End-Stage Heart Failure: Symptoms, Treatments, and Coping Strategies
Understand the complexities of end-stage heart failure, its symptoms, management options, and supportive care for patients and caregivers.
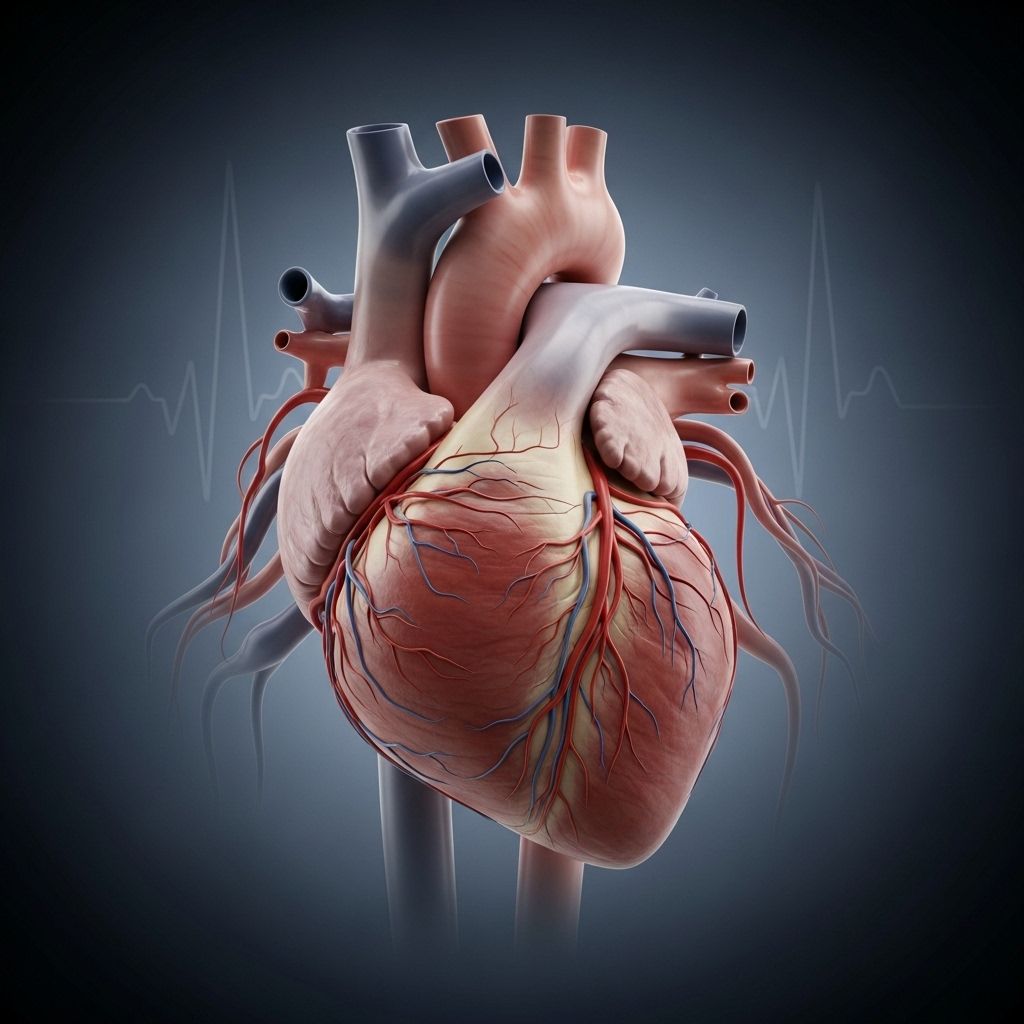
End-stage heart failure, also known as advanced or late-stage heart failure, is the most severe phase of chronic heart failure. In this stage, the heart’s ability to pump blood diminishes so significantly that symptoms persist despite optimal medical therapy. Understanding the symptoms, underlying causes, management options, and coping strategies is critical for patients, caregivers, and healthcare providers.
What Is End-Stage Heart Failure?
Heart failure is a progressive condition in which the heart gradually loses its ability to pump enough blood to support the body’s needs. In end-stage heart failure (sometimes called stage D heart failure, per the American Heart Association’s classification), symptoms become severe and unmanageable with standard treatments. At this point, the focus typically shifts from cure to symptom management, comfort, and quality of life.
