Egg Freezing: Preserving Fertility for the Future
Comprehensive guide to egg freezing technology and fertility preservation options
Understanding Egg Freezing: A Modern Approach to Fertility Preservation
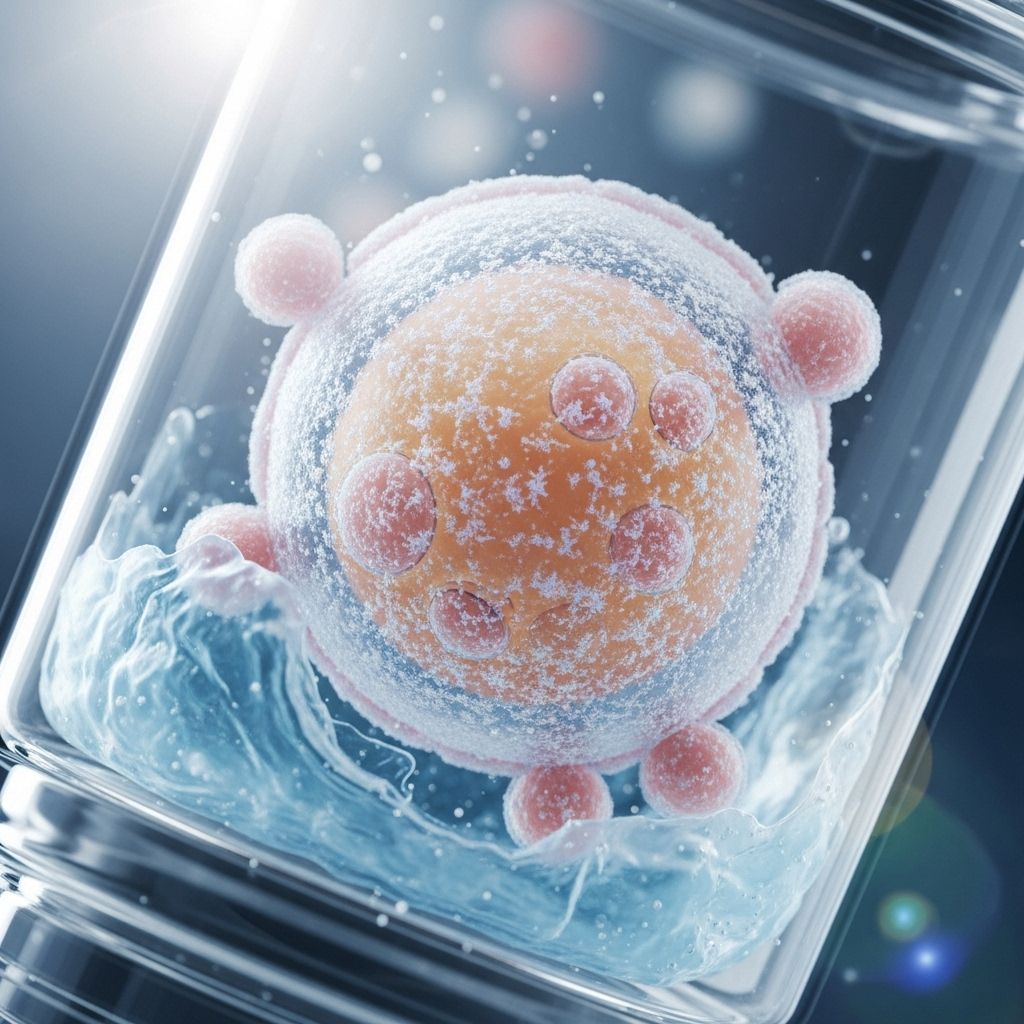
Egg freezing, medically known as oocyte cryopreservation, represents one of the most significant advances in reproductive medicine over the past decade. This innovative technology allows individuals with ovaries to preserve their fertility by extracting, freezing, and storing eggs for future use. What was once considered an experimental procedure has now become a mainstream option for family planning, offering hope and flexibility to those who wish to delay childbearing for personal, professional, or medical reasons.
The science behind egg freezing has evolved dramatically, with modern vitrification techniques achieving remarkable success rates. This flash-freezing method has transformed the landscape of fertility preservation, providing individuals with the opportunity to maintain their reproductive potential even as they age. Understanding this process can empower you to make informed decisions about your reproductive future.
The Science Behind Female Fertility and Aging
To appreciate the value of egg freezing, it’s essential to understand how female fertility changes over time. Individuals with female reproductive organs are born with approximately 6 million eggs at 20 weeks gestation – the highest number they will ever possess. This number drops significantly by birth, with about half of these eggs naturally lost during fetal development.
