Understanding the Progression from Dry to Wet Age-Related Macular Degeneration (AMD)
Learn how and why dry AMD can progress to wet AMD, what it means for your vision, and steps for management.
Age-related macular degeneration (AMD) is a leading cause of vision loss among older adults. While dry AMD is more common, wet AMD can cause rapid and severe visual impairment. This article discusses how and why dry AMD can progress to wet AMD, what that means for your vision, and what steps you can take to monitor, prevent, or treat these conditions.
What Is Age-Related Macular Degeneration (AMD)?
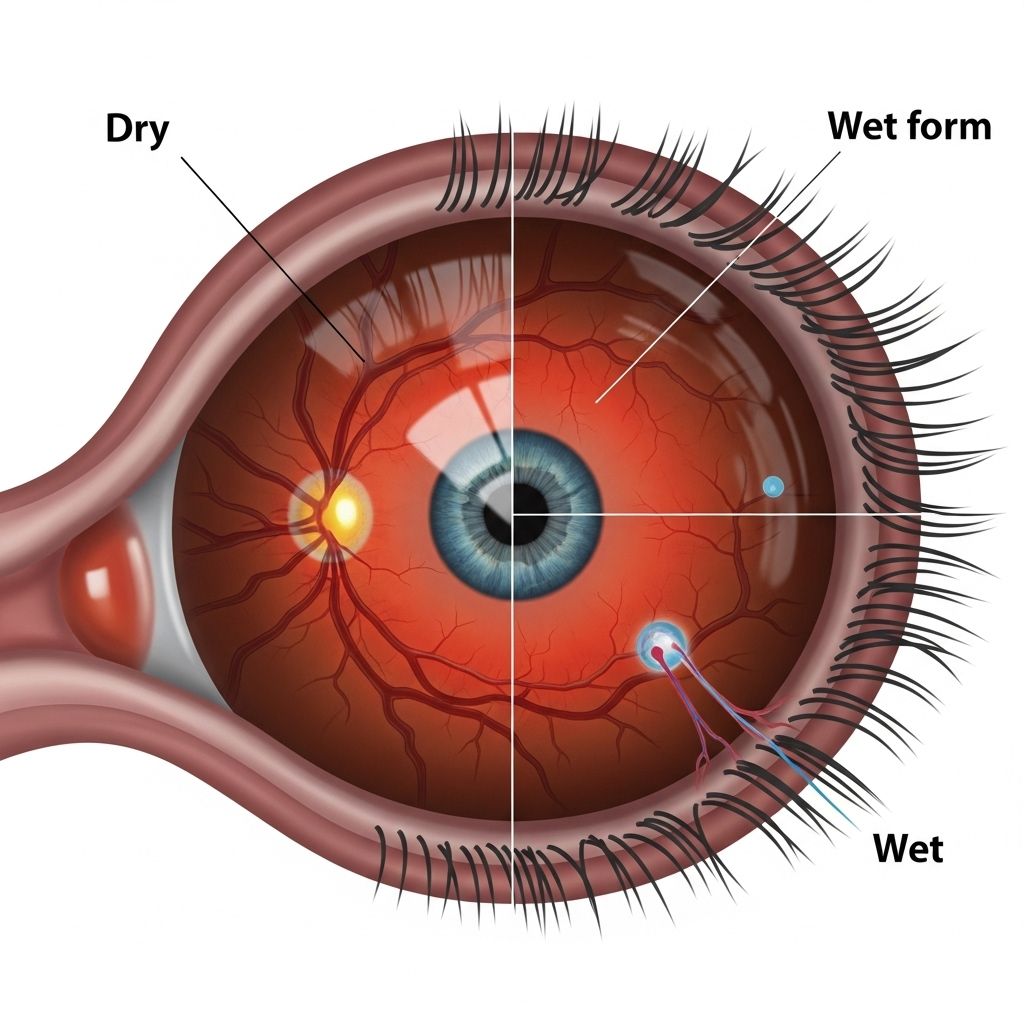
AMD is an eye condition involving the breakdown of the macula, the part of the retina responsible for clear central vision. There are two main types:
- Dry AMD (atrophic): The more common form, caused by gradual thinning of the macula as retinal cells break down and drusen (tiny deposits) build up under the retina.
