Innovative Procedures for Eustachian Tube Dysfunction: Advances in Balloon Dilation
Minimally invasive balloon dilation provides lasting relief for Eustachian tube dysfunction, restoring hearing and quality of life.
Eustachian Tube Dysfunction: A Direct Procedural Approach
Eustachian tube dysfunction (ETD) is a common cause of ear-related symptoms including muffled hearing, aural fullness, pain, and problems with balance. Until recently, invasive surgical solutions or symptomatic therapies such as pressure equalization tube placement were the mainstays of treatment. Today, balloon dilation of the Eustachian tube has emerged as a minimally invasive, effective technique, providing symptomatic relief and improving quality of life for many patients.
This article covers the latest advances in ETD management, highlights clinical outcomes, and explains the procedural details, candidate selection, safety profile, and future directions for this novel approach.
Understanding Eustachian Tube Dysfunction
The Eustachian tube connects the middle ear to the back of the nose, regulating air pressure and draining fluid. Dysfunction occurs when this tube fails to open and close properly, causing symptoms such as:
- Aural fullness (the sensation of ear blockage)
- Muffled or distorted hearing
- Ear pain and recurrent infections
- Difficulty equalizing pressure—especially during altitude changes
- Chronic otitis media (middle ear infections)
Traditional options for persistent or chronic ETD included pressure equalization tubes (PETs) and invasive surgeries. Often, these interventions offered only temporary or incomplete relief, or carried higher risks and inconvenience for patients.
The Rise of Balloon Dilation: A Minimally Invasive Solution
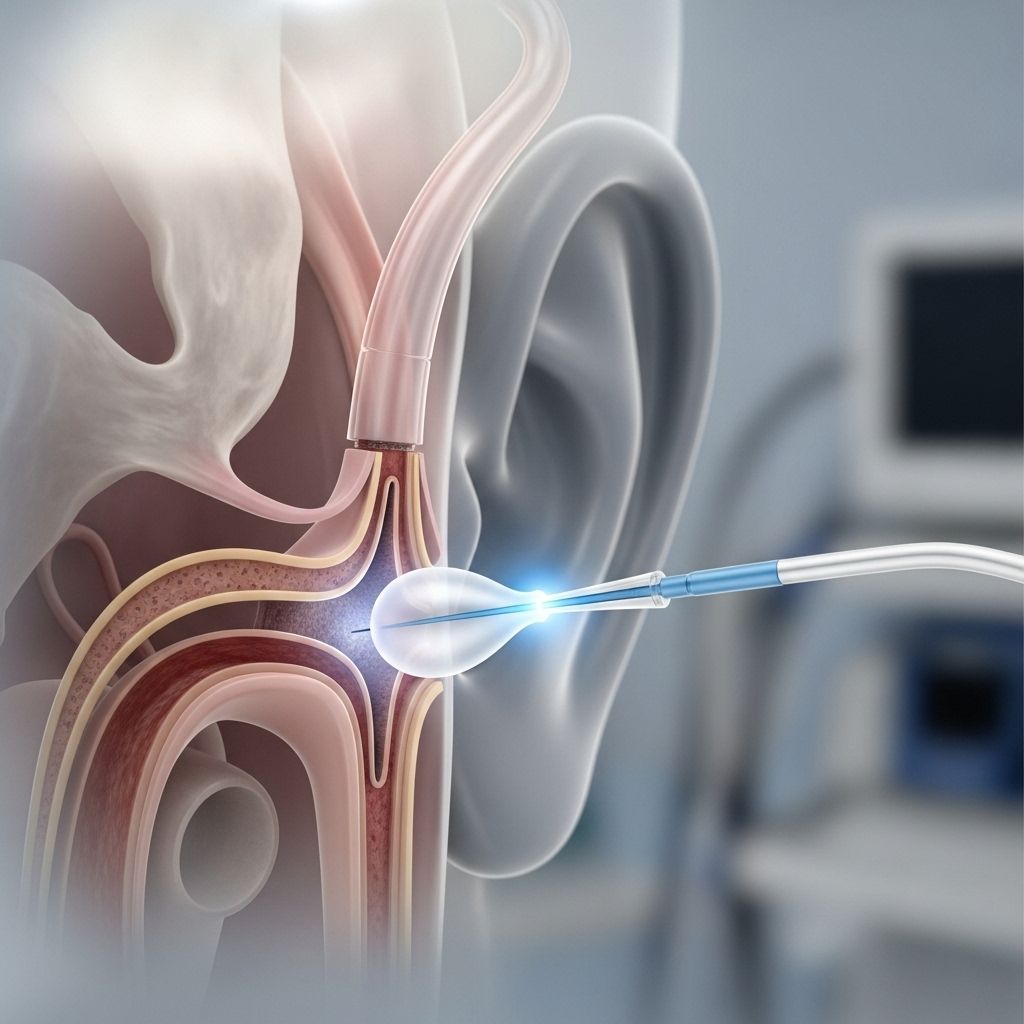
Balloon dilation (also called balloon Eustachian tuboplasty or BET) involves the gentle expansion of the Eustachian tube using an endoscopically guided balloon catheter. The procedure restores tube patency, reduces symptoms, and often improves hearing.
Key procedural milestones in the development and refinement of balloon dilation include:
- Initial trials demonstrating technical feasibility and safety
- Growing clinical data supporting long-term results
- Recognition as a first-line minimally invasive procedure for select ETD patients
Mechanism and Procedure Overview
Balloon dilation is typically performed under general anesthesia by an otolaryngologist. The main steps include:
- Endoscopic visualization of the Eustachian tube opening via the nasal cavity
- Insertion of a balloon catheter into the cartilaginous part of the Eustachian tube
- Inflation of the balloon (usually to 10 bars) for 2 minutes to widen and decompress the tube
- Gentle withdrawal and re-evaluation of tube patency
Mild discomfort, such as sore throat, is possible in the days following the procedure, but serious side effects are rare.
