Endoscopic Retrograde Cholangiopancreatography (ERCP): Procedure, Preparation, Risks, and FAQs
A comprehensive guide to understanding ERCP, from preparation and procedure to risks, recovery, and frequently asked questions.
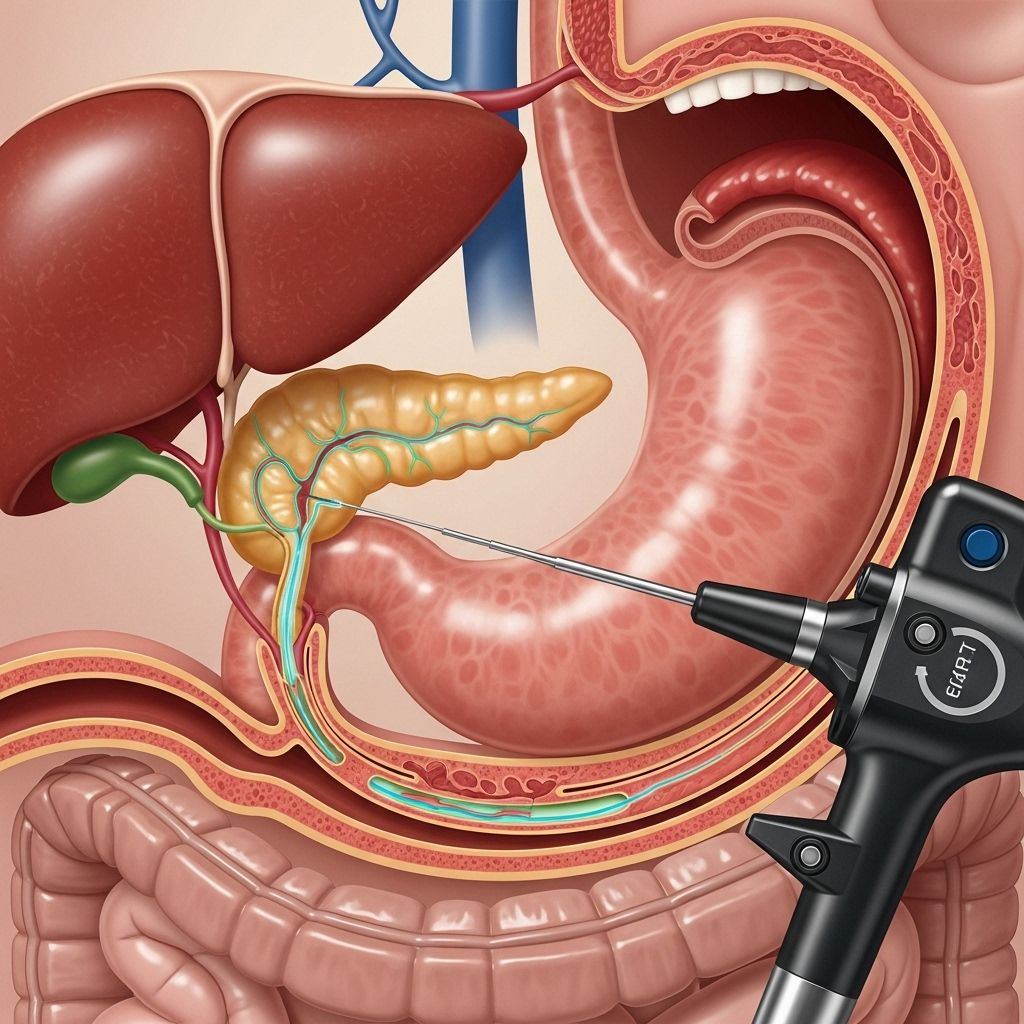
Endoscopic retrograde cholangiopancreatography (ERCP) is a specialized procedure that enables doctors to diagnose and treat conditions of the bile ducts, pancreatic duct, and gallbladder. By combining endoscopy and X-ray imaging, ERCP offers both diagnostic insights and therapeutic interventions for various disorders affecting the digestive system.
What is ERCP?
ERCP is an advanced medical technique that uses an endoscope—a thin, flexible tube with a camera—to access the digestive tract and inject contrast dye into the bile and pancreatic ducts. This allows physicians to visualize these passageways on X-ray images and perform treatments such as removing bile duct stones, relieving obstructions, or obtaining tissue samples for biopsy.
Why Might I Need ERCP?
