Endocarditis and Cough: Understanding Symptoms, Risks, and Treatments
Learn why endocarditis can cause cough, its symptoms, risk factors, and effective treatments for heart health.
Does Endocarditis Make You Cough?
Endocarditis is a rare infection of the heart’s inner lining (endocardium), impacting approximately 3–10 people per 100,000. One of its complications is coughing, which may arise as an early nonspecific symptom, or as a sign of severity if the infection damages heart structures, leads to heart failure, or affects the lungs.
- Coughing in endocarditis can indicate underlying heart or lung involvement.
- This symptom may be due to fluid buildup (from heart failure) or direct lung infection/pneumonia related to bacterial spread.
- The cough may be dry or productive and is usually accompanied by other flu-like signs.
Effectively treating the underlying infection and any heart damage can usually resolve an endocarditis-related cough.
How Does Endocarditis Cause a Cough?
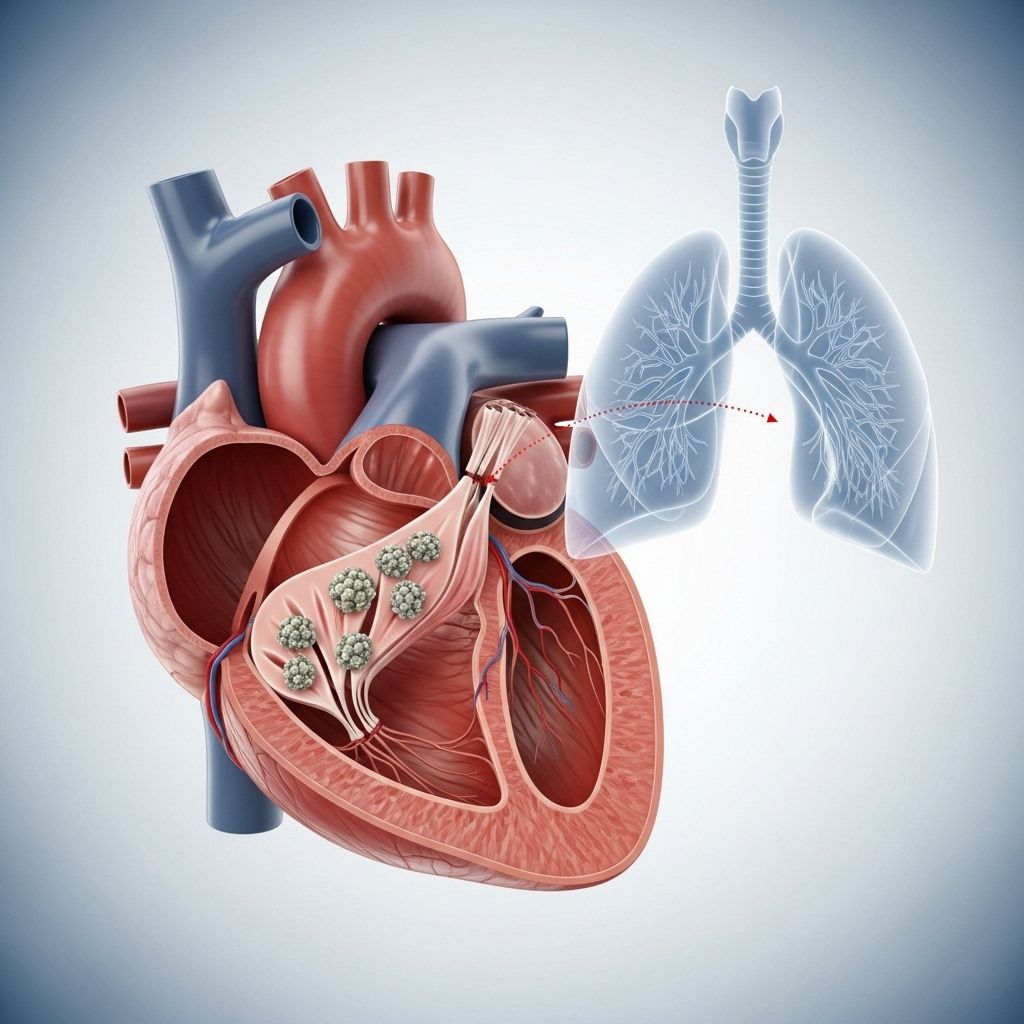
The mechanism behind coughing in endocarditis involves several factors:
- Fluid Retention: When the heart isn’t pumping efficiently, fluid can build up in the lungs (pulmonary edema), triggering a cough.
