Dysentery: Causes, Symptoms, Treatment, and Prevention
Discover essential facts on dysentery, its types, causes, symptoms, complications, and effective prevention and treatment strategies.
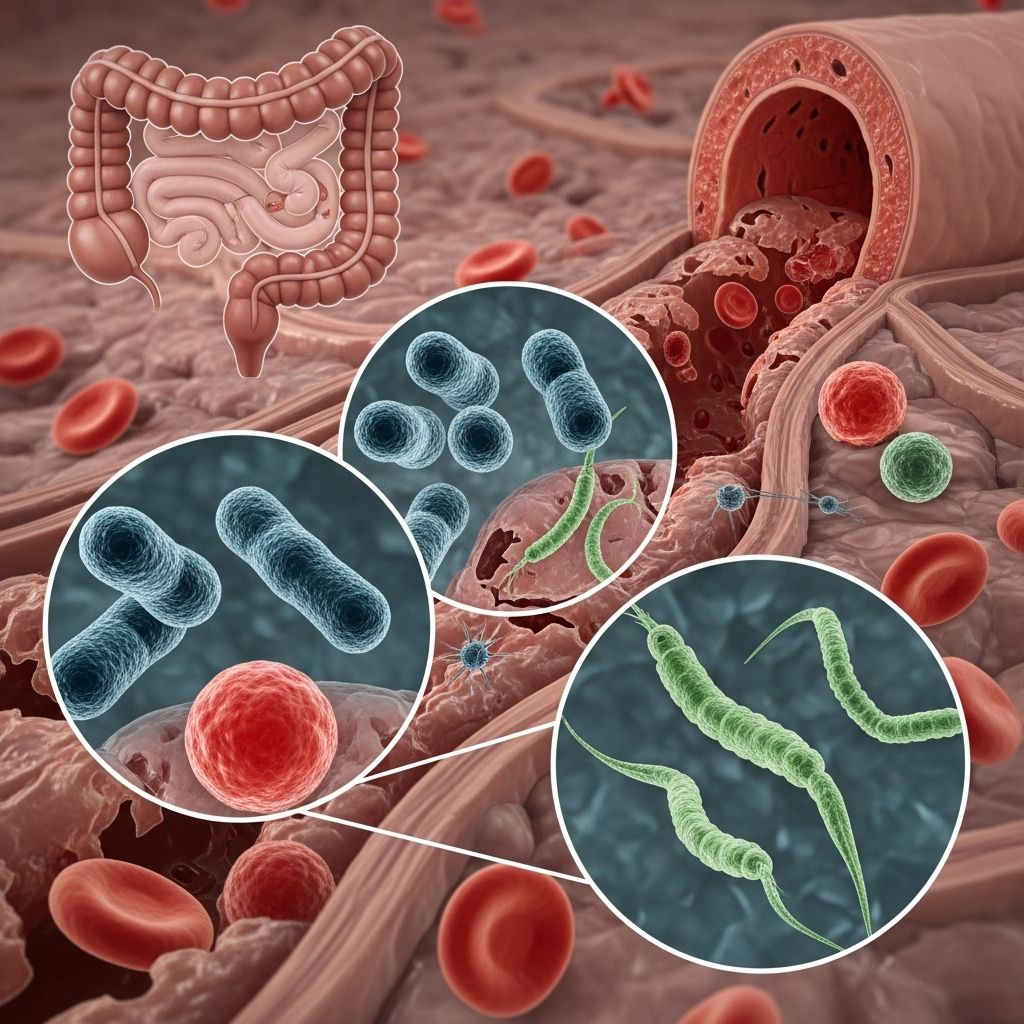
What Is Dysentery?
Dysentery is a serious intestinal infection characterized chiefly by bloody diarrhea and, in many cases, mucus in the stool. Typically, an episode lasts 3 to 7 days, but in severe cases, it may persist longer.
Other accompanying symptoms can include:
- Abdominal cramps or pain
- Nausea
- Vomiting
- Fever over 100.4°F (38°C)
- Signs of dehydration (dry mouth, dizziness, reduced urination)
Dysentery can be life-threatening if not promptly managed, especially when dehydration occurs or in vulnerable populations such as children, older adults, and people with weakened immune systems.
Types of Dysentery
Dysentery most commonly presents as one of two types, differentiated by cause:
- Bacterial Dysentery: Primarily caused by Shigella bacteria, but may also result from Campylobacter, Salmonella, or enterohemorrhagic E. coli. The most prevalent bacterial form is shigellosis, which constitutes around 500,000 diagnosed cases annually in the United States.
- Amebic Dysentery: Also known as amebiasis, this form stems from infection with the Entamoeba histolytica parasite. Amebic dysentery is less common in developed countries, tending to affect people in tropical regions with poor sanitation, or travelers returning from those regions.
| Type | Main Cause | Common Regions | Transmission |
|---|---|---|---|
| Bacterial (Shigellosis) | Shigella and other bacteria | Worldwide, mainly in areas with poor sanitation | Person-to-person, contaminated food/water |
| Amebic (Amebiasis) | Entamoeba histolytica | Tropical regions with poor sanitation | Contaminated food/water, travel to high-risk areas |
Viruses are not common causes of dysentery. Rarely, certain chemicals or other protozoa and parasitic worms may also be implicated.
Causes and Risk Factors
Dysentery is almost always linked to poor hygiene and sanitation practices. The primary mechanism is the oral ingestion of infectious organisms present in food, water, or through hand-to-mouth contact with contaminated surfaces. Transmission routes include:
- Eating contaminated food
- Drinking or using contaminated water (for drinking, bathing, or recreation)
- Poor handwashing practices after toilet use
- Swimming in contaminated pools, lakes, or rivers
- Person-to-person contact (especially in close quarters)
Risk factors for dysentery include:
- Living or traveling in developing countries/tropical regions with inadequate sanitation
- Being a child (especially under 5 years old)
- Attending childcare centers, schools, or nursing homes
- Having close contact with an infected person
Both shigellosis and amebic dysentery are easily spread in environments where people are in close proximity—such as households, daycare centers, schools, or care facilities.
