Drug-Eluting Stents: Function, Benefits, Risks, and Prevention
Comprehensive guide on how drug-eluting stents work, their benefits over bare-metal stents, potential risks, and post-procedure care.
Drug-Eluting Stents: How Do They Work?
Drug-eluting stents (DES) have transformed the treatment of coronary artery disease (CAD) by providing a minimally invasive option to open narrowed arteries, prevent future blockages, and promote lasting heart health. This article provides an in-depth look at how drug-eluting stents work, their advantages over other treatment methods, the procedure, potential risks, and guidance for maintaining your long-term heart health following stent implantation.
Understanding Drug-Eluting Stents and Coronary Artery Disease
Coronary artery disease (CAD) is a condition where the coronary arteries become narrowed or blocked by plaque buildup (atherosclerosis).
- This blockage restricts blood flow, depriving the heart muscle of oxygen-rich blood.
- Prolonged or severe reduction in blood flow increases the risk of heart muscle damage and heart attack.
- Symptoms can include chest pain (angina), shortness of breath, or even heart attack.
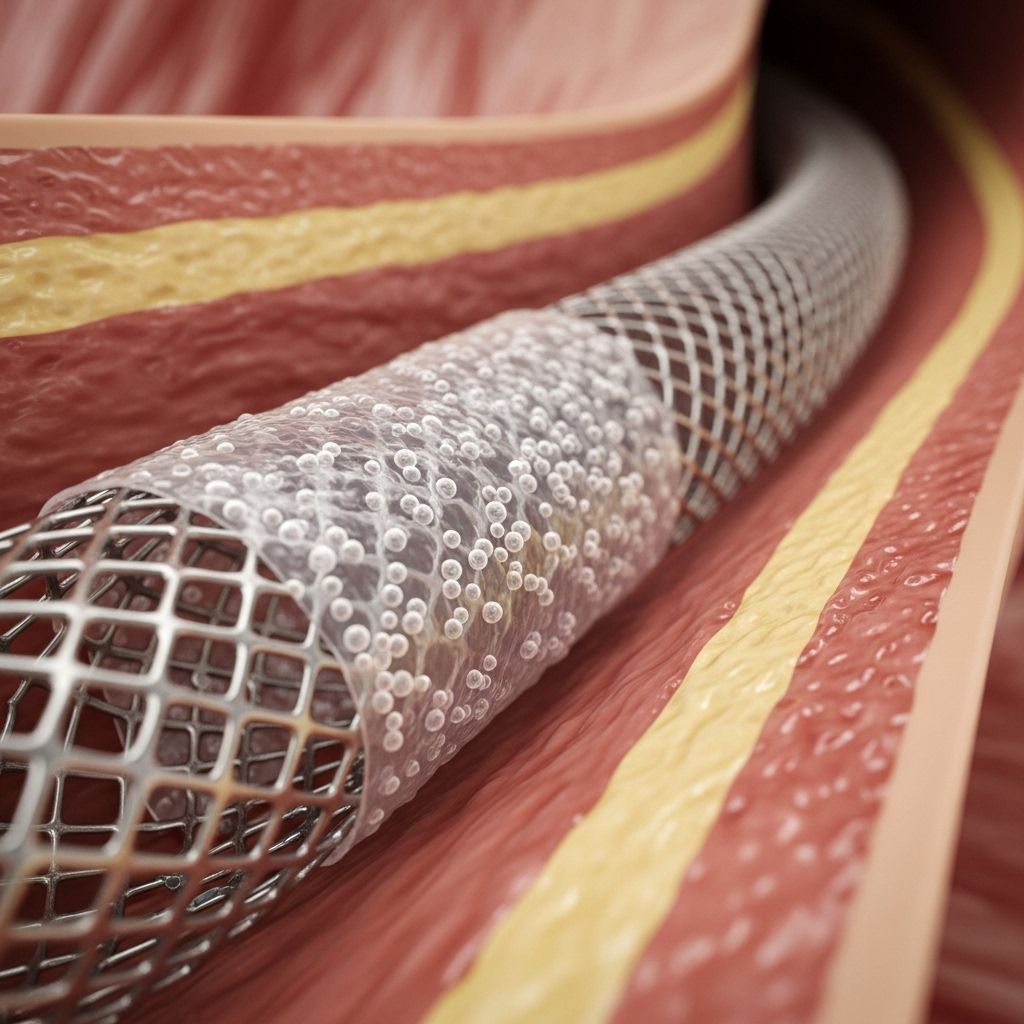
Stents are small, mesh-like metal tubes inserted into narrowed arteries during an angioplasty procedure to keep them open and support improved blood flow.
What Is a Drug-Eluting Stent?
