Dry Age-Related Macular Degeneration: Causes, Symptoms, and Care
Understand the causes, symptoms, diagnosis, and treatment options for dry age-related macular degeneration and learn how to protect your central vision.
Dry Age-Related Macular Degeneration: A Comprehensive Guide
As we age, changes in our vision are common, but some conditions can significantly affect our quality of life. Dry age-related macular degeneration (dry AMD) is one of the most prevalent eye diseases impacting central vision among older adults. Understanding its symptoms, causes, progression, and management is crucial for maintaining eye health and independence.
What Is Dry Age-Related Macular Degeneration?
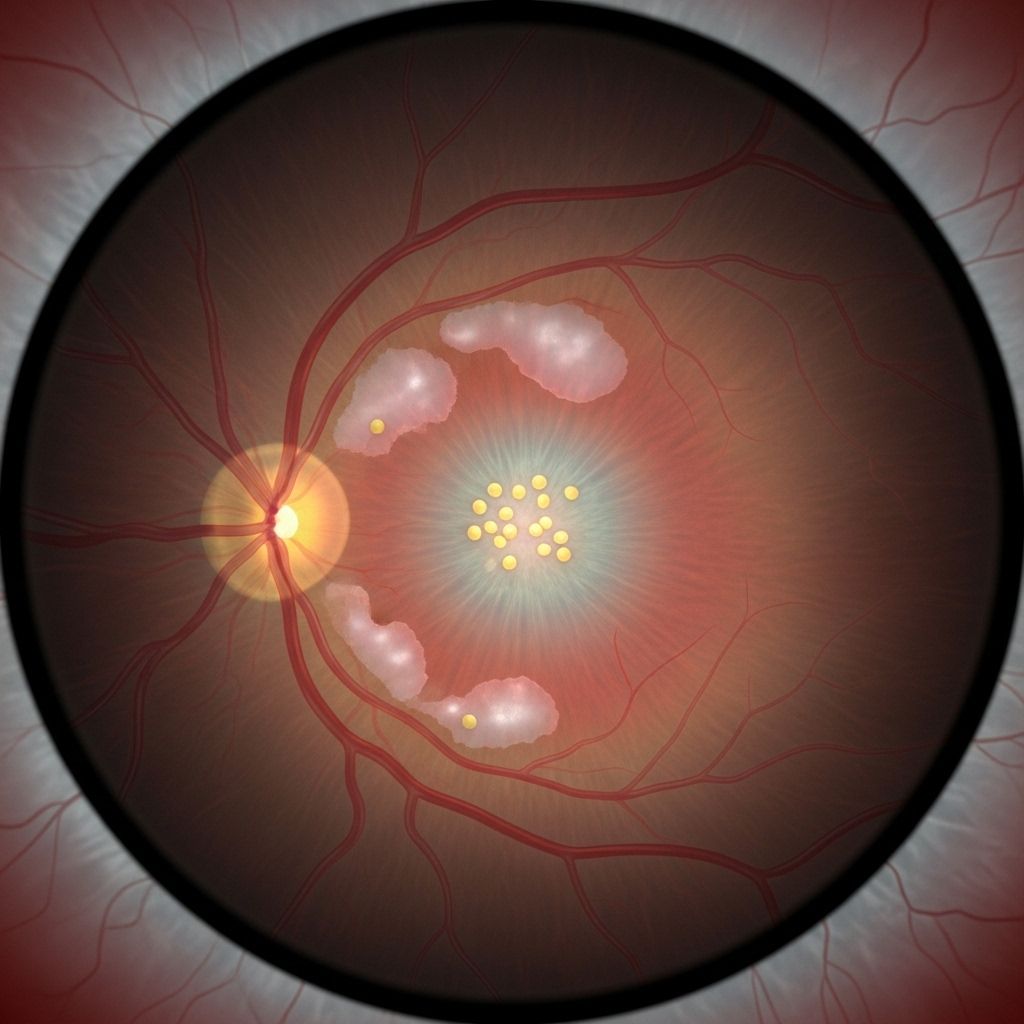
Dry age-related macular degeneration (dry AMD) is a chronic eye disorder where the macula—responsible for clear, central vision—gradually thins and deteriorates over time. This loss affects the photoreceptor and retinal pigmented epithelial cells in the macula, compromising the sharp, focused vision crucial for activities like reading, driving, and recognizing faces.
- The macula is a specialized region at the center of the retina responsible for detailed central vision.
- Dry AMD progresses over years and often develops in people aged 55 and older.
