Electromyography (EMG): A Comprehensive Guide to Muscle and Nerve Evaluation
Discover how EMG testing uncovers muscle and nerve health, helping diagnose conditions that affect bodily movement and strength.
Electromyography (EMG): Understanding the Diagnostic Test for Muscles and Nerves
Electromyography (EMG) is an essential diagnostic procedure that assesses the health of muscles and the nerve cells that control them, known as motor neurons. By measuring electrical activity in muscles and nerves, EMG assists medical professionals in diagnosing a range of muscular and neurological conditions. This guide explores the core aspects of EMG testing, including its purpose, indications, procedure steps, preparation, risks, potential outcomes, and commonly asked questions.
What Is Electromyography (EMG)?
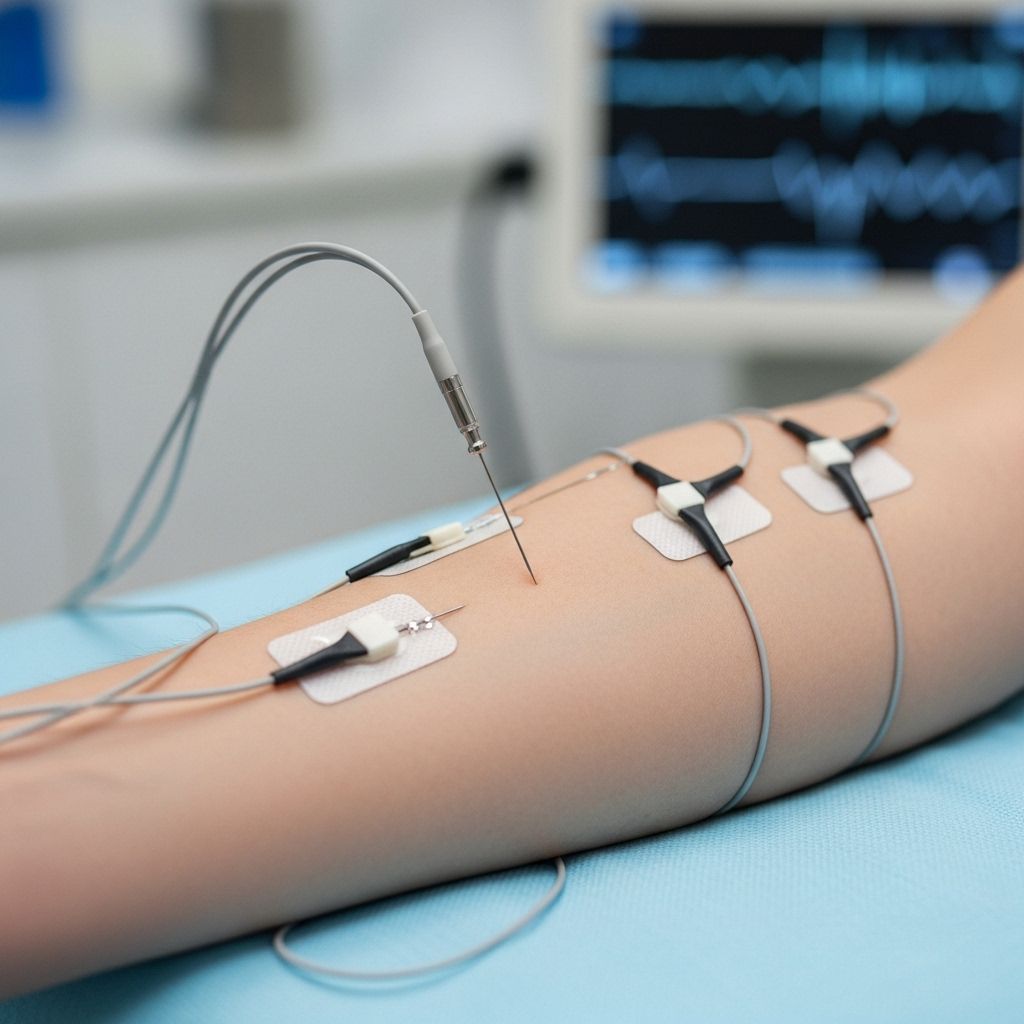
Electromyography (EMG) is a medical test that evaluates the health, function, and connectivity of skeletal muscles and the nerves that activate them. The procedure examines the electrical signals sent from the motor neurons to the muscle fibers, translating these signals into graphs, sounds, or numerical data for clinical interpretation. EMG is often coupled with nerve conduction studies to provide a comprehensive view of nerve and muscle activity.