A drug-eluting stent (DES) is a specialized stent coated with a medication that gradually releases (elutes) into the surrounding artery wall over a period of months after placement.
- The drug is typically an anti-proliferative agent that prevents restenosis—the re-narrowing or blockage of the artery due to excess tissue growth.
- This controlled drug release significantly lowers the risk of tissue regrowth and future blockages compared to “bare-metal” stents or balloon angioplasty alone.
DES technology is now the standard of care for most patients requiring stent placement for CAD.
Components of a Drug-Eluting Stent
- Metal mesh frame: Typically made of stainless steel or other advanced alloys to maintain arterial support.
- Polymer coating: Holds and gradually releases the drug.
- Pharmacologic agent: Drug(s) embedded in the polymer that prevents cell overgrowth and reduces restenosis risk.
Drug-Eluting Stents vs. Bare-Metal Stents
| Feature | Drug-Eluting Stent (DES) | Bare-Metal Stent (BMS) |
|---|---|---|
| Drug Coating | Yes, slow-release to prevent restenosis | No |
| Risk of Restenosis | <10% | ~30% |
| Need for Repeat Procedure | Lower | Higher |
| Antiplatelet Therapy | Longer duration usually needed | Shorter duration may suffice |
| Long-term Safety | Established, with appropriate medication adherence | Reliable, but higher chance of restenosis |
How Is a Drug-Eluting Stent Implanted?
The placement of a drug-eluting stent is performed during an outpatient procedure called coronary angioplasty or percutaneous coronary intervention (PCI).
Step-By-Step Procedure
- Access: A small incision is made, typically in the groin or wrist.
- Catheterization: A thin, flexible tube (catheter) is threaded through a blood vessel to the blocked section of the coronary artery.
- Balloon inflation: A balloon-tipped catheter is inflated to widen the narrowed artery.
- Stent placement: The drug-eluting stent, mounted on the balloon, is positioned at the site of narrowing. The balloon is then inflated, expanding the stent into place.
- Stent deployment: The balloon is deflated and removed, leaving the stent anchored in the artery, where it supports vessel walls and slowly releases medication.
- End of procedure: The incision site is closed, and most patients remain in the hospital for observation, usually overnight.
Benefits of Drug-Eluting Stents
- Greatly Reduced Restenosis: DES lower the risk of restenosis to less than 10%, compared to 30% with bare-metal stents and 40% with balloon angioplasty alone.
- Restores and Maintains Blood Flow: By keeping the artery open and inhibiting tissue overgrowth, DES restore oxygen-rich blood supply to heart muscle, reducing symptoms such as chest pain.
- Decreases the Need for Repeat Procedures: The lower risk of artery re-narrowing reduces the chance of requiring another angioplasty or stent.
- Minimally Invasive Option: Compared to open-heart surgery or coronary artery bypass grafting (CABG), DES implantation is less invasive, involves a smaller incision, and requires shorter hospital stays.
- Faster Recovery: Many patients resume normal activity within days to weeks, whereas bypass surgery recovery can take several weeks to months.
- Safe and Effective: Extensive research and real-world data confirm that modern DES are safe and effective for the majority of patients when prescribed antiplatelet (anti-clotting) therapy is followed.
Who Might Benefit from a Drug-Eluting Stent?
DES are typically recommended for:
- Individuals with significant coronary artery narrowing due to atherosclerosis
- People experiencing angina (chest pain) that limits activity or quality of life
- Those at high risk for tissue regrowth (restenosis) following angioplasty
- Patients for whom major cardiac surgery (bypass) may not be appropriate
Ultimately, the choice of stent type and specific approach is based on the individual’s anatomy, overall health, and risk factors, and is determined by the treating cardiologist.
Risks and Potential Complications of Drug-Eluting Stents
As with any medical procedure, drug-eluting stents carry some risks, though advances in technology and technique have substantially reduced complication rates:
- Blood clots (Stent thrombosis): Can occur in rare cases, especially if antiplatelet therapy is not strictly followed. These clots can cause a heart attack or be life-threatening.
- Bleeding: Related to the access site or from long-term antiplatelet medication use.
- Infection: Risk is low but possible any time the vascular system is entered.
- Allergic reaction: Rare reactions to stent materials or drugs may occur.
- Artery damage: The vessel may become injured during the procedure, though such risks are minimized with modern techniques.
How to Minimize Risks
- Adhere to prescribed antiplatelet therapy: Medications such as aspirin and a P2Y12 inhibitor (e.g., clopidogrel, ticagrelor, or prasugrel) reduce clotting risk significantly and are usually required for several months to a year after DES placement.
- Communicate with your care team: Inform all healthcare providers about your stent, especially before surgical or dental procedures.
