Understanding Endovascular Aneurysm Repair (EVAR): Procedure, Benefits, and Risks
A comprehensive guide to endovascular aneurysm repair—what it is, how it works, risks, recovery, and frequently asked questions.
What to Know About Endovascular Aneurysm Repair (EVAR)
Endovascular aneurysm repair (EVAR) is a minimally invasive surgical technique that helps treat certain types of aneurysms in the aorta— the large artery carrying blood from your heart to your body. By reinforcing weakened sections of the aorta, EVAR reduces the risk of a life-threatening rupture, offering a safer and faster recovery than open surgery for many patients.
What is Endovascular Aneurysm Repair (EVAR)?
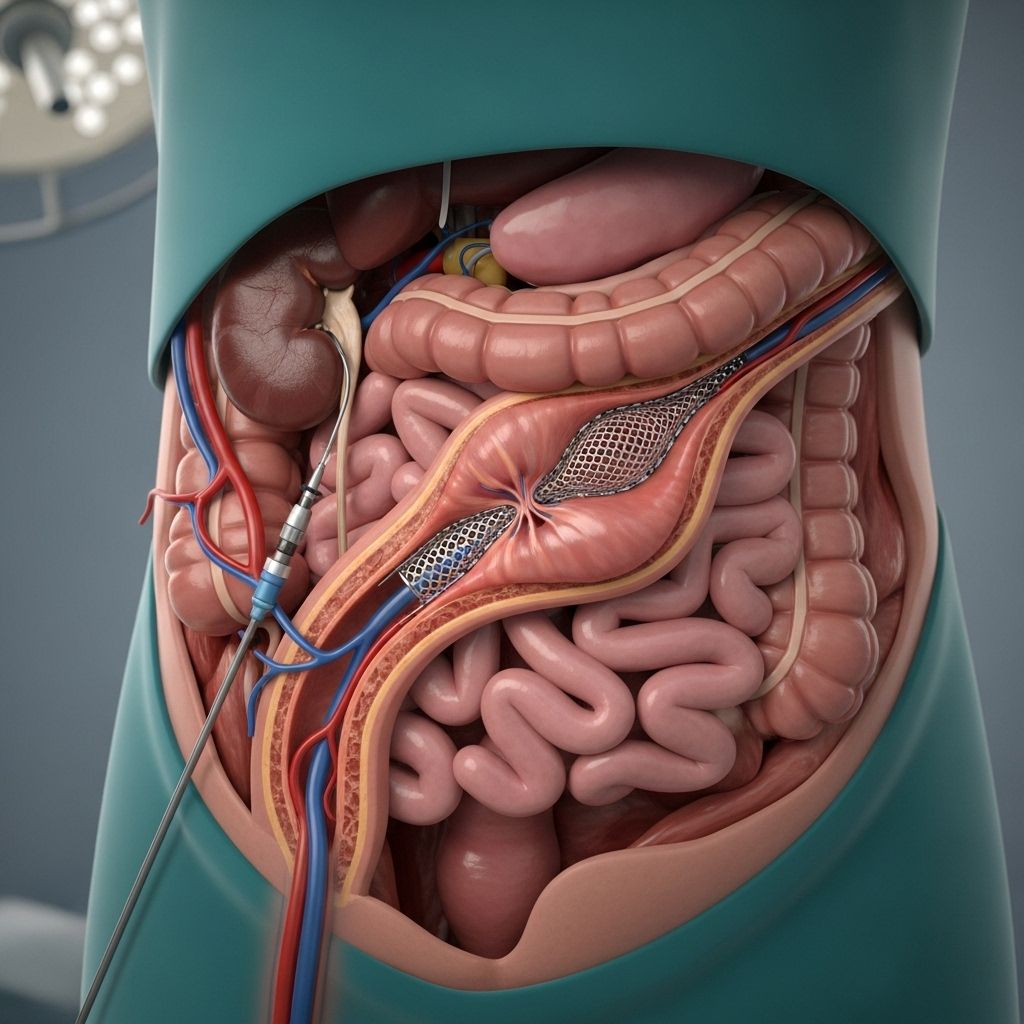
Endovascular aneurysm repair is a modern procedure designed to fix an aortic aneurysm, a dangerous bulging (or ballooning) in the wall of the aorta. Most often, the treatment targets abdominal aortic aneurysms (AAA), which appear in the section of the aorta that runs through your abdomen. The main aim of EVAR is to prevent the aneurysm from rupturing by inserting a stent graft that provides a new pathway for blood flow inside the vessel, keeping blood away from the weakened section.
- Minimally invasive: Performed through small incisions in the groin, not large chest or abdominal incisions.