- Purpose: Detects abnormal electrical activity or communication between nerves and muscles.
- Diagnostic Value: Helps identify nerve dysfunction, muscle disorders, and signal transmission problems.
- Technique: Uses electrodes placed on or in the muscle to record electric signals during muscle contraction and rest.
Why Is Electromyography (EMG) Performed?
EMG testing is recommended when patients exhibit symptoms suggestive of muscle or nerve dysfunction. Common indications include persistent muscle weakness, numbness, tingling, cramping, pain, or unexplained mobility issues with the limbs. Through EMG, physicians can pinpoint the root cause of these problems and tailor appropriate treatment strategies.
- Typical Symptoms Triggering EMG:
- Tingling or numbness
- Muscle weakness or loss of strength
- Muscle pain, cramps, spasms, or twitching
- Unexplained paralysis
- Persistent limb discomfort
- Common Conditions Diagnosed via EMG:
- Muscle disorders (e.g., muscular dystrophy, polymyositis)
- Nerve-to-muscle signal disorders (e.g., myasthenia gravis)
- Peripheral nerve conditions (e.g., carpal tunnel syndrome, neuropathies)
- Motor neuron diseases (e.g., amyotrophic lateral sclerosis [ALS])
- Root nerve pathologies (e.g., herniated disc)
If you're interested in understanding the heart's electrical activity alongside muscle diagnostics, take a look at our comprehensive guide to Electrocardiograms (ECG or EKG). This connection can shed light on how various conditions may affect both your heart and muscles, enhancing your overall health insight.
How Does EMG Work? The Basics of Muscle and Nerve Electrical Activity
Motor neurons transmit electrical signals from the spinal cord to muscles, triggering contraction and physical movement. EMG captures the patterns and strength of these reflected signals to help identify whether the muscle or nerve is functioning correctly. Abnormal readings often indicate issues such as muscle disease or nerve damage.
- Main Functions Monitored:
- Resting muscle electrical activity (baseline level)
- Response during voluntary muscle contraction
- Types of EMG Electrodes:
- Surface electrodes (stickers applied to skin)
- Needle electrodes (thin needles inserted into muscle tissue)
Preparing for an EMG Test
Preparation for EMG is typically straightforward. The test is usually done in an outpatient setting, such as a hospital or clinic, and does not require extensive pre-procedure protocols. However, some considerations help optimize the procedure’s accuracy and comfort:
- Avoid Applying Lotions or Oils: Refrain from using creams, lotions, or oils on the skin before the test, as these may interfere with electrode contact.
- Comfortable Clothing: Wear loose-fitting clothes that allow easy access to the area being tested.
- Medical History: Inform your provider about all medications, especially blood thinners; share any bleeding disorders or implanted electrical devices (such as pacemakers).
- Meals and Fasting: Most patients do not need to fast; regular meals are safe unless advised otherwise.
EMG Test Procedure: Step-by-Step
The EMG process involves two major components: the nerve conduction study and the needle EMG. Both parts are important for obtaining a comprehensive understanding of muscle and nerve function.
| Procedure Component | Description | What to Expect |
|---|---|---|
| Nerve Conduction Study (NCS) | Surface electrodes are attached to the skin to detect how electrical signals travel through nerves. | Small electrical impulses cause slight tingling or twitching. Evaluates nerve signal speed and strength. |
| Needle EMG | Thin needle electrodes are inserted into various muscles. These record electrical activity at rest and during contraction. | You may feel brief discomfort or stinging. The needle is removed after measurements are complete. |
- The overall test duration ranges from 30 to 60 minutes depending on the number of muscles and nerves examined.
- During the test, patients may be asked to change position or contract specific muscles.
- Data from both surface and needle electrodes is displayed as waveforms or audio signals.
After the EMG: What to Expect
Most people can resume normal activities immediately after EMG testing. It is common to experience mild discomfort, bruising, or soreness at needle insertion points, which typically resolves within hours.
- Post-Test Care: Minor soreness or bruising in the tested muscle areas is normal.
- Resuming Routine: No restrictions are generally necessary; you may return to work, driving, or exercise unless advised otherwise.