- Wet AMD (neovascular): The less common but more severe form, occurring when abnormal blood vessels grow under the retina, leaking blood and fluid.
How Common Is Progression from Dry to Wet AMD?
Most people diagnosed with AMD initially have the dry form. According to the National Eye Institute, around 10-15% of dry AMD cases can progress to wet AMD over time, typically in advanced stages.
- Dry AMD accounts for about 85-90% of all AMD cases.
- Wet AMD, although less common, is responsible for about 90% of cases of severe vision loss from AMD.
Why and How Does Dry AMD Progress to Wet AMD?
The process by which dry AMD transitions to wet AMD is not entirely understood, but several factors play a role:
- Accumulation of Drusen: Drusen are yellowish deposits under the retina. As their number and size increase, retinal cells become progressively stressed and die.
- Retinal Damage: Chronic cell loss in the macula can disrupt normal function and structure, potentially triggering the growth of abnormal blood vessels beneath the retina.
- Neovascularization: In wet AMD, these abnormal blood vessels grow rapidly, leading to leakage of blood and fluid, which can cause sudden central vision loss.
Not everyone with dry AMD will develop wet AMD, but the risk increases with disease progression and severity.
What Are the Symptoms of Dry and Wet AMD?
| Symptom | Dry AMD | Wet AMD |
|---|---|---|
| Onset | Gradual vision changes, often over years | Sudden, dramatic vision changes (days or weeks) |
| Vision Distortion | Blurriness in central vision, fading colors | Wavy or crooked lines, blind spots, rapid vision loss |
| Light Sensitivity | Difficulty adapting to low light | May occur, often with more severe vision changes |
| Blind Spots | Small dark or blurry spots may develop in the center | Larger, more noticeable central blind spots |
Risk Factors for Progression from Dry to Wet AMD
While the exact cause of AMD is multifactorial, factors that increase the risk of progression include:
- Age: The risk increases significantly after age 60.
- Genetics: Family history of AMD or certain gene variants contribute.
- Smoking: Doubles the risk of AMD and its progression.
- High blood pressure and cardiovascular disease.
- Poor diet or obesity.
- Race: Caucasians are at higher risk.
- Ocular factors: Large drusen, pigment changes, and advanced dry AMD in one eye increase risk in the other.
How Is the Progression from Dry to Wet AMD Diagnosed?
Regular dilated eye exams are vital for detecting AMD and any signs of progression:
- Ophthalmoscopy: Allows your eye doctor to see drusen and changes to the macula.
- Optical Coherence Tomography (OCT): Provides detailed cross-sectional images, revealing thinning, fluid, or new vessels.
- Fluorescein Angiography: Uses a dye to detect leaking blood vessels characteristic of wet AMD.
- Amsler Grid Test: At-home monitoring test; new distortion or missing squares can signal wet AMD development.
What Should I Do If I Notice Vision Changes?
- Act quickly: Sudden vision changes—such as wavy lines or new blind spots—require immediate assessment by an eye specialist.
- Regular monitoring: Even without symptoms, routine eye exams are crucial for early detection.
- Communication: Inform your doctor of any family history, other eye conditions, or rapid changes.
Managing the Risk: Can I Prevent Dry AMD from Turning Into Wet AMD?
There is no way to guarantee prevention of progression, but you can reduce risk:
- Don’t smoke: Quitting can significantly reduce the progression risk.
- Diet: Eat a diet rich in leafy greens, colorful fruits and vegetables, omega-3s, and whole grains.
- Supplements: High-dose antioxidant vitamins and zinc, following the Age-Related Eye Disease Study (AREDS) formula, may slow progression in intermediate or advanced dry AMD.
- Control health conditions: Managing blood pressure and heart disease can help protect your eyes.