- Stent graft placement: A stent (a metal mesh tube) with a fabric covering is guided through the blood vessels to the aneurysm’s location, where it is expanded and attached to healthy vessel walls.
- Goal: Reinforce the aneurysm site, lower the chance of rupture, and reduce complications.
Why is EVAR Performed?
EVAR is recommended in cases where an abdominal aortic aneurysm becomes large, grows quickly, or threatens to rupture. Untreated, a ruptured aortic aneurysm can be fatal. The decision for EVAR depends on several factors:
- Aneurysm size: Typically recommended if the aneurysm is larger than 5 centimeters (about 2 inches)
- Growth rate: If it has grown more than 0.5 centimeters (0.2 inches) in 6–12 months
- Symptoms: Such as pain, tenderness, or signs that it may burst
- Risk for rupture: Higher if the aneurysm is large or changing rapidly
- Risk for open surgery: Offers a less invasive option for older adults and those with medical conditions making open surgery riskier
Some aneurysms may be found incidentally, during ultrasounds or CT scans performed for other reasons. Treatment is aimed at preventing a deadly rupture by fortifying the vessel wall from inside using the EVAR technique.
Who is a Good Candidate for EVAR?
Not everyone with an aortic aneurysm will be eligible for EVAR. The suitability of EVAR mainly depends on factors such as:
- Size, shape, and position: The anatomy of the aneurysm and surrounding blood vessels
- Overall health: Especially in patients who are older, or have additional illnesses such as heart, lung, or kidney disease
- Risk factors: Those for whom traditional open surgery would pose higher risks due to age or other medical conditions
Certain aneurysm shapes, such as those involving branches of the aorta or other anatomical complexities, may require different approaches or disqualify a patient from EVAR completely.
How is the EVAR Procedure Performed?
EVAR is typically performed in a hospital’s radiology or operating suite, and the procedure involves the following main steps:
- Anesthesia: Patients usually receive either general anesthesia (put to sleep), or spinal/epidural anesthesia to numb the lower part of the body.
- Incision: Small cuts are made near the groin to access the femoral arteries.
- Catheter Insertion: A thin, flexible tube (catheter) is threaded up through the blood vessels to the aneurysm’s site under X-ray guidance.
- Stent Graft Placement: A stent graft—a fabric-covered metal mesh tube—is guided through the catheter and extended to cover the aneurysm.
- Imaging: Dye is injected and X-rays ensure correct placement of the graft and assess for any leaks.
- Completion: The catheters are removed and the groin incisions are closed with stitches, staples, or special tape.
The graft creates a stable, reinforced channel through which blood can flow, diverting it from the weak spot in the aorta. Over time, the aneurysm tends to shrink as blood is no longer directly pushing against its walls.
Preparing for EVAR
Proper preparation is important for the success of an endovascular aneurysm repair. Before the procedure, patients commonly undergo:
- Imaging studies: CT scans or ultrasounds to visualize the aneurysm and plan the repair accurately
- Medication review: Doctors may ask you to stop certain blood thinners, or adjust medications
- Fasting: You may need to avoid food and drink for several hours before surgery
- General pre-op testing: Blood tests, chest X-rays, ECG (heart tracing), and assessment for anesthesia risk
Always inform your healthcare team of all medications, supplements, and medical conditions before the procedure. Arrange for someone to help you at home after discharge, as you may be unable to drive or stand for long periods immediately after surgery.
What Are the Benefits of EVAR?
EVAR has significant advantages compared to traditional open surgery for aortic aneurysm repair:
- Minimally invasive: No large abdominal or chest incisions, leading to less trauma
- Faster recovery: Most patients go home in just 1–3 days
- Less pain: Smaller incisions mean less post-op discomfort
- Lower early risk: Reduced risk of some complications, especially in people with other health conditions
- Reduced blood loss: Less need for transfusions or intensive care
EVAR’s benefits are often most pronounced in older adults or those who would not be good candidates for open surgery due to other medical risks.
Potential Risks and Complications
While EVAR is generally considered safer and faster to recover from than open surgery, it does come with certain risks and complications:
- Bleeding before, during, or after the procedure (possibly requiring additional intervention)
- Infection (incision, urinary tract, or lungs)
- Blood clots in the legs that could travel to the lungs (pulmonary embolism)
- Heart attack or stroke
- Kidney problems or failure (especially in those with previous kidney disease)
- Blockage of the stent (which may reduce blood flow to the legs or organs)
- Endoleak (continued blood flow into the aneurysm sac, sometimes requiring extra procedures)
- Stent migration (moving from the original position)
- Nerve injuries causing leg pain, numbness, or weakness
- Problems with sexual function in men (erectile dysfunction)
- Death is rare, but possible
Some complications, such as endoleaks or stent migration, are specific to endovascular procedures and may necessitate follow-up procedures or, rarely, conversion to open surgery. Frequent monitoring and imaging after EVAR are important to detect these issues early.