- Bacterial Spread: Clumps of bacteria can travel like tiny clots to the lungs, blocking blood flow or causing infection/pneumonia. This leads to cough, sometimes with sputum.
- Medications: Certain heart failure medications (like ACE inhibitors) can cause a dry cough as a side effect.
Untreated endocarditis can escalate to more severe conditions (e.g., heart failure) that make coughing more pronounced.
What is Endocarditis?
Endocarditis is a potentially fatal infection of the inner lining of the heart. It primarily occurs when bacteria or, less commonly, fungi or viruses enter the bloodstream and settle on the heart valves or endocardium.
- Most cases are bacterial (infective endocarditis).
- Fungal or viral cases are rarer but may require surgical intervention.
- Recent research has identified post-viral endocarditis as a complication of COVID-19.
How Does It Start?
Bacteria may enter the bloodstream via:
- Cuts, wounds, or injection sites
- Dental procedures
- Surgeries on organs like the heart, GI tract, or urinary tract
Once inside, bacteria attach to heart valves or lining, proliferate, and damage tissues, which can compromise heart function.
Other Symptoms of Endocarditis
While cough is one possible symptom, several others may be more prominent or classic in endocarditis. These can range from subtle early signs to acute complications if not diagnosed and treated promptly.
- Fever
- Chills
- Night sweats
- Headaches
- Joint and muscle pain
- Fatigue
- Shortness of breath
- New or changing heart murmur
- Weight loss and poor appetite
- Petechiae: Small red, brown, or purple spots on the skin
- Painless red spots: Seen on palms and soles
- Painful red spots: On fingertips and toes
- Bleeding under the nails
In addition, advanced and poorly managed cases can lead to:
- Sepsis: Life-threatening body-wide infection
- Stroke: Due to emboli (clumps of bacteria) traveling to the brain
- Heart valve damage
- Heart failure
Risk Factors for Endocarditis
Anyone can develop endocarditis, but those with preexisting heart conditions or certain risk factors are far more likely to be affected.
- Artificial heart valves
- Congenital heart defects
- History of rheumatic fever
- Mitral valve prolapse
- Hypertrophic cardiomyopathy
- Implanted medical devices (pacemakers, defibrillators)
- An immunocompromised state (such as HIV or chemotherapy)
- Intravenous (IV) drug use
- Recent surgical or dental procedures
- Age over 60 years
Table: Common Risk Factors for Endocarditis
| Risk Factor | Notes |
|---|---|
| Artificial Heart Valve | Bacterial colonization risk is high after implant. |
| Prior Endocarditis | History increases recurrence risk. |
| Congenital Heart Defect | Structural changes promote bacterial attachment. |
| IV Drug Use | Needle use introduces bacteria directly. |
| Dental/Surgical Procedures | Bacteria may enter bloodstream. |
| Immunocompromised | Reduced resistance increases risk. |
How Do You Treat an Endocarditis Cough?
The cornerstone of treating endocarditis—and therefore the associated cough—is medical management in a hospital setting.
- IV Antibiotics: Carefully selected based on the causative organism. Blood cultures determine the best antibiotics.
- Duration: Typically 6–8 weeks of intensive therapy, often starting in-hospital.
- Infectious Disease Consultation: Specialists tailor therapy and monitor progress.
Most symptoms, including cough, subside as infection is controlled and inflammation resolves.
When is Surgery Needed?
- Valve Repair or Replacement: Required if heart valves are severely damaged.
- Medical Device Replacement: Pacemakers, defibrillators may need replacing if infected.
