Distal Radius Fracture (Wrist Fracture): Symptoms, Diagnosis, and Treatments
Comprehensive guide to understanding, diagnosing, and treating distal radius (wrist) fractures, including symptoms, recovery, and FAQs.
A distal radius fracture is one of the most common types of bone injuries, frequently resulting from falls or trauma to the wrist. This guide covers the causes, symptoms, diagnostic procedures, treatment options, and answers frequently asked questions to help patients and caregivers understand this condition and its management.
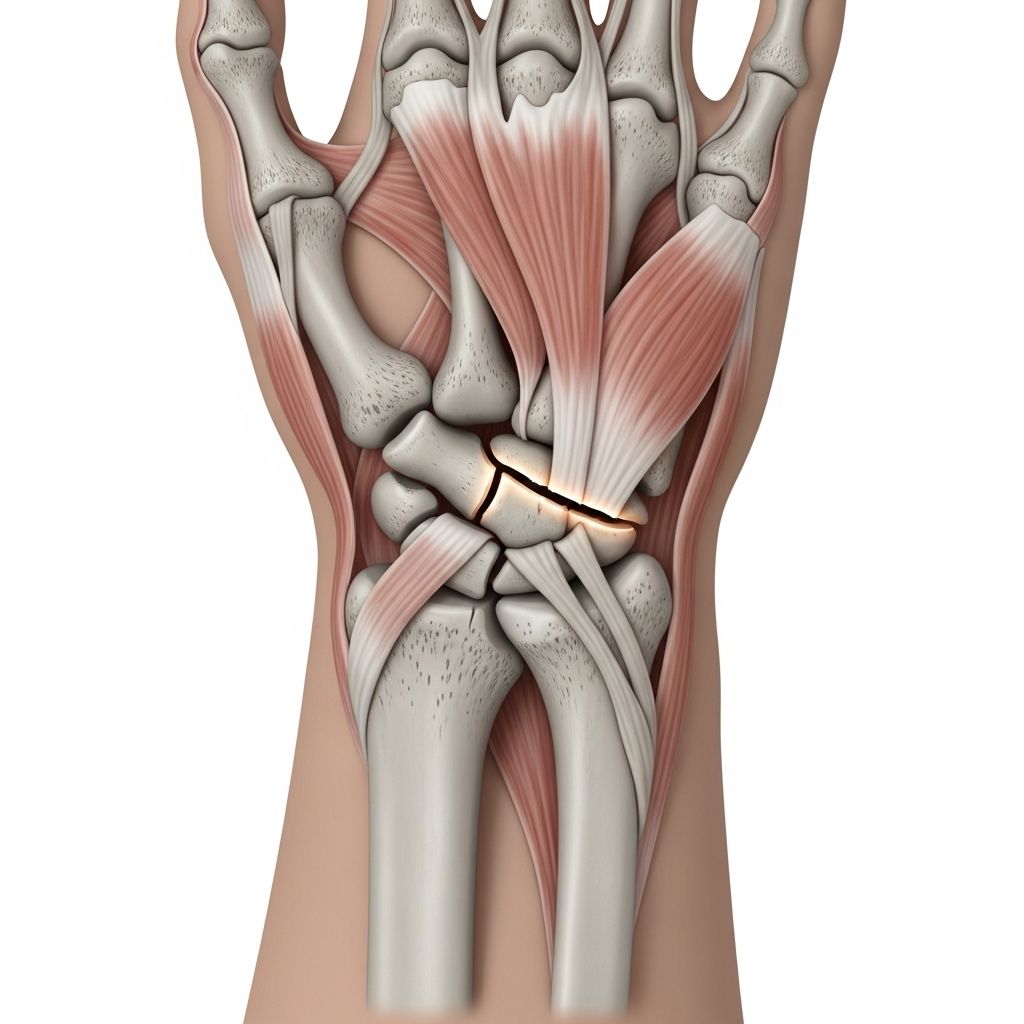
What is a Distal Radius Fracture?
The distal radius refers to the end portion of the radius bone near the wrist. A fracture here—commonly known as a wrist fracture—occurs when part or all of this bone breaks, often following a fall onto an outstretched hand or other trauma. This injury can affect people of all ages but is especially prevalent among children, active adults, and older adults with osteoporosis.
Causes of Distal Radius Fractures
- Fall on an Outstretched Hand (FOOSH): The most common cause, leading to high force being transmitted to the wrist.