Follow-up occurs after the procedure; patients are often advised to avoid strenuous activities and nose blowing for about a week.
Candidate Selection and Evaluation
Not all ETD cases are suitable for balloon dilation. Key selection criteria include:
- Persistent symptoms despite medical therapy
- Chronic or recurrent otitis media
- Poor middle ear pressure equalization demonstrated by Valsalva or Toynbee maneuvers
- Positive diagnostic findings on examination
- Absence of obstructive anatomical abnormalities or tumors
A full evaluation includes a detailed history, physical examination, and may involve imaging or endoscopy to assess Eustachian tube anatomy and function.
Clinical Outcomes: Efficacy and Durability
Recent studies report long-lasting symptom relief following balloon dilation for ETD. Key findings include:
- High rates of symptom improvement—including resolution of fullness and hearing loss
- Mild side effects, often limited to transient discomfort
- Durable results, with many patients remaining symptom-free for a year or more
| Outcome | Percentage of Patients | Notes |
|---|---|---|
| Significant Symptom Relief | ~85% | Reduction in fullness, hearing loss |
| Mild Side Effects | <10% | Sore throat, minor discomfort |
| Long-term Benefit | 60-70% | Durable improvement at 12 months |
Studies suggest that results from BET are generally superior to repeated pressure tube insertions and reduce the burden of chronic ear disease.
Comparison with Other Procedures
Other interventions for ETD and related conditions include:
- Catheter (shim) insertion—provides a temporary stent effect
- Calcium hydroxyapatite injection—adds bulk to the Eustachian tube walls
- Reconstruction and obliteration procedures—used for patulous Eustachian tube dysfunction (PETD)
While each method may relieve symptoms, balloon dilation stands out for its minimally invasive nature, low risk, and durability for classic ETD (not patulous type).
Safety, Risks, and Side Effects
Research consistently finds BET to be safe, with mild, transient side effects.Potential risks include:
- Sore throat, nasal discomfort (most common)
- Rare risk of bleeding or infection
- Unintended pressure or trauma to tube walls (very rare)
Rigorous surgical training and endoscopic guidance minimize risks. No major complications were reported in large case series, and post-procedure monitoring further ensures safety.
Combining Procedures: Complex and Resistant Cases
Some patients benefit from combining BET with other ear surgeries, such as myringoplasty, especially in cases with underlying chronic infection or poor mastoid aeration. Ongoing research explores whether staged or synchronous interventions provide added value.
Post-Procedural Care and Recovery
Most patients experience a rapid recovery:
- Mild symptoms (sore throat, discomfort) typically resolve within days
- Activity restrictions for 5–7 days after procedure
- Follow-up evaluations assess benefit and need for further interventions
Patients are advised to avoid nose blowing and strenuous activity to reduce risk of pressure changes or tube trauma during healing.
Current Research and Future Directions
While existing studies support balloon dilation as safe and effective, ongoing research includes:
- Randomized controlled trials—to further validate efficacy against placebo or other surgical methods
- Head-to-head comparisons of techniques (BET vs. catheter, injection, reconstruction)
- Exploring BET in special populations—children, patients with complex ear diseases
- Defining long-term durability beyond 1–2 years of follow-up
Future refinements in BET technology, patient selection criteria, and adjunctive therapies may improve outcomes even further.
Patient Stories: Renewed Quality of Life
Patients who undergo balloon dilation often report dramatic improvements:
- Restoration of normal hearing
- Freedom from persistent ear fullness
- Return to normal daily activities and recreation
Many express gratitude for the minimally invasive nature of the procedure and rapid return to comfort.
Frequently Asked Questions (FAQs)
Q: Who is a good candidate for Eustachian tube balloon dilation?
A: Patients with chronic symptoms of ETD—especially aural fullness, poor pressure equalization, and recurrent infections—unresponsive to medical therapy are ideal candidates after thorough evaluation.
Q: What is the recovery like after balloon dilation?
A: Most experience mild discomfort and soreness, with full recovery in several days. Normal activities can resume after a week, and risks are low when postoperative instructions are followed.
Q: Is balloon dilation safe and effective?
A: Yes. Studies confirm a high safety profile, rare side effects, and durable improvement in symptoms and hearing, often lasting a year or longer.
Q: Will my hearing improve after the procedure?
A: Most patients report restoration of hearing and relief from fullness or blockage soon after balloon dilation.
Q: Are additional treatments ever needed?
A: Some patients may require extra procedures for complex cases or if symptoms recur, but most experience long-term relief after a single intervention.
Key Takeaways
- Balloon dilation is transforming ETD management by providing a safe, rapid, and durable relief
- Patient selection is crucial for optimal results
- Clinical studies support both efficacy and safety, and future research may further refine the technique
For those suffering from chronic Eustachian tube dysfunction, direct procedural options like balloon dilation offer hope for restored hearing, comfort, and quality of life.
References
- https://premiersinus.com/services/eustachian-tube-balloon-dilation/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9682686/
- https://pure.johnshopkins.edu/en/publications/twelve-month-outcomes-of-eustachian-tube-procedures-for-managemen
- https://pubmed.ncbi.nlm.nih.gov/30325505/
- https://www.youtube.com/watch?v=CoxHpqZ2NUw
- https://onlinelibrary.wiley.com/doi/full/10.1002/lary.30659
- https://pure.johnshopkins.edu/en/publications/patulous-eustachian-tube-dysfunction-symptoms-following-balloon-d
Read full bio of Sneha Tete