- It typically affects both eyes, though one may be more severely impacted.
Unlike some forms of vision loss, dry AMD does not cause complete blindness; however, losing your central vision can make daily activities much more challenging.
Symptoms of Dry Age-Related Macular Degeneration
The symptoms of dry AMD often develop slowly and can be subtle in the early stages. They may differ between individuals, but common symptoms include:
- Blurry or fuzzy central vision: Difficulty reading, seeing faces, or focusing on detailed tasks.
- Dark, blurry, or blank spots: Gaps or smudges in your central vision, sometimes described as dark or empty areas.
- Visual distortions: Straight lines, such as door frames or lampposts, may appear bent or wavy.
- Difficulty adapting to low light: Struggling with vision when moving from bright to dim areas or needing brighter light for reading.
- Fading colors: Colors may look less vibrant or washed out.
- Difficulty recognizing faces due to loss of central detail.
Some individuals initially have no noticeable symptoms, especially if only one eye is affected, as the other eye can compensate for vision loss. As the condition progresses, symptoms become more evident.
Stages of Dry Age-Related Macular Degeneration
Dry AMD progresses through three main stages, each impacting vision differently:
- Early stage: The macula begins to thicken and degrade, but visual symptoms are usually absent. Diagnosis often depends on regular eye exams revealing small drusen (yellow deposits) beneath the retina.
- Intermediate stage: You may start to notice mild vision changes, such as blurry areas in central vision or slightly faded colors. Drusen are larger, and minor retinal pigment changes may be detected during an exam.
- Late stage: Symptoms become more pronounced, with substantial central vision loss and significantly increased difficulty with detailed tasks. The atrophy (thinning and dying) of retinal cells is extensive.
What Causes Dry Age-Related Macular Degeneration?
Dry AMD is primarily associated with age-related changes in the eye. The exact cause is not completely understood, but the following mechanisms play key roles:
- Gradual breakdown and thinning of the macula’s light-sensitive cells.
- Accumulation of drusen between the retina and the underlying tissue, interfering with nutrient delivery and waste removal.
- Genetic predisposition, environmental factors, and lifestyle choices also influence risk.
Key Contributing Factors
- Age: The risk significantly increases after age 55.
- Genetics: A family history of AMD raises your likelihood of developing it.
- Race: White or Caucasian individuals are statistically more prone to AMD.
- Smoking: Tobacco use damages the blood vessels of the retina.
- Poor diet: Particularly low intake of antioxidants, vitamins, and minerals.
- Obesity and cardiovascular health: These conditions are linked to increased risk and faster progression.
Dry vs. Wet Macular Degeneration
| Dry AMD | Wet AMD |
|---|---|
| Most common type (85–90% of cases) | Less common (10–15% of cases) |
| Caused by thinning and degeneration of macular cells | Caused by abnormal blood vessel growth and leakage under retina |
| Progresses slowly, often over years | Often progresses quickly and causes rapid vision loss |
| Can potentially progress to wet AMD | Associated with more severe vision loss |
Dry AMD progresses gradually and is far more common, but has less risk of sudden vision loss than wet AMD. However, some people with dry AMD may develop wet AMD later, leading to more severe complications. Prompt diagnosis and monitoring are essential to detect any progression.
Who Is at Risk of Developing Dry Age-Related Macular Degeneration?
Several demographic and lifestyle factors can increase an individual’s risk for dry AMD:
- Advancing age (over 55 years)
- Family history or genetic predisposition
- Being Caucasian
- Smoking or use of tobacco products
- Poor dietary habits, especially low antioxidant intake
- Obesity and cardiovascular disease
- High blood pressure (hypertension)
- Long-term exposure to ultraviolet radiation
Although you cannot change your genetics or age, other risk factors such as diet, smoking, and UV protection can be modified to support eye health and slow disease progression.
How Is Dry Age-Related Macular Degeneration Diagnosed?
Early detection is critical for managing dry AMD. Diagnosis typically involves a visit to an eye care professional (optometrist or ophthalmologist), who may use several tools and tests:
- Dilated eye exam: Eye drops enlarge the pupil, allowing detailed inspection of the retina and the presence of drusen or pigment changes.
- Visual acuity test: Measures your ability to see fine detail at various distances.
- Amsler grid: A simple grid test to check for visual distortions or blank spots in central vision.
- Optical coherence tomography (OCT): Imaging technology creates detailed cross-sectional images of the retina, highlighting areas of thinning, drusen, or atrophy.