- Sports Injuries: Contact sports or activities with a high risk of falling.
- Motor Vehicle Accidents: Direct trauma from collisions.
- Work-related Injuries: Slips, trips, or being struck by an object at work.
- Age-related Bone Loss: Osteoporosis increases fracture risk in older adults.
Symptoms of Distal Radius Fracture
- Wrist Pain: Usually immediately after the injury, may be severe.
- Swelling: Around the wrist and forearm.
- Deformity: Noticeable change in wrist shape if the fracture is displaced.
- Bruising: Black and blue discoloration is common around the injury site.
- Loss of Function: Difficulty moving or using the wrist and hand.
- Numbness or Tingling: Possible if nerves are affected.
- Decreased Mobility and Strength: Limited range of motion and weakness in grip.
If you experience intense pain, deformity, numbness, or loss of color in fingers after a wrist injury, seek emergency care immediately.
Diagnosis of Distal Radius Fractures
- Medical History: Typically involves trauma, such as a fall or accident.
- Physical Examination: The physician checks for deformity, swelling, tenderness, and neurovascular compromise.
- X-ray Imaging: Primary diagnostic tool to assess location, type, and severity of the fracture. Most distal radius fractures are visible on plain radiographs, which help classify the injury and guide treatment decisions.
Advanced imaging (CT or MRI) may be used for complex fractures or to plan for surgery.
Types and Classification of Distal Radius Fractures
Distal radius fractures are classified according to their pattern, location, and degree of displacement. Several key factors help determine management choices:
- Degree of Fragmentation: Complexity of the fracture.
- Displacement: Whether bone fragments have shifted out of their normal alignment.
- Integrity of Wrist Columns: Assessment includes nearby bones, such as the ulna.
- Patient Age: Indicative of bone quality and likely healing capacity.
- Joint Surface Involvement: Whether the break extends into the wrist joint.
Emergency Management
Immediate care steps for a suspected distal radius fracture include:
- Protecting the wrist with a splint.
- Applying ice to reduce swelling.
- Elevating the arm above heart level.
- Pain management, using oral or intravenous medication as needed.
- Seeking prompt orthopedic evaluation for severe pain, deformity, or neurovascular symptoms.
Special Considerations
- Open Fractures: If the bone breaks through the skin, urgent orthopedic and often vascular surgical care is needed. These injuries require cleaning (“washout”) and antibiotic prophylaxis.
- Neurovascular Compromise: If blood flow (pulses) or nerve function is impaired, emergency surgical evaluation is warranted.
Treatment Options for Distal Radius Fracture
Treatment of distal radius fractures is determined by the fracture type, patient’s age and lifestyle, overall health, and degree of displacement. The main goals are restoring bone alignment, joint function, and stability while minimizing complications.
- Non-Surgical Treatment (Casting/Splinting):
- Stable, minimally displaced fractures are often treated with a cast or splint for about six weeks.
- Closed reduction can be performed under anesthesia to realign bones before casting.
- Subsequent follow-up includes repeat radiographs to confirm maintenance of alignment.
- Light use of the hand may begin once initial healing occurs, usually by six weeks.
- Surgical Treatment:
- Unstable or displaced fractures, especially in younger or highly active patients, may need surgical intervention for optimal outcomes.
- The surgeon may perform open reduction and internal fixation using plates, screws, or rods, or minimally invasive techniques such as percutaneous pinning.
- Surgery aims to restore alignment, smooth joint surfaces, and stability to enable functional recovery.
- Emergent surgery is required for open fractures, severe neurovascular injury, or failed non-surgical management.
Table: Comparison of Non-Surgical vs. Surgical Treatment
| Aspect | Non-Surgical (Cast/Splint) | Surgical (ORIF, Pins, Plates) |
|---|---|---|
| Indications | Stable, non-displaced fractures; patient unable to undergo surgery | Unstable, displaced, intra-articular fractures; failed non-op treatment |
| Procedure | Closed reduction (if needed), immobilization in cast/splint | Open reduction (fracture exposure), fixation (plates, screws, pins) |
| Duration | Cast/splint worn for 6 weeks then rehabilitation | Surgical wound healing (2-3 weeks), possible cast, then rehabilitation |
| Recovery | Light use after 6 weeks; full recovery in months | Often earlier motion; full recovery may be quicker |
| Advantages | Avoids surgical risks; cost-effective | Better alignment; lower chance of long-term deformity |
| Disadvantages | Some risk of malunion; immobilization stiffness | Surgical risks (infection, hardware issues, nerve injury) |
Pain Management & Post-Treatment Care
- Pain Control: Oral analgesics, intravenous narcotics, and nerve blocks may be used; tailored to severity.