Symptoms of Dysentery
The hallmark symptom is diarrhea that contains visible blood. Other gastroenteritis symptoms commonly occur:
- Abdominal pain or cramping
- Nausea and vomiting
- Fever and chills
- Dehydration signs (thirst, dry lips/mouth, dark urine, reduced urine output)
- Occasional presence of mucus in the stool
Symptoms can vary in severity, sometimes resolving on their own but potentially leading to severe, prolonged illness, especially in high-risk groups. Mild cases may mimic other stomach infections, but any diarrhea with blood should be evaluated by a healthcare provider.
Diagnosis
If dysentery is suspected, a healthcare provider will ask about recent travel, exposure to sick individuals, and symptoms. Diagnosis typically involves:
- Physical examination and medical history assessment
- Lab analysis of stool samples (to identify bacteria, parasites, or presence of blood/mucus)
- Blood tests (when severe illness or complications are suspected)
Identifying the specific cause of dysentery guides effective treatment and helps prevent further spread.
Treatment Options
Treatment for dysentery depends on the underlying cause and severity of symptoms:
- Hydration: The cornerstone of management. Includes oral rehydration solutions, clear fluids, and electrolyte replacement. IV fluids may be required if dehydration is severe.
- Antibiotics:
- Bacterial dysentery (e.g., shigellosis) often requires antibiotics such as azithromycin or ciprofloxacin.
- Parasitic (amebic) dysentery is treated with specific anti-parasitic medications like metronidazole or tinidazole.
- Over-the-counter medications: Anti-diarrheal drugs (like loperamide) are not recommended alone for bloody diarrhea, but may be used cautiously alongside antibiotics under doctor supervision.
- Supportive care: Maintaining good nutrition, rest, and monitoring for complications.
Most cases resolve in about one week, but severe cases may require hospitalization.
Complications of Dysentery
- Severe dehydration (may require hospitalization and IV fluids)
- Electrolyte imbalance affecting heart, nerves, and muscles
- Kidney failure in extreme cases
- Abscesses (rare, typically with amebic dysentery)
- Long-term gut motility issues after severe infection
- Anemia from chronic blood loss
- Systemic infection if bacteria or parasites spread to other organs
Children, older adults, and immunocompromised individuals are at greatest risk of serious complications.
Outlook (Prognosis)
Most people with mild bacterial dysentery make a full recovery within days to a week, provided they maintain proper hydration. Severe or untreated cases can be life-threatening, especially in populations with limited access to medical care. Amebic dysentery is more likely to cause persistent symptoms and complications if not effectively treated.
Access to prompt medical care and supportive measures improves outlook considerably.
Prevention: How to Avoid Dysentery
A combination of good personal hygiene and food/water safety practices can help prevent dysentery, especially in high-risk regions:
- Thorough hand washing: Especially after toilet use and before handling food.
- Safe drinking water: Use bottled or boiled water where sanitation is uncertain.
- Proper food handling: Ensure food is cooked thoroughly and served hot.
- Avoid raw or unpeeled produce: Especially in settings with uncertain sanitation.
- Disinfect surfaces regularly: Especially in shared environments (schools, daycare, healthcare settings).
- Check sanitation before swimming: Avoid swimming in water likely contaminated by fecal matter.
Handwashing and improved sanitation remain the most effective preventive steps.
Frequently Asked Questions (FAQs)
Q: Who is most at risk of getting dysentery?
Children, especially those in childcare or school settings, and travelers to developing countries are at highest risk. Close contact in nursing homes is also a common setting for bacterial dysentery transmission.
Q: Can dysentery go away without treatment?
Mild cases, particularly in healthy adults, may resolve on their own with proper hydration. However, all cases with bloody diarrhea should be evaluated by a healthcare provider, as complications can be severe, and antibiotics may be necessary.
Q: How quickly do symptoms appear after exposure?
Symptoms may develop anywhere from a few hours to several days following exposure to the infectious organism.
Q: Is dysentery contagious?
Yes—dysentery, especially the bacterial type, is easily spread through close contact, contaminated surfaces, and food/water.
Q: What should I eat or drink if I have dysentery?
Focus on clear fluids, oral rehydration solutions, and bland foods such as rice, bananas, or toast. Avoid dairy, fatty foods, and foods high in fiber until the illness improves.
Q: Can dysentery be fatal?
Untreated severe cases, especially in vulnerable people, may lead to life-threatening dehydration, kidney failure, or other complications. Prompt care can prevent most deaths.
Key Takeaways
- Dysentery causes bloody diarrhea, abdominal pain, and dehydration.
- Most cases are bacterial (shigellosis) or amoebic (amebiasis).
- Good hygiene and sanitation are vital for prevention.
- Rapid treatment—primarily focused on hydration and targeted medications—reduces risk of complications.
- Contact a healthcare provider for any bloody diarrhea, persistent symptoms, or signs of dehydration.
References
- https://en.wikipedia.org/wiki/Dysentery
- https://www.healthline.com/health/digestive-health/dysentery
- https://www.medicalnewstoday.com/articles/171193
- https://www.healthline.com/health/difference-between-gastroenteritis-and-dysentery
- https://my.clevelandclinic.org/health/drugs/23567-dysentery
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6021764/
- https://www.britannica.com/science/dysentery
- https://www.who.int/news-room/fact-sheets/detail/diarrhoeal-disease
Read full bio of Sneha Tete