EVAR vs. Open Surgical Repair: Key Differences
| Feature | EVAR | Open Surgery |
|---|---|---|
| Approach | Through blood vessels (minimally invasive) | Large abdominal/chest incision |
| Hospital Stay | Usually 1-3 days | Usually 5-10 days |
| Recovery Time | 2-6 weeks | Up to 3 months |
| Blood Loss | Minimal | Greater |
| Follow-up Needs | Ongoing imaging for leaks/stent position | Less frequent imaging after initial recovery |
| Who’s Eligible? | Depends on artery anatomy, better for high-risk patients | Works for most, but higher risk for frail or elderly |
Recovery After EVAR
Most people recover from EVAR much faster compared to open surgery. Here’s what to expect:
- Hospital stay: Usually 1–3 days post-procedure
- Post-operative monitoring: Vital signs and graft success are monitored closely
- Activity: Gradual return to normal activity; avoid heavy lifting for several weeks
- Pain management: Pain at incision sites is usually mild and managed with oral pain relievers
- Follow-up imaging: Necessary at regular intervals to check for graft leaks or stent movement
Most patients feel ready to resume many day-to-day activities within two weeks, though complete healing and return to strenuous activity may take a bit longer.
Self-Care and Tips After EVAR
- Take all medications as prescribed, including any antibiotics or blood pressure medicines
- Follow activity restrictions—ask your healthcare provider about when you can drive, bathe, or return to work
- Watch for signs of complications such as severe pain, fever, swelling, numbness, or bleeding from incision sites—seek medical help if these occur
- Attend all scheduled follow-up appointments for imaging tests and check-ups
- Adopt heart-healthy lifestyle habits: quit smoking, eat a balanced diet, exercise regularly, and keep blood pressure under control
Long-Term Outlook and Monitoring
With successful EVAR, people can expect a good quality of life, especially when risk factors for vascular disease are managed. However, routine follow-up imaging (CT or ultrasound) is required at regular intervals for life. This is crucial to monitor for stent movement, endoleaks (blood leaking back around the graft), or other delayed complications requiring further care.
Some patients may eventually require additional interventions if late complications appear. Your medical team will tailor your follow-up schedule based on your health status and procedure results.
FAQs: Frequently Asked Questions About EVAR
Is EVAR a cure for all aortic aneurysms?
No. EVAR is best for certain types of aortic aneurysms, particularly those located in the abdomen with favorable anatomy. Some aneurysms in other locations or with complex shapes may not be suitable for this approach.
How long does the stent graft last?
Stent grafts are designed for long-term durability, often lasting many years. However, ongoing imaging is necessary to ensure they stay in place and there are no leaks or complications over time.
Is open surgery ever preferred?
Yes. If the aneurysm or arteries are unsuitable for EVAR, or if there is failure of the endovascular graft, traditional open surgery may be recommended. Your surgical team will decide the safest approach based on your specific condition.
What are signs of a complication after EVAR?
Symptoms such as chest, back, or abdominal pain; persistent fever; swelling, redness, or drainage from incision sites; numbness or weakness in the legs; or abdominal pulsations may suggest complications. Seek immediate medical attention if these occur.
Can you prevent aneurysms from developing?
While not all aneurysms can be prevented, you can reduce risk by managing blood pressure, avoiding tobacco, staying physically active, and treating chronic conditions like high cholesterol and diabetes.
Are routine check-ups necessary?
Yes. Lifelong monitoring with periodic scans is crucial after EVAR, as some complications like endoleaks or graft movement may not cause symptoms but need early detection and treatment.
Summary
Endovascular aneurysm repair (EVAR) offers a minimally invasive, effective treatment option for certain aortic aneurysms, particularly abdominal aortic aneurysms. With faster recovery and fewer early complications compared to open repair, EVAR is especially valuable for older adults or those with additional medical risks. Careful selection, experienced providers, and ongoing lifelong monitoring are essential for long-term success and prevention of serious complications. Always discuss the risks, benefits, and alternatives with your medical team to determine the best approach for your situation.
References
- https://www.icrjournal.com/articles/endovascular-aneurysm-repair?language_content_entity=en
- https://medlineplus.gov/ency/article/007391.htm
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3387737/
- https://www.healthline.com/health/heart/endovascular-aneurysm-repair
- https://www.healthline.com/health/endovascular-reconstruction
- https://www.mayoclinic.org/medical-professionals/cardiovascular-diseases/news/endovascular-repair-of-complex-aortic-aneurysms/mac-20429867
Read full bio of medha deb