ERCP is recommended for patients who show signs or symptoms of disorders affecting their bile ducts, pancreas, or gallbladder. Common indications for this procedure include:
- Diagnosis or treatment of blockages or narrowing in the bile or pancreatic ducts
- Removal of gallstones or bile duct stones
- Evaluation of chronic pancreatitis or unexplained upper abdominal pain
- Assessment of abnormal liver tests or jaundice
- Investigation of suspected tumors or cancers of the bile ducts or pancreas
- Treatment for strictures, leaks, or injuries in the ducts
- Placement or replacement of stents to keep ducts open or relieve blockages
How Should I Prepare for ERCP?
Preparation for ERCP is essential to ensure your safety and the success of the procedure. Your healthcare team will provide specific instructions tailored to your situation. Key preparation steps include:
- Fasting: Do not eat or drink for at least 6 to 8 hours before ERCP to reduce the risk of aspiration.
- Medication Review: Inform your doctor about all medications you take, including blood thinners, diabetes medications, and immunosuppressants. You may need to stop certain medications before the procedure.
- Allergy Disclosure: Tell your team if you are allergic to iodine, shellfish, or contrast dye.
- Arrange Transportation: You will receive sedatives during ERCP, so arrange for someone to drive you home afterward.
- Consent: Your provider will review and have you sign a consent form, ensuring you understand the risks, benefits, and alternatives.
You may also be asked to change into a hospital gown and remove any jewelry or dentures prior to the procedure.
What Happens During the ERCP Procedure?
ERCP is usually performed by a trained gastroenterologist or surgical specialist and typically takes one to two hours.
- Sedation: An intravenous (IV) line is placed for sedatives or anesthesia to ensure your comfort and minimize memory of the procedure.
- Throat Preparation: You may be given a local anesthetic spray or liquid to numb the back of your throat, reducing the gag reflex.
- Endoscope Insertion: You will lie on your left side, and the doctor will gently insert the endoscope through your mouth, down the esophagus, into the stomach, and into the first part of the small intestine (the duodenum).
- Cannulation: A thin tube (catheter) is passed through the endoscope to reach the openings of the bile and pancreatic ducts.
- Contrast Dye Injection: A special dye is injected through the catheter, making the ducts visible on X-ray (fluoroscopy) images.
- Imaging and Intervention: The doctor examines the images for blockages, stones, strictures, or other abnormalities, and treats them if needed by removing stones, widening narrowed areas, placing stents, or taking biopsies.
What Are the Benefits of ERCP?
ERCP is both a diagnostic and therapeutic tool with several advantages:
- Non-surgical Correction: Many duct problems can be treated without open surgery, reducing hospital stays and recovery times.
- Real-time Diagnosis: The procedure allows for immediate visualization and treatment of obstructions, stones, or strictures.
- Direct Treatment: Therapeutic interventions—such as stone removal, stent placement, or dilation—can be performed during the same session as diagnosis.
- Investigation of Unexplained Symptoms: ERCP can clarify the cause of persistent abdominal pain, jaundice, or abnormal liver tests.
Potential Risks and Complications of ERCP
Although ERCP is considered safe when performed by experienced professionals, it does carry a risk of complications, including:
| Risk | Description | Frequency |
|---|---|---|
| Pancreatitis | Inflammation of the pancreas. Symptoms include abdominal pain, nausea, vomiting, and possibly fever. | 5–8% (up to 20% in certain individuals) |
| Bleeding | Particularly if a sphincterotomy or tissue biopsy is performed. | Rare; risk increases with certain procedures |
| Infection | Infection of the bile ducts or pancreas can occur, especially if there is a blockage. | Uncommon with proper antibiotic use |
| Perforation | A tear or hole in the esophagus, stomach, or intestine requiring surgical repair. | Very rare |
| Adverse reaction to sedation | Allergic reactions, breathing difficulties, or cardiovascular issues related to sedative medications. | Possible, but closely monitored |
| Missed diagnosis | As with any procedure, there is a small chance that abnormalities may not be detected. | Rare |
Most complications are mild and can be managed with hospitalization and supportive care. Notify your healthcare provider immediately if you develop fever, worsening abdominal pain, severe nausea, vomiting, or signs of bleeding after ERCP.
What Happens After the Procedure?
Recovery after ERCP varies based on the procedures performed and whether any complications arise. Key points about post-procedure care include:
- Observation: Most patients are monitored in a recovery area until the sedative wears off—typically one to two hours after the procedure.