By puberty, only around 200,000 eggs remain, and this decline continues throughout a person’s reproductive years. The reduction in both egg quantity and quality accelerates with age, particularly after the mid-30s. In the early 20s, fertility begins its gradual decline, but conception rates remain relatively high through the early 30s. However, by the mid-30s, this decline becomes more pronounced, with pregnancy potential reaching minimal levels by the early 40s.
This age-related decline in fertility is accompanied by increased risks of chromosomal abnormalities, miscarriage, and other pregnancy complications. Women in their late 30s and early 40s face significantly higher risks of genetic abnormalities in their children due to age-dependent changes in egg quality.
How Egg Freezing Works: The Complete Process
The egg freezing process involves five distinct phases, each carefully orchestrated to maximize the number of viable eggs retrieved and preserved. Understanding each phase can help you prepare for what lies ahead and set realistic expectations for the journey.
Phase 1: Initial Consultation and Diagnostic Testing
Your egg freezing journey begins with a comprehensive consultation with a reproductive endocrinologist. During this initial meeting, your doctor will discuss your medical history, fertility goals, and the specifics of the egg freezing process. This consultation is crucial for determining whether you’re a good candidate for the procedure and developing a personalized treatment plan.
Diagnostic testing typically includes blood work to assess hormone levels and ovarian reserve function, as well as a transvaginal ultrasound to evaluate your ovaries and count the number of available follicles. These tests help your medical team design the optimal stimulation protocol for your unique physiology and predict how you might respond to fertility medications.
Phase 2: Ovarian Stimulation and Monitoring
The second phase involves stimulating your ovaries to produce multiple mature eggs simultaneously. Normally, your body releases only one egg per menstrual cycle, but fertility medications can encourage the development of multiple eggs at once, increasing the number available for freezing.
This phase typically begins with cycle synchronization using birth control pills or estrogen for 7-14 days. Following this preparation, you’ll begin daily hormone injections containing follicle-stimulating hormone (FSH) and luteinizing hormone (LH) – essentially concentrated versions of your body’s natural hormones. These medications are administered for an average of 8-12 days.
During stimulation, you’ll visit your fertility clinic every 2-3 days for monitoring appointments. These visits include ultrasounds to track follicle growth and blood tests to monitor hormone levels. Your medical team will adjust medication dosages based on your body’s response, ensuring optimal egg development while minimizing risks.
As your follicles approach maturity, a third medication called a GnRH antagonist is typically added to prevent premature ovulation. Once several follicles reach the appropriate size, you’ll stop the stimulation medications and administer a “trigger shot” containing human chorionic gonadotropin (hCG) or a GnRH agonist. This injection finalizes the egg maturation process and must be timed precisely.
Phase 3: Egg Retrieval
The egg retrieval procedure occurs 36-37 hours after your trigger shot. This outpatient procedure is performed under conscious sedation to ensure your comfort throughout the process. Using transvaginal ultrasound guidance, your doctor will insert a thin needle through the vaginal wall to access each mature follicle in your ovaries.
The follicular fluid containing the eggs is gently aspirated through the needle, and the entire procedure typically takes 15-30 minutes. Most patients experience minimal discomfort and can return home within a few hours of the procedure. You may experience mild cramping, bloating, or spotting for a day or two following retrieval, but these symptoms generally resolve quickly.
Phase 4: Egg Assessment and Vitrification
Once retrieved, your eggs are immediately transported to the laboratory where embryologists assess their maturity and quality. Only mature eggs (those in metaphase II of meiosis) are suitable for freezing, as immature eggs have lower survival and fertilization rates after thawing.
The mature eggs undergo vitrification, a rapid freezing process that prevents ice crystal formation within the egg. This flash-freezing technique has revolutionized egg preservation, achieving survival rates of 90-95% after thawing. The vitrified eggs are then stored in liquid nitrogen at -196°C, where they can remain viable for many years.
Phase 5: Future Use – Thawing and Fertilization
When you’re ready to use your frozen eggs, they will be thawed and fertilized through intracytoplasmic sperm injection (ICSI), where a single sperm is directly injected into each egg. The resulting embryos are cultured in the laboratory for several days before being transferred to the uterus or stored for future use.
Optimal Timing for Egg Freezing
The timing of egg freezing is crucial for maximizing success rates and preserving the highest quality eggs possible. Most fertility specialists recommend egg freezing in the late 20s to early 30s, with any age before 35 considered optimal. During this period, eggs are typically of higher quality, and ovarian reserve is still robust.
However, fertility preservation at any age is better than no preservation at all. Women between ages 30-40 can still benefit from egg freezing, though success rates may be lower, and more cycles might be needed to achieve adequate egg numbers. The decision should be individualized based on personal circumstances, medical history, and reproductive goals.
Who Should Consider Egg Freezing?
Egg freezing can benefit various groups of individuals facing different circumstances:
Career and Life Planning: Women who wish to focus on career advancement, education, or personal goals before starting a family can use egg freezing to preserve their fertility potential while pursuing other priorities.