- Abscess Drainage and Fistula Repair: Needed to restore heart function and relieve symptoms like cough.
- Fungal Endocarditis: Surgery is more likely if caused by fungi.
Treatment outcomes are best when started early—delayed therapy can result in severe, multi-organ complications.
Managing the Cough Itself
- Cough improves with infection management. Symptomatic treatment (like cough suppressants) may be considered if severe, but root cause therapy is paramount.
- Fluid Management: For cough due to fluid buildup (pulmonary edema), diuretics and cardiac support are used.
- Address drug side effects (e.g., switch ACE inhibitors if persistent dry cough).
Complications of Untreated Endocarditis
If endocarditis is left untreated, the risk of life-threatening complications increases substantially.
- Heart Failure: Most common serious complication, often producing cough and breathlessness.
- Valve Destruction: Leads to regurgitation, severe cardiac dysfunction, embolism risk.
- Embolic Events: Clumps of bacteria may block blood vessels (e.g., lungs, brain, spleen), leading to stroke, pulmonary embolism, or abscess formation.
- Sepsis: Bacteria in bloodstream provoking widespread inflammation and organ shutdown.
- Pneumonia: Direct extension to lungs, resulting in cough and respiratory distress.
Urgent diagnosis and initiation of therapy is crucial to prevent these outcomes.
Prevention Strategies
- Maintain good dental hygiene and promptly treat oral infections.
- Practice sterile technique with IV drug use or devices.
- Prophylactic antibiotics prior to invasive dental or surgical procedures if at risk.
- Monitor and manage chronic heart conditions carefully.
- See a doctor promptly if symptoms (especially in high-risk individuals) occur.
Frequently Asked Questions (FAQs)
Q: Is cough always present in endocarditis?
A: No, cough is not always present, but it can occur, especially if the infection progresses or affects the lungs or causes heart failure.
Q: How can doctors tell if my cough is related to endocarditis?
A: Healthcare professionals assess for additional symptoms (such as fever, heart murmur, fatigue) and risk factors, then order blood cultures, echocardiogram, and possibly chest imaging to make the diagnosis.
Q: Can you recover fully from endocarditis-induced cough?
A: Yes, most people see improvement as the infection is treated and the inflammation subsides. Sometimes, recovery may require heart valve repair or replacement.
Q: Are there lasting effects after treatment?
A: If treated early, many people recover fully. Untreated or delayed cases may result in permanent valve damage, heart failure, or other organ complications.
Q: Who is most at risk for developing endocarditis?
A: Individuals with artificial heart valves, prior endocarditis, certain congenital heart defects, immunocompromised states, or recent invasive procedures are at greatest risk.
When to Seek Medical Help
- High-risk individuals should seek care immediately if experiencing fever, cough, unexplained fatigue, breathlessness, or strange rashes.
- Early diagnosis dramatically improves the outlook.
- Untreated endocarditis can be fatal.
Takeaway
Coughing can be a sign of endocarditis, particularly when accompanied by other symptoms suggesting heart or lung impairment. Understanding the link between the infection, heart function, and lung complications helps guide effective therapy. Early intervention—including IV antibiotics, sometimes heart surgery, and monitoring for complications—is critical for a favorable outcome.
References
- https://www.healthline.com/health/heart-health/endocarditis-cough
- https://uvahealth.com/services/heart-valve-disease/endocarditis
- https://www.tgh.org/institutes-and-services/conditions/endocarditis
- https://my.clevelandclinic.org/health/diseases/16957-endocarditis
- https://www.mayoclinic.org/diseases-conditions/endocarditis/symptoms-causes/syc-20352576
- https://www.pennmedicine.org/conditions/endocarditis
- https://www.nhs.uk/conditions/endocarditis/symptoms/
- https://www.bhf.org.uk/informationsupport/conditions/endocarditis
- https://www.merckmanuals.com/home/heart-and-blood-vessel-disorders/endocarditis/noninfective-endocarditis
Read full bio of Sneha Tete