- Mild Discomfort: Sore throat, stomach discomfort, or bloating may occur. These symptoms usually resolve within 24 hours.
- Resuming Diet: Eating and drinking can usually resume once swallowing is comfortable, unless told otherwise by your provider.
- Activity: Avoid driving, operating machinery, or making important decisions for the rest of the day due to lingering effects of sedation.
- Hospital Stay: Most patients return home the same day, but some may require overnight observation—especially if a stent was placed, a stone was removed, or if mild pancreatitis develops.
Your doctor will provide specific instructions regarding medications, signs of complications to watch for, and follow-up appointments as needed.
Alternatives to ERCP
Certain imaging tests and procedures may be considered as alternatives to ERCP, especially when only diagnosis (not treatment) is required. These include:
- Magnetic Resonance Cholangiopancreatography (MRCP): A non-invasive MRI test to visualize the bile and pancreatic ducts without endoscopy or X-rays.
- Endoscopic Ultrasound (EUS): Uses ultrasound via endoscopy to image the digestive tract and surrounding organs.
- Percutaneous Transhepatic Cholangiography (PTC): Involves needle access to the bile ducts through the skin, often when ERCP is not possible.
Your provider will help determine the best approach for your needs.
Frequently Asked Questions (FAQs) About ERCP
Q: Will I be asleep during ERCP?
Most patients receive sedation that makes them relaxed and sleepy. Some may receive general anesthesia, depending on their medical condition and the complexity of the procedure.
Q: How long does ERCP take?
The procedure itself usually takes one to two hours. Additional preparation and recovery time should be expected.
Q: Can I eat or drink after ERCP?
Typically, you can resume eating and drinking once the sedative wears off and your swallowing reflex has returned. Follow your provider’s specific instructions.
Q: What should I do if I develop severe symptoms after ERCP?
Contact your healthcare provider immediately if you experience fever, severe abdominal pain, persistent vomiting, chest pain, or signs of bleeding.
Q: How soon can I return to normal activities?
Most people can return to regular activities, including work, the day after ERCP. However, avoid strenuous activity and driving for at least 24 hours post-procedure.
Q: Is ERCP covered by insurance?
ERCP is typically covered by health insurance, but coverage can vary depending on your provider. Check with your insurance company before the procedure.
Key Takeaways
- ERCP is a vital procedure for diagnosing and treating conditions of the bile ducts, pancreas, and gallbladder.
- It offers both diagnostic and therapeutic benefits, reducing the need for more invasive surgery in many cases.
- Risks include pancreatitis, bleeding, infection, and reactions to sedatives, but these are generally uncommon and manageable with prompt care.
- Careful preparation and following your doctor’s instructions are essential for safety and success.
Frequently Asked Questions (FAQs) — Short Answers
Will I be under general anesthesia for ERCP?
Most patients receive moderate sedation or deep sedation; general anesthesia may be used for select cases.
What symptoms should I report after ERCP?
Contact your doctor promptly if you develop fever, chills, worsening abdominal pain, persistent nausea or vomiting, or rectal bleeding.
Who should not undergo ERCP?
People with certain severe health conditions, known allergies to contrast dye, or uncorrected blood-clotting disorders may not be suitable candidates. Always discuss your health history with your doctor before scheduling the procedure.
How effective is ERCP?
ERCP provides both diagnostic and therapeutic benefits, successfully treating a variety of ductal conditions in a minimally invasive manner, reducing the need for open surgery.
References
- https://gastroassociatesla.com/endoscopic-retrograde-cholangiopancreatography-ercp-baton-rouge-la/
- https://indygastro.com/endoscopic-retrograde-cholangiopancreatography-ercp/
- https://www.healthline.com/health/ercp-procedure
- https://gipartnersofil.com/treatment/endoscopic-retrograde-cholangiopancreatographyercp/
- https://www.medparkhospital.com/en-US/disease-and-treatment/ercp-endoscopic-retrograde-cholangiopancreatography
- https://www.medstarhealth.org/blog/ercp-understanding-risks-rewards
- https://www.niddk.nih.gov/health-information/diagnostic-tests/endoscopic-retrograde-cholangiopancreatography
- https://my.clevelandclinic.org/health/diagnostics/4951-ercp-endoscopic-retrograde-cholangiopancreatography
- https://www.guysandstthomas.nhs.uk/health-information/ercp-endoscopic-retrograde-cholangio-pancreatography
Read full bio of Sneha Tete