- Attend regular follow-up visits: Schedule and attend check-ups to ensure your stent remains open and to monitor for side effects.
- Report symptoms promptly: If you experience chest pain, shortness of breath, or unusual bleeding, contact your doctor immediately.
Long-Term Care and Lifestyle After Drug-Eluting Stent Placement
Caring for your heart after stent implantation is crucial for promoting stent success and maintaining long-term cardiovascular health.
- Stay on prescribed medications: Even after the minimum period, you may need to stay on aspirin or other heart-protective medications.
- Adopt a heart-healthy lifestyle:
- Eat a balanced, low-sodium, low-saturated fat diet rich in fruits, vegetables, and whole grains
- Engage in regular physical activity as advised by your physician
- Maintain a healthy weight
- Quit smoking and avoid tobacco products
- Limit alcohol intake
- Control blood pressure, cholesterol, and diabetes: Managing these risk factors is essential for preventing new blockages.
Prevention and Monitoring of Restenosis
While drug-eluting stents make restenosis much less likely, ongoing vigilance is important:
- Routine testing: Follow-up appointments may include stress tests, echocardiograms, or angiography to check arterial flow if needed.
- Symptom recognition: Recurrence of chest pain or other symptoms could signal a new or recurring blockage.
- Medication adherence: Skipping medications, especially antiplatelet therapy, is a major risk for stent thrombosis.
Comparing Treatment Options: Angioplasty, Stenting, and Bypass Surgery
| Treatment | Invasiveness | Recovery Time | Restenosis Risk | Suitability |
|---|---|---|---|---|
| Angioplasty Alone | Minimally invasive | 1-2 days | 40% | Selected simple blockages |
| Bare-Metal Stent (BMS) | Minimally invasive | 1-2 days | ~30% | May be used where longer antiplatelet therapy isn’t desired |
| Drug-Eluting Stent (DES) | Minimally invasive | 1-2 days | <10% | Most modern cases of CAD |
| Bypass (CABG) Surgery | Highly invasive; open-heart | Several weeks | Very low at graft site | Multi-vessel or complex disease, failed stent cases |
Frequently Asked Questions (FAQs) About Drug-Eluting Stents
Q: What is the main advantage of a drug-eluting stent over a bare-metal stent?
A: Drug-eluting stents have a significantly lower risk of restenosis because the drug coating inhibits tissue overgrowth inside the artery, reducing the chances of recurrent narrowing and the need for repeat procedures.
Q: How long do drug-eluting stents last?
A: The stent itself is designed to be permanent. The drug is released over a few months, after which the stent remains to support the artery. Lifelong medication and heart-healthy habits are still necessary to support overall cardiovascular health.
Q: Can I stop my antiplatelet medications once my stent is in place?
A: No. Stopping antiplatelet therapy too early increases the risk of life-threatening stent thrombosis. Always follow your cardiologist’s guidance regarding medication duration.
Q: Are there people who should not get a drug-eluting stent?
A: Drug-eluting stents may not be suitable for individuals unable to take long-term antiplatelet medications or those with certain allergies to stent materials. Your care team will help determine the safest option.
Q: What symptoms should prompt me to contact my doctor after stent placement?
A: New or worsening chest pain, shortness of breath, or unexpected bleeding should be promptly reported to your healthcare provider.
When to Call Your Doctor
After receiving a drug-eluting stent, contact your healthcare provider if you experience any of the following:
- Fever, chills, or signs of infection at the incision site
- New, recurring, or severe chest pain
- Unusual bleeding, headache, or bruising
- Shortness of breath, fainting, or cough that won’t go away
Regular medical follow-up ensures early detection and management of any complications.
Summary
Drug-eluting stents offer a life-saving and minimally invasive approach to restoring blood flow in coronary artery disease, dramatically reducing the risk of artery renarrowing and improving quality of life for heart patients. With modern advances, these stents are a cornerstone of contemporary cardiology, but long-term success depends on medication adherence, healthy habits, and ongoing follow-up care.
References
- https://www.youtube.com/watch?v=Oi729xpRA48
- https://www.mayoclinic.org/diseases-conditions/coronary-artery-disease/in-depth/drug-eluting-stents/art-20044911
- https://www.healthline.com/health/heart-disease/drug-eluting-stent
- https://www.merillife.com/blogs/drug-eluting-stent-what-is-it-and-how-it-is-implanted-meril-life
- https://www.healthline.com/health/heart-disease/stent
- https://pubmed.ncbi.nlm.nih.gov/17315599/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3417932/
- https://www.ecrjournal.com/articles/newest-generation-drug-eluting-stents-and-beyond?language_content_entity=en
Read full bio of Sneha Tete












