The Effects of Insulin on the Body: How This Key Hormone Shapes Health
Discover how insulin works, its essential role in metabolism, and what happens when things go wrong.
The Effects of Insulin on the Body
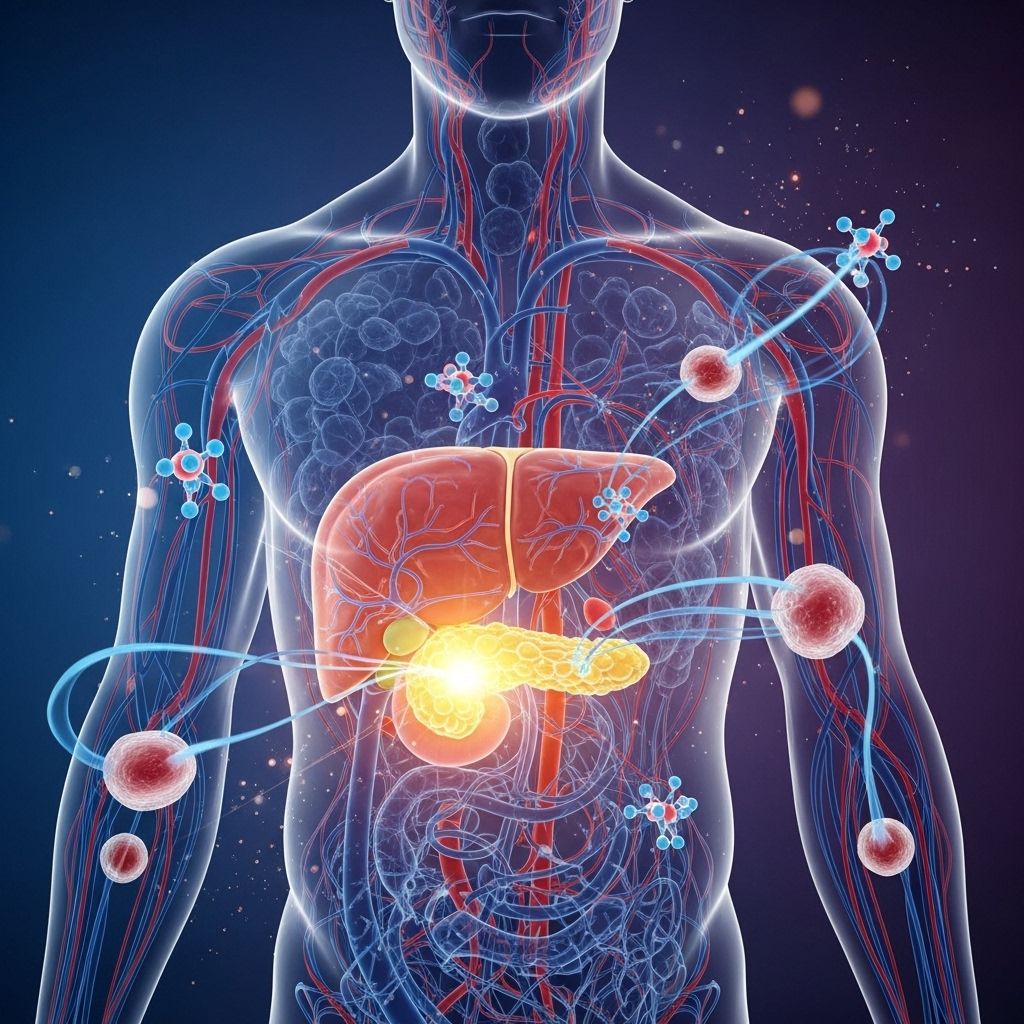
Insulin is a natural hormone your pancreas produces to control how your body uses and stores blood sugar (glucose). It acts as a key, allowing glucose to enter the cells that fuel your daily life. Understanding insulin’s functions—and what happens if those functions are disrupted—is vital for everyone, especially people with diabetes.
What Is Insulin?
Insulin is a hormone released by the pancreas in response to elevated blood glucose levels, such as after eating. Its main job is to facilitate the movement of glucose from your bloodstream into your cells, powering muscles, organs, and the brain. Without insulin, your body’s metabolism and basic cellular functions quickly break down.
Core Functions of Insulin
- Regulates blood sugar: Maintains safe and stable glucose levels in the blood.
- Supports metabolism: Helps your body convert food into usable energy.
- Stores excess energy: Signals the liver and muscles to store extra glucose as glycogen, and fat tissue to store it as fat for later use.
