild, brief symptoms | Minimal to none |
| Valsalva maneuver | Equalizes ear pressure through forced exhalation | Acute or altitude-related symptoms | Rarely, can cause dizziness |
| Decongestants & antihistamines | Reduce swelling and congestion | Allergy-related or infection-related symptoms | Side effects (dry mouth, insomnia) |
| Myringotomy and ear tubes | Drains fluid; ventilates middle ear | Chronic/recurrent ETD or infections | Infection, persistent perforation |
| Balloon dilation | Physically opens and expands the tube | Refractory, chronic ETD | Nasal bleeding, rare complications |
Key Takeaways
- Eustachian tube dysfunction is a common cause of ear pressure, discomfort, and muffled hearing.
- Most cases resolve with simple self-care measures; persistent or severe symptoms require medical evaluation.
- Treatment options are tailored to causative factors and may range from medication to surgical procedures.
- Prevention and early intervention help reduce the risk of complications.
Further Resources
- Consult an otolaryngologist (ENT specialist) for persistent ear issues.
- American Academy of Otolaryngology—Head and Neck Surgery information on ear health.
- Stay updated with FDA advisories regarding ear treatment methods.
References
- https://sinuscenterok.com/eustachian-tube-dysfunction/
- https://familydoctor.org/condition/eustachian-tube-dysfunction/
- https://www.ent-sd.com/ent-medical-treatments-san-diego/ears-hearing/eustachian-tube-dysfunction/
- https://my.clevelandclinic.org/health/diseases/22527-eustachian-tube-dysfunction
- https://patient.info/ears-nose-throat-mouth/earache-ear-pain/eustachian-tube-dysfunction
- https://www.ncbi.nlm.nih.gov/books/NBK262265/
- https://mmment.com/services/ear-nose-throat-care/ear/eustachian-tube-dysfunction/
- https://med.stanford.edu/ohns/OHNS-healthcare/earinstitute/conditions-we-treat/eustachian-tube-dysfunction.html
- https://www.brighamandwomens.org/surgery/otolaryngology/ear/eustachian-tube-dysfunction
Read full bio of Sneha Tete