- Follow-up: Regular assessments and radiographs to monitor bone healing and alignment.
- Rehabilitation: Physical therapy to restore range of motion, strength, and function, starting soon after immobilization ends.
Potential Complications
- Malunion: Bones heal in poor alignment, reducing function and causing deformity.
- Nerve or Blood Vessel Injury: Risk in complex/fractured or displaced injuries.
- Compartment Syndrome: Rare, severe swelling restricting blood supply, requires emergency surgery.
- Post-Traumatic Arthritis: If joint surface involvement was present.
- Stiffness: Especially with prolonged immobilization or incomplete rehabilitation.
- Nonunion: Fracture fails to heal; may require further surgery.
Recovery Timeline
- Initial Healing: Most distal radius fractures are stabilized within six weeks, permitting initiation of light activities.
- Full Recovery: May take several months for complete bone and soft tissue healing and functional return.
- Physical Therapy: Plays a vital role in regaining motion and strength for regular daily use.
Frequently Asked Questions (FAQs)
Q: What should I do if I think I have a wrist fracture?
A: Protect the wrist using a splint, apply ice, and keep the arm elevated. Seek urgent medical evaluation, especially if there’s severe pain, wrist deformity, numbness, or color changes in the fingers.
Q: How is a distal radius fracture diagnosed?
A: Diagnosis is based on medical history, physical exam, and confirmation with x-rays. Advanced imaging may be required for complex cases.
Q: Do all distal radius fractures require surgery?
A: No. Many stable or minimally displaced fractures heal well with casting alone. Surgery is reserved for unstable, misaligned, or joint-involved fractures.
Q: What is recovery like after a distal radius fracture?
A: Initial cast/splint use lasts about six weeks. Physical therapy starts after immobilization ends. Full recovery can take several months, and some residual stiffness or weakness is possible.
Q: Can I prevent distal radius fractures?
A: Practicing fall prevention (especially in the elderly), using wrist guards during high-risk activities, and maintaining healthy bones with adequate calcium and vitamin D can reduce risk.
Additional Common Questions
Q: What happens if I delay treatment?
A: Delaying treatment increases the risk of poor bone alignment, longer healing times, complications such as chronic pain, stiffness, or loss of function.
Q: Is physical therapy needed after treatment?
A: Yes. Physical therapy is essential for regaining wrist strength and flexibility after immobilization or surgery.
Q: How long does it take to return to normal activities?
A: Simple, non-displaced fractures can allow return to normal light activities after six weeks, but full recovery may take up to six months or longer depending on injury severity and patient factors.
Key Takeaways
- Distal radius fractures are common and often result from falls or direct trauma.
- Early diagnosis and proper management (whether non-surgical or surgical) are crucial for good outcomes.
- Physical therapy and rehabilitation play a central role in full recovery and restoring hand and wrist function.
- Prompt care helps minimize complications and long-term disability.
This comprehensive overview aims to provide patients, families, and clinicians with an evidence-based understanding of distal radius fractures, supporting informed conversations about individual care needs.
References
- https://www.hss.edu/health-library/conditions-and-treatments/distal-radius-fractures-of-the-wrist
- https://orthopedicreviews.openmedicalpublishing.org/article/125163-distal-radius-fracture-with-dorsal-angulation
- https://www.uconnhealth.org/orthopedics-sports-medicine/services-specialties/distal-radius-fracture
- https://www.ncbi.nlm.nih.gov/books/NBK536916/
- https://thejacksonclinics.com/arm-yourself-after-a-distal-radius-fracture/
- https://orthoinfo.aaos.org/en/diseases–conditions/distal-radius-fractures-broken-wrist/
- https://my.clevelandclinic.org/health/diseases/21860-colles-fracture
- https://www.cfaortho.com/distal-radius-fracture-broken-wrist-distalradiusfracture
- https://www.uhsussex.nhs.uk/wp-content/uploads/2022/09/Distal-radius-fractures-virtual-hand-fracture-clinic.pdf
Read full bio of medha deb