Key Characteristics of End-Stage Heart Failure
- Severe and persistent symptoms, even at rest
- Recurrent hospitalizations or inability to leave the hospital
- Limited functional ability, affecting activities of daily living
- Dependence on advanced therapies for relief
Symptoms of End-Stage Heart Failure
Symptoms become more intensive and wide-ranging as heart failure advances. Common symptoms include:
- Shortness of breath (dyspnea), including at rest or when lying down
- Severe fatigue and weakness impacting daily activities
- Swelling (edema) in the legs, ankles, and abdomen
- Persistent cough or wheezing, sometimes producing white or pink blood-tinged phlegm
- Rapid or irregular heartbeat
- Abdominal pain, nausea, or loss of appetite
- Confusion or impaired thinking due to reduced blood flow to the brain
- Changes in skin color (bluish or pale appearance)
- Unintended weight loss
(known as cardiac cachexia, indicating advanced disease)
Causes and Risk Factors
End-stage heart failure is typically the culmination of a longstanding heart condition. Key causes include:
- Coronary artery disease (blocked arteries)
- High blood pressure (hypertension)
- Previous heart attacks
- Certain congenital heart defects
- Heart valve disease
- Cardiomyopathy (disease of the heart muscle)
- Other chronic conditions (such as diabetes or untreated arrhythmias)
Risk Factors
- Age (higher risk with advancing age)
- Male gender
- Obesity
- Persistent unhealthy lifestyle (smoking, poor diet, physical inactivity)
- Family history of heart disease
Diagnosis: Identifying End-Stage Heart Failure
Diagnosing end-stage heart failure requires a comprehensive assessment. This usually includes:
- Physical examination and history of worsening symptoms
- Review of hospitalizations or emergency room visits for heart failure
- Advanced imaging (e.g., echocardiography, cardiac MRI) for ejection fraction, chamber size, and valve function
- Blood tests for markers such as B-type natriuretic peptide (BNP)
- Electrocardiogram (ECG) and chest X-ray
Progression: How Does Heart Failure Reach the End Stage?
Heart failure is progressive – symptoms worsen over time unless the underlying cause is reversed. Although medications and lifestyle changes can slow disease progression, eventually the heart becomes too weak or stiff to maintain adequate circulation. At this point, symptoms never fully resolve, even with optimal medical therapy.
Stages of Heart Failure (AHA Classification)
| Stage | Description |
|---|---|
| A | At risk, but no structural disease or symptoms |
| B | Structural damage, but no symptoms |
| C | Structural disease with prior or current symptoms |
| D | Advanced disease with symptoms at rest, refractive to treatment (End-stage) |
Treatment Options for End-Stage Heart Failure
Once heart failure has reached the end stage, the primary goals of treatment are to:
- Relieve symptoms
- Improve quality of life
- Reduce hospitalizations
- Support patients and families in care planning
Medical Therapy
Medications remain central to management, although they may provide less symptomatic relief in advanced cases.
- ACE inhibitors: Lower blood pressure, reduce strain on the heart
- Angiotensin receptor blockers (ARBs): Similar benefits for those intolerant to ACE inhibitors
- Beta-blockers: Slow the heart, reduce workload, help prevent arrhythmias
- Aldosterone antagonists: Help reduce fluid retention and improve outcomes
- Diuretics: Help remove excess fluid, reducing swelling and breathlessness
- Digitalis (low dose): Used selectively to strengthen the heart’s contractions
- Inotropic therapy: IV medications for temporary or ongoing symptom relief in select patients
Device and Surgical Therapies
- Cardiac resynchronization therapy (CRT): Biventricular pacemakers correct abnormal heart rhythms and chamber synchronization
- Implantable cardioverter-defibrillator (ICD): Prevents life-threatening arrhythmias in some patients
- Left ventricular assist devices (LVADs): Mechanical pumps that help the failing heart deliver blood to the body
- Heart transplantation: For eligible patients, a new heart can resolve heart failure, but this option is limited by age, comorbidities, and donor availability
Palliative and Supportive Care
Palliative care focuses on maximizing comfort and quality of life at every stage of advanced heart failure—not just end of life. Support may include:
- Expert symptom management (pain, breathlessness, anxiety, depression, etc.)