- Follow-Up: Your doctor will review and interpret results, often scheduling a follow-up discussion to explain findings and guide treatment.
EMG Risks and Possible Complications
EMG is considered a safe diagnostic procedure with minimal risks. Side effects, when they do occur, are usually mild and temporary.
- Discomfort: Temporary muscle soreness, minor bruising, and slight bleeding at needle sites.
- Infection: Extremely rare at needle insertion points if proper sterile technique is followed.
- Nerve Injury: Very rare; most adverse effects resolve quickly.
- Considerations for Special Populations: Patients with bleeding disorders or implanted electrical devices should notify providers, as modifications may be necessary.
EMG Test Results: How Are They Interpreted?
EMG findings are interpreted by a neurologist or specialist in physical medicine. Results reflect the electrical activity within muscles during rest and movement, helping distinguish between healthy and damaged tissue or nerves.
- Normal Results: Show muscle activity when contracted and minimal activity at rest.
- Abnormal Results:
- Unusual electrical patterns may indicate muscle disease (myopathy).
- Abnormal nerve conduction may reveal neuropathy or blocked nerve signals.
- Combined readings help diagnose complex neuromuscular disorders.
- Clinical Implications: The test helps clarify the location, severity, and nature of muscle and nerve involvement.
Common Medical Conditions Diagnosed by EMG
EMG can diagnose and help manage a spectrum of disorders affecting the muscles and nerves, including:
- Muscular dystrophy
- Polymyositis
- Myasthenia gravis
- Carpal tunnel syndrome
- Peripheral neuropathy
- Amyotrophic lateral sclerosis (ALS)
- Spinal nerve root compression (e.g., herniated disc)
- Guillain-Barré syndrome
- Other myopathies or neuropathies
Frequently Asked Questions (FAQs)
Q: Does an EMG test hurt?
A: Most patients experience mild discomfort during needle insertion, similar to a brief sting. The sensation is usually brief and well-tolerated. Surface electrode placement does not cause pain.
Q: How long does an EMG test take?
A: The procedure typically lasts between 30 and 60 minutes, depending on the complexity and number of areas being tested.
Q: Is EMG safe for children?
A: Yes, EMG is safe for children and adults. The test uses minimal electrical stimulation and sterile needles, with negligible risk of complications.
Q: Do I need to stop any medications before EMG?
A: Always discuss your medications with your provider before EMG testing. Some drugs, especially blood thinners, may require special handling.
Q: When will I receive my EMG results?
A: Results are usually available within a few days. Your healthcare provider will discuss the findings and recommended next steps during a follow-up visit.
Q: Can I drive or exercise after an EMG?
A: Yes, you may resume normal activities after EMG unless your healthcare provider gives specific advice otherwise.
Key Points to Remember About EMG
- EMG is a powerful tool for diagnosing muscle and nerve disorders affecting movement, force, and sensation.
- The procedure is minimally invasive, safe, and performed on an outpatient basis.
- Accurate interpretation of results helps direct treatment and rehabilitation for a wide array of neuromuscular conditions.
- If you’re experiencing unexplained muscle or nerve symptoms, EMG can yield crucial information for your health management.
For Patients: Tips for a Successful EMG Experience
- Communicate openly about your symptoms and medical history.
- Follow pre-test instructions regarding skin preparation and medication disclosure.
- Ask questions about the procedure, risks, and expected outcomes.
- Consult with your provider about your test results and recommended treatment plans.
Electromyography (EMG) continues to be a cornerstone in identifying and managing neuromuscular disorders, guiding therapy and improving patient outcomes. With proper preparation and understanding, EMG testing is a valuable step in regaining function, strength, and quality of life.
References
- https://www.healthline.com/health/electromyography
- https://www.mayoclinic.org/tests-procedures/emg/about/pac-20393913
- https://www.medicalnewstoday.com/articles/emg-test
- https://my.clevelandclinic.org/health/diagnostics/4825-emg-electromyography
- https://www.youtube.com/watch?v=AzLYAW_OeME
- https://www.pennmedicine.org/treatments/electromyography
- https://en.wikipedia.org/wiki/Electromyography
- https://www.hss.edu/health-library/conditions-and-treatments/emg-testing-a-patient-guide
Read full bio of medha deb