- Fundus photography: High-resolution pictures of the retina to document macular changes over time.
Because early-stage dry AMD often has no noticeable symptoms, routine eye exams are important after age 50, especially for those with increased risk.
Treatment Options for Dry Age-Related Macular Degeneration
Currently, there is no cure or treatment to stop the cell loss characteristic of dry AMD. However, several strategies may help slow its progression or improve remaining vision:
- Low-vision aids: Devices such as magnifying glasses, reading lamps, and electronic readers help compensate for central vision loss.
- Vision rehabilitation: Specialized therapy teaches new methods for reading, daily tasks, and coping with vision changes.
Role of Nutritional Supplements
Evidence suggests that certain dietary supplements may slow progression in those with intermediate or late-stage dry AMD. The AREDS2 (Age-Related Eye Disease Study 2) formulation is widely recommended and includes:
- Vitamin C (ascorbic acid)
- Vitamin E
- Lutein and zeaxanthin
- Zinc oxide
- Copper oxide
Consult your ophthalmologist before starting any supplement, especially if you have other health conditions.
Prevention: How to Lower Your Risk
While age and genetics are unchangeable, you can adopt lifestyle and dietary habits to help preserve your vision:
- Quit smoking: Stopping tobacco use is one of the most impactful steps you can take.
- Eat a balanced diet: Emphasize green leafy vegetables, colorful fruits and vegetables, fish (omega-3 sources), and healthy fats.
- Exercise regularly: Physical activity helps maintain heart and blood vessel health, supporting good eye circulation.
- Manage chronic conditions: Keep blood pressure, cholesterol, and diabetes under control.
- Protect eyes from UV light: Wear sunglasses that block both UVA and UVB radiation when outdoors.
- Regular eye exams: Early detection allows for better management before significant vision loss occurs.
Outlook for People With Dry Age-Related Macular Degeneration
Dry AMD typically progresses slowly, allowing many people to adapt their lifestyles and retain independence for years after diagnosis. Most people do not become completely blind, as side (“peripheral”) vision remains intact. However, central vision loss can substantially affect reading, recognizing faces, and performing tasks relying on detailed vision.
Vision rehabilitation, assistive technology, and supportive care remain crucial for maintaining quality of life. Ongoing research is focused on new medications, cell therapy, and vision-improving technologies for future treatment options.
Frequently Asked Questions (FAQs)
Can dry AMD be cured?
No, dry age-related macular degeneration cannot currently be cured. However, lifestyle adjustments and medical management may slow its progression and maximize remaining vision.
Is dry AMD the same as wet AMD?
No. Dry AMD is caused by gradual thinning of the macula, whereas wet AMD involves abnormal blood vessel growth under the retina. Dry AMD is more common and progresses slowly, but it can develop into wet AMD in some individuals.
Does dry AMD cause total blindness?
Dry AMD does not cause complete blindness because it primarily affects central vision. Peripheral vision usually remains unchanged, but significant central vision loss can make everyday activities challenging.
Who is most at risk for dry AMD?
People over 55, especially those who are white, have a family history of macular degeneration, smoke, or have poor diets are at highest risk of developing dry AMD.
Can a healthy lifestyle really help prevent or slow dry AMD?
Yes. Quitting smoking, eating a diet rich in leafy greens and colored vegetables, protecting your eyes from UV rays, and managing health conditions can help lower the risk and may slow progression.
Summary
Dry age-related macular degeneration is a prevalent and progressive condition affecting the central vision of older adults. While it cannot be cured, timely diagnosis, lifestyle changes, and vision support can improve quality of life and help you continue to enjoy daily activities. If you notice any changes in your vision—especially blurriness, blank spots, or difficulty seeing details—consult an eye care professional for assessment and support.
References
- https://www.healthline.com/health/eye-health/dry-age-related-macular-degeneration
- https://www.macularsociety.org/macular-disease/macular-conditions/dry-age-related-macular-degeneration/
- https://www.mayoclinic.org/diseases-conditions/dry-macular-degeneration/symptoms-causes/syc-20350375
- https://www.healthline.com/health/macular-degeneration
- https://www.ncbi.nlm.nih.gov/books/NBK500482/
- https://www.brightfocus.org/resource/update-on-dry-age-related-macular-degeneration/
- https://medlineplus.gov/maculardegeneration.html
- https://www.eyesiteonwellness.com/stateofwi/en
Read full bio of Sneha Tete