- Builds muscle mass: Helps amino acids enter cells, a critical step in protein synthesis.
- Balances electrolytes: Aids in cellular uptake of potassium, ensuring stable nerve and muscle function.
How Insulin Works in the Body
Every time you eat, carbohydrates are broken down into glucose. This glucose is absorbed into the bloodstream, and the pancreas releases insulin to help cells access and use the glucose for energy or store it for later. Without enough insulin—or if your body cannot respond properly to it—glucose builds up in the blood, eventually causing damage to organs, blood vessels, and nerves.
Step-by-Step: The Insulin-Glucose Process
- You eat foods containing carbohydrates.
- Carbohydrates are broken down into glucose in your digestive tract.
- Blood sugar levels rise, prompting the pancreas to produce and release insulin.
- Insulin acts as a key, allowing glucose to move from the blood into the body’s cells.
- Cells use the glucose for immediate energy; excess amounts are stored in the liver, muscles, or as body fat.
Types of Diabetes and Insulin’s Role
Problems with insulin underlie all forms of diabetes, but the exact mechanisms differ:
| Condition | Insulin Production | Cellular Response |
|---|---|---|
| Type 1 Diabetes | Little or none (autoimmune destruction of pancreatic cells) | Not applicable — insulin must be supplied externally |
| Type 2 Diabetes | Initially normal, then may decline over time | Impaired (insulin resistance) |
| Prediabetes | Normal to high | Reduced (early insulin resistance) |
Type 1 diabetes means the pancreas can no longer produce insulin; people need daily insulin therapy to stay alive. In type 2 diabetes, the body produces insulin but becomes resistant, so the cells don’t respond as well, requiring more insulin than normal to keep blood sugar in check.
Insulin Therapy: What Is It, and Who Needs It?
People with type 1 diabetes require insulin to survive. Many with type 2 diabetes also need it when oral medications and lifestyle changes alone can’t maintain target blood sugar levels. Insulin can be delivered by injection, pen, or pump, and is carefully dosed to match dietary intake and activity.
Types of Insulin Used in Treatment
- Rapid-acting insulin: Works within 15 minutes; duration up to 4 hours.
- Short-acting insulin: Starts working in 30 minutes; lasts 6 hours.
- Intermediate-acting insulin: Takes 2–4 hours to activate; effective for about 18 hours.
- Long-acting insulin: Begins after a few hours and stabilizes glucose for up to 24 hours.
Dosing is determined by blood sugar monitoring, meal timing, and activity levels. Insulin therapy is often adjusted individually and monitored closely by healthcare providers.
The Importance of Balanced Blood Sugar
Blood glucose provides the primary source of energy for your cells. Insulin keeps blood sugar within a tight, healthy range by ensuring that just enough is available for immediate needs and that excess is safely stored.
What Happens With Too Much or Too Little Glucose?
- Hyperglycemia (high blood sugar): Excess glucose damages blood vessels, nerves, kidneys, eyes, and heart. Common symptoms include thirst, frequent urination, fatigue, and blurred vision.
- Hypoglycemia (low blood sugar): If insulin levels are too high relative to glucose intake, you may feel irritable, shaky, confused, or even lose consciousness. Severe hypoglycemia is an emergency and can be life-threatening.
Insulin’s Key Effects on Body Systems
1. Cellular Health and Energy
All body cells require glucose for energy. Without insulin, glucose cannot enter these cells, leading to energy starved tissues. Over time, this weakens the body, delays healing, and can lead to life-threatening complications.
2. Protein & Fat Metabolism
- Insulin promotes the storage of glucose as glycogen in muscles and liver for later use.
- It also helps cells absorb amino acids, supporting muscle growth and repair.
- Insulin inhibits the breakdown of fat for energy, encouraging fat storage — a key reason why dysregulated insulin can contribute to weight gain or loss depending on overall balance.
3. Potassium and Electrolyte Balance
Insulin helps move potassium into cells, affecting heart rhythm, nerve impulses, and muscle contraction. Improper levels can cause dangerous shifts in electrolyte balance, resulting in arrhythmias or muscle weakness.
What Happens When Insulin Doesn’t Work?
Insulin Resistance
Insulin resistance occurs when body cells stop responding properly to insulin, so the pancreas produces more and more. This is the primary problem in type 2 diabetes and prediabetes. Risk factors include obesity, inactivity, genetics, and some medical conditions. Insulin resistance increases the risk for heart disease, fatty liver, and certain cancers.