- Assistance with complex decision-making and future planning
- Coordinated care between cardiologists, primary care, nurses, and social workers
- Hospice care for those who choose to focus only on comfort in their remaining time
Other Supportive Approaches
- Supplemental oxygen therapy
- Opioids for severe breathlessness
- Antidepressants and anxiolytics for emotional symptoms
- Nutrition support for severe weight loss (cachexia)
Living With End-Stage Heart Failure: Quality of Life and Emotional Support
Coping with end-stage heart failure can be emotionally and physically draining for both patients and their loved ones. Common needs include:
- Practical guidance on managing day-to-day symptoms (e.g., fluid restriction, monitoring weight, recognizing symptom worsening)
- Clear communication from healthcare providers about prognosis, options, and realistic goals
- Emotional and psychological support for depression, anxiety, and uncertainty
- Advance care planning, including preferences for medical interventions and resuscitation
- Family and caregiver education about what to expect as the disease progresses
How Can You Delay Progression to End-Stage Heart Failure?
For individuals earlier in the disease process, adopting heart-healthy habits and managing risk factors can slow progression:
- Follow a balanced, low-sodium diet
- Take all prescribed medications as directed
- Engage in appropriate physical activity (such as walking or light cardio)
- Stop smoking and limit alcohol intake
- Monitor daily weight and symptoms
- Keep regular follow-up appointments with a care team
Prognosis: What Is the Life Expectancy With End-Stage Heart Failure?
Life expectancy in end-stage heart failure is highly variable and depends on age, underlying health, kidney function, response to treatments, and whether advanced interventions (such as LVAD or transplant) are suitable.
- Without advanced therapies, the estimated median survival is often less than 12 months once symptoms are refractory to standard treatments
- With heart transplant or continuous LVAD support, some patients can survive several years or longer
- Quality of life is a key consideration—many patients and families value comfort, dignity, and time at home over aggressive interventions
Tips for Caregivers
Caring for someone with end-stage heart failure can be overwhelming. Recommendations include:
- Learn about the stages and symptoms of heart failure progression
- Communicate frequently with the healthcare team
- Create a safe, supportive environment for the patient
- Seek respite and accept help from friends or professional caregivers to avoid burnout
- Consider advanced directives and care preferences early
Frequently Asked Questions (FAQs)
Q: How do you know if heart failure is advanced or end-stage?
A: Symptoms are severe and persistent, occur even at rest, and do not significantly improve with conventional therapy. Repeated hospitalizations and functional limitation in daily activities are typical signs.
Q: Can end-stage heart failure be cured?
A: There is currently no cure except potentially for those who receive a successful heart transplant. Most treatments aim to alleviate symptoms and improve quality of life.
Q: What are the main causes leading to advanced heart failure?
A: Common causes include long-standing hypertension, coronary artery disease, repeated heart attacks, and damage to the heart muscle from other illnesses or genetic conditions.
Q: What support is available for families and patients?
A: Palliative care, hospice services, counseling, support groups, and coordinated care with multidisciplinary teams help support both physical and emotional needs.
Q: How do you recognize when the end of life is near?
A: Signs may include rapid worsening of symptoms, increased fatigue, loss of appetite, decreased responsiveness, and recurrent hospitalizations despite maximal treatment—all suggesting the need for transition to comfort-focused care.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC1955535/
- https://www.tgh.org/institutes-and-services/conditions/advanced-heart-failure
- https://www.medicalnewstoday.com/articles/end-stage-heart-failure
- https://www.massgeneralbrigham.org/en/patient-care/services-and-specialties/heart/conditions/end-stage-heart-failure
- https://my.clevelandclinic.org/health/diseases/17069-heart-failure-understanding-heart-failure
- https://www.mariecurie.org.uk/professionals/palliative-care-knowledge-zone/heart-failure
- https://www.webmd.com/heart-disease/heart-failure/end-stage-heart-failure-signs
- https://www.mayoclinic.org/diseases-conditions/heart-failure/symptoms-causes/syc-20373142
- https://resources.amedisys.com/stages-dying-end-stage-congestive-heart-failure
- https://www.nhs.uk/conditions/heart-failure/treatment/
Read full bio of Sneha Tete