- Eye protection: Wear sunglasses to block UV rays.
- Monitor vision regularly: Early detection greatly improves treatment outcomes.
Treatment Options for Wet AMD
If wet AMD develops, early intervention is key to preserving vision. Treatments include:
- Anti-VEGF injections: Medications such as ranibizumab, aflibercept, or bevacizumab injected into the eye stop new blood vessel growth and reduce leaking.
- Photodynamic therapy: Uses a light-activated drug to target abnormal vessels.
- Laser therapy: Sometimes used to destroy leaking blood vessels, but less common than injections today.
These treatments aim to stop vision loss, but typically do not restore vision already lost.
Comparing Dry and Wet AMD: Key Differences
| Feature | Dry AMD | Wet AMD |
|---|---|---|
| Prevalence | Most common (85-90% of cases) | Less common (10-15% of cases) |
| Progression | Slow (years) | Rapid (days to weeks) |
| Primary Issue | Drusen buildup, macular thinning | New abnormal blood vessels under macula |
| Vision Loss | Mild to moderate, gradual | Severe, sudden if untreated |
| Treatment Focus | Lifestyle, nutrition, supplements | Injections, occasionally laser or light therapy |
| Potential for Vision Restoration | Limited | Visual decline can often be stopped, not reversed |
Frequently Asked Questions (FAQs)
Can dry AMD always progress to wet AMD?
No. Most cases of dry AMD never progress to wet AMD. Regular monitoring can detect those at risk and facilitate early intervention.
Are there symptoms unique to wet AMD?
Yes. Wet AMD often presents with sudden vision changes, such as wavy or distorted lines and larger central blind spots, unlike the slow progression of dry AMD.
If one eye develops wet AMD, will the other eye do the same?
The risk increases if one eye has wet AMD, but it is not guaranteed the other will develop it.
Can lost vision from wet AMD be restored?
Current treatments reduce further vision loss but rarely restore vision already lost to abnormal vessel growth and bleeding.
Does wet AMD mean dry AMD is ‘cured’?
No. Wet AMD is a progression, not a cure or change from one type to another. Management and monitoring must continue in both eyes.
Living with AMD: Managing Quality of Life
Maintaining quality of life with AMD requires both medical and practical approaches:
- Low vision aids: Magnifiers, special glasses, and improved lighting can help compensate.
- Rehabilitation: Vision rehabilitation programs offer techniques for maximizing remaining sight.
- Support networks: Counseling and support groups offer emotional and practical support.
When to Contact Your Eye Doctor
Contact your eye care provider if you notice:
- New or worsening vision problems
- Lines appearing wavy or distorted
- Rapid changes in visual clarity or colors
- Developing central blind spots
Conclusion
Dry AMD can progress to wet AMD, but not in every case. Understanding your risk factors and maintaining regular eye exams can protect your vision. Lifestyle modifications, effective at-home monitoring, and prompt access to new treatments offer the best chances to prevent severe vision loss. If you have any concerns about your vision, seek an eye care professional’s advice right away.
References
- https://www.crmd.net/wet-vs-dry-macular-degeneration-key-differences-and-treatment-approaches/
- https://www.healthline.com/health/wet-vs-dry-macular-degeneration
- https://www.macularsociety.org/about/media/news/2019/august/do-you-know-difference-between-wet-and-dry-amd/
- https://www.kcretina.com/blog/understanding-the-difference-between-dry-and-wet-age-related-macular-degeneration
- https://www.medicalnewstoday.com/articles/wet-vs-dry-macular-degeneration
- https://health.clevelandclinic.org/wet-vs-dry-macular-degeneration
- https://louisianaretina.com/what-is-the-difference-between-wet-and-dry-macular-degeneration/
- https://www.eyecenteroftexas.com/2021/01/wet-vs-dry-macular-degeneration/
- https://www.macular.org/about-macular-degeneration/what-is-macular-degeneration/types/dry-vs-wet-macular-degeneration
Read full bio of medha deb