Lack of Insulin: Type 1 Diabetes
Without adequate insulin (as in type 1 diabetes), glucose cannot reach the body’s cells. The body, starved for energy, begins breaking down fat and protein for fuel instead, causing dangerous byproducts called ketones and leading to a life-threatening condition called diabetic ketoacidosis if not treated.
Hyperinsulinemia
This describes abnormally high insulin levels, often seen in the early stages of type 2 diabetes due to insulin resistance. Chronically high insulin can worsen resistance and drive weight gain, increase inflammation, and raise the risk of heart disease.
Consequences of Poorly Managed Insulin
Failure to control insulin levels and blood sugar over time can lead to:
- Kidney disease (diabetic nephropathy)
- Nerve damage (diabetic neuropathy)
- Heart complications (heart attack, stroke, atherosclerosis)
- Eye disease (diabetic retinopathy, possible blindness)
- Foot and skin problems due to poor blood flow and nerve function
- Gastroparesis (stomach emptying problems)
- Mental health impacts like depression and anxiety
Insulin and Weight Gain: What’s the Connection?
Insulin is a storage hormone: it helps the body save excess energy as fat. People who start insulin therapy, especially for type 2 diabetes, may notice weight gain. This occurs because their bodies are finally able to process and store glucose again rather than expelling it through urine. In some cases, people eat extra carbs to prevent low blood sugar, worsening the issue.
- Strategies to minimize weight gain with insulin therapy include healthy diet planning, regular physical activity, and careful monitoring of carb intake.
How to Keep Your Insulin in Balance
- Follow your diabetes care plan: Take medications as prescribed, check blood glucose regularly, and attend medical appointments.
- Eat a balanced diet: Choose high-fiber carbs, lean proteins, and healthy fats. Limit processed foods and added sugars.
- Exercise regularly: Activity helps cells use insulin more efficiently and improves insulin sensitivity.
- Manage weight: Maintaining a healthy weight reduces insulin resistance and supports better glucose control.
- Limit stress and get enough sleep: Both stress and poor sleep can increase insulin resistance.
Blood Testing and Insulin Monitoring
Blood glucose tests (fasting, random, and A1C) are the primary method for measuring how well your body is responding to insulin. Elevated levels suggest insulin resistance or insufficient insulin. Consistently low values may indicate excess insulin or overtreatment. Your healthcare provider may also test insulin levels directly, especially if unexplained metabolic symptoms persist.
Frequently Asked Questions (FAQs)
Q: What does insulin do in simple terms?
A: Insulin helps your body use sugar from food as energy and stores any surplus, keeping blood sugar at safe, stable levels.
Q: Why do people with diabetes need insulin therapy?
A: In type 1 diabetes, the pancreas cannot make insulin. In some type 2 cases, the body doesn’t produce enough or can’t use it properly. Insulin therapy ensures blood sugar is controlled to prevent complications.
Q: Can insulin therapy cause weight gain?
A: Yes. As insulin helps store glucose as fat, people starting therapy sometimes gain weight, but this can be managed through healthy eating and exercise habits.
Q: What are signs of too much or too little insulin?
A: Too much insulin can cause low blood sugar symptoms: shakiness, confusion, sweating, or loss of consciousness. Too little causes high blood sugar: thirst, frequent urination, and fatigue.
Q: What happens if diabetes is left unmanaged?
A: Unmanaged diabetes leads to dangerous complications including kidney, nerve, and heart damage, vision loss, and potentially life-threatening emergencies like diabetic ketoacidosis.
Takeaway
Insulin is indispensable to health, ensuring cells get the energy they need, blood sugar stays in check, and organs function optimally. For those living with diabetes, proactive management, including insulin therapy when needed and healthy lifestyle choices, is key to reducing complications and living well.
References
- https://www.medicalnewstoday.com/articles/325328
- https://www.healthline.com/health/diabetes/insulin-effects-on-body
- https://www.medicalnewstoday.com/articles/323729
- https://www.healthline.com/nutrition/insulin-and-insulin-resistance
- https://www.healthline.com/health/video/the-complete-guide-to-insulin-and-how-to-use-it
- https://my.clevelandclinic.org/health/diseases/7104-diabetes
- https://www.healthline.com/health/video/insulin-resistance-diet
- https://www.healthline.com/health/video/blood-sugar-spike
- https://www.healthlinedme.com/Resource-Center/Medical-Health-Issues?issue=Diabetes
- https://www.news-medical.net/health/Insulins-role-in-the-human-body.aspx
Read full bio of Sneha Tete