Medical Circumstances: Individuals facing cancer diagnosis or other medical treatments that may compromise fertility should consider egg freezing before beginning treatment. Chemotherapy, radiation, and certain medications can significantly impact egg quality and quantity.
Family History: Those with a family history of early menopause or premature ovarian failure may benefit from freezing eggs at a younger age to preserve their reproductive potential.
Relationship Status: Single individuals who haven’t found a partner but want biological children in the future can use egg freezing as insurance against age-related fertility decline.
Gender Transition: Individuals planning to transition with hormone therapy or gender-affirming surgery can preserve their fertility through egg freezing before beginning treatment.
Success Rates and Expectations
Understanding realistic expectations for egg freezing success is crucial for making informed decisions. Success rates depend on several factors, including age at freezing, number of eggs retrieved, and individual medical circumstances.
Generally, younger women have higher success rates. Women who freeze eggs before age 35 typically have better outcomes than those who freeze after 35. The number of eggs frozen also impacts success rates – most specialists recommend retrieving 15-20 mature eggs to optimize the chances of future pregnancy.
It’s important to remember that egg freezing is not a guarantee of future pregnancy. While modern vitrification techniques achieve excellent egg survival rates, not all thawed eggs will fertilize successfully, and not all resulting embryos will lead to pregnancy. Multiple factors influence the ultimate success of using frozen eggs, including the quality of sperm used for fertilization, uterine health at the time of embryo transfer, and individual reproductive factors.
Timeline and What to Expect
The entire egg freezing process, from initial consultation to egg retrieval, typically takes 6-8 weeks. This timeline includes time for consultation, diagnostic testing, and the actual stimulation cycle. The active treatment portion – from starting medications to egg retrieval – takes approximately 2-3 weeks.
For individuals facing urgent medical situations, such as cancer diagnosis, fertility clinics can often expedite the process to accommodate treatment schedules. Many clinics work closely with oncologists to coordinate care and ensure timely fertility preservation before beginning cancer treatment.
Frequently Asked Questions
Q: Is egg freezing painful?
A: Most women experience minimal discomfort during the egg freezing process. The daily hormone injections may cause mild bruising or soreness at injection sites. The egg retrieval procedure is performed under sedation, so you won’t feel pain during the procedure. Some mild cramping and bloating may occur afterward, but this typically resolves within a day or two.
Q: How many eggs should I freeze?
A: The ideal number depends on your age and reproductive goals. Generally, freezing 15-20 mature eggs provides the best chance of future pregnancy success. Younger women may need fewer eggs, while those over 35 might benefit from freezing more eggs or undergoing multiple cycles.
Q: How long can frozen eggs be stored?
A: Frozen eggs can be stored indefinitely in liquid nitrogen at -196°C. There’s no evidence that storage duration affects egg quality or viability. Eggs frozen for 10+ years have successfully resulted in healthy pregnancies.
Q: Can I use my frozen eggs for multiple pregnancies?
A: Yes, if you freeze an adequate number of eggs, you may be able to use them for multiple pregnancies. However, this depends on factors like your age at freezing, the number of eggs retrieved, and success rates of fertilization and embryo development.
Q: What are the risks of egg freezing?
A: Egg freezing is generally safe with minimal risks. Potential complications include ovarian hyperstimulation syndrome (OHSS), mild bleeding or infection from the retrieval procedure, and rare allergic reactions to medications. Serious complications are very uncommon when performed by experienced fertility specialists.
Making the Decision: Is Egg Freezing Right for You?
Deciding whether to freeze your eggs is a personal choice that should be made after careful consideration of your individual circumstances, goals, and values. Consulting with a reproductive endocrinologist can help you understand your specific fertility situation and the potential benefits and limitations of egg freezing in your case.
Consider factors such as your current age, career goals, relationship status, family history, and personal timeline for having children. Remember that while egg freezing can provide peace of mind and extend your reproductive window, it’s not a guarantee of future pregnancy success.
The most empowering aspect of egg freezing is that it provides options and flexibility in your reproductive journey. By taking proactive steps to preserve your fertility, you’re investing in your future ability to start a family when the time is right for you, regardless of the biological clock.
References
- https://www.shadygrovefertility.com/treatments/egg-freezing/
- https://www.illumefertility.com/fertility-blog/how-does-egg-freezing-work
- https://progyny.com/education/egg-freezing/understanding-the-egg-freezing-process
- https://www.healthline.com/health/egg-freezing-process
- https://my.clevelandclinic.org/health/treatments/17000-fertility-preservation
- https://www.brighamandwomens.org/obgyn/infertility-reproductive-surgery/fertility-preservation
- https://www.emoryhealthcare.org/centers-programs/reproductive-center/treatments/egg-freezing-fertility-preservation
Read full bio of Sneha Tete












