Disorders of the Pituitary Gland: Causes, Types, Symptoms & Treatments
Explore common and rare pituitary gland disorders, their causes, symptoms, and current treatment options for improved hormonal health.
Disorders of the Pituitary Gland
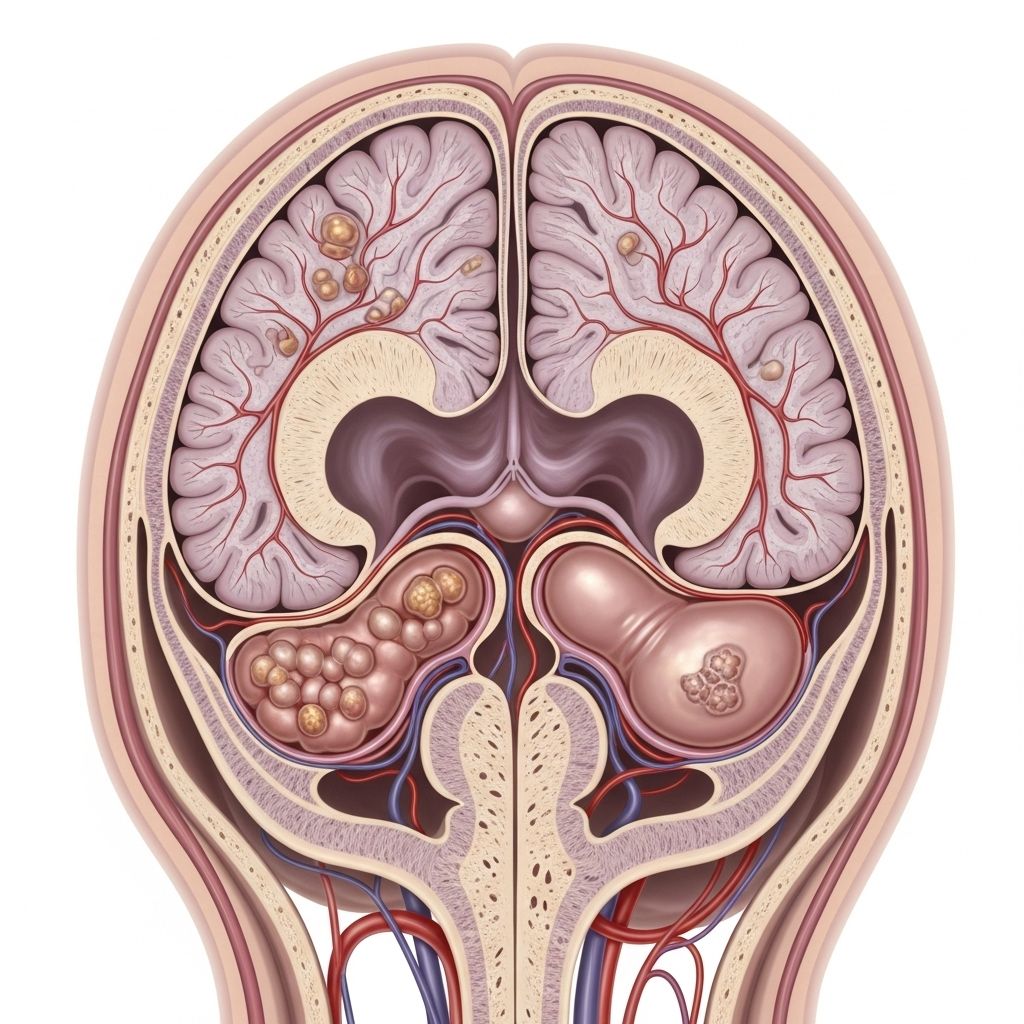
The pituitary gland is a small, pea-sized organ located at the base of the brain, often referred to as the “master gland” due to its key role in regulating other endocrine glands. Despite its size, the pituitary is critical for managing a wide array of bodily functions, including growth, metabolism, reproductive processes, and stress response. Disruptions to its function — whether through tumors, trauma, genetics, or disease — can result in significant, often complex health problems known as pituitary gland disorders.
What Is the Pituitary Gland?
The pituitary gland produces several hormones that control vital processes:
- Growth hormone (GH): Regulates growth and body composition.
- Adrenocorticotropic hormone (ACTH): Stimulates adrenal glands to produce cortisol.
- Thyroid-stimulating hormone (TSH): Controls thyroid gland hormone production.
- Luteinizing hormone (LH) & Follicle-stimulating hormone (FSH): Regulate sexual development, function, and reproduction.
- Prolactin: Influences milk production in the breasts.
- Antidiuretic hormone (ADH, vasopressin): Manages body water balance through kidney regulation.
- Oxytocin: Stimulates uterine contractions and milk ejection.
The pituitary has two main lobes, each responsible for different hormones — the anterior lobe (front) and posterior lobe (back). Disorders may involve either or both parts.
What Are Pituitary Gland Disorders?
Pituitary gland disorders arise when the gland produces either too much (hyper-) or too little (hypo-) of one or more hormones, or develops tumors that disrupt normal function.
- Hyperpituitarism: Excessive hormone production.
- Hypopituitarism: Decreased hormone production, potentially affecting one or multiple hormones.
- Pituitary tumors (adenomas): Noncancerous growths in the gland causing pressure effects and/or hormone imbalances.
Types of Pituitary Gland Disorders
Pituitary gland disorders can be categorized primarily by the specific hormone(s) involved or the presence of tumor growth.
Pituitary Tumors (Adenomas)
- Nonfunctioning adenomas: These benign tumors do not secrete excess hormones but can grow large and compress nearby tissues, leading to headaches, visual changes, or reduced hormone production (hypopituitarism).
- Functioning adenomas: These tumors actively secrete excess hormones and are classified by the type of hormone involved:
- Prolactinoma: Secretes excess prolactin.
- Somatotroph adenoma: Produces excess growth hormone (leads to acromegaly in adults).
- Corticotroph adenoma: Produces excess ACTH (leads to Cushing’s disease).
- Thyrotroph adenoma: Secretes excess TSH (rare).
Based on size, adenomas are classified as:
- Microadenomas: Less than 1 cm in diameter.
- Macroadenomas: 1 cm or larger; more likely to cause symptoms by pressing on nearby structures.
Hormonal Imbalance Disorders
- Hypopituitarism: Partial or complete loss of pituitary hormone production. May result from tumor compression, surgery, trauma, radiation, infection, or autoimmune processes.
- Hyperpituitarism: Excessive hormone production, usually due to a functioning pituitary tumor.
Specific hormone disorders include:
- Diabetes insipidus: Caused by deficiency of ADH (antidiuretic hormone/vasopressin), leading to excessive urination and thirst.
- Acromegaly: Caused by excess growth hormone in adults, resulting in enlargement of hands, feet, and facial bones.
- Cushing’s disease: Caused by excess ACTH, leading to high levels of cortisol and characteristic symptoms such as weight gain, round face (“moon facies”), and skin changes.
- Hyperprolactinemia: Excessive production of prolactin, which can cause menstrual disturbances, infertility, and inappropriate breast milk production (galactorrhea).
- Central hypothyroidism: Deficient TSH leading to low thyroid hormone production.
- Central adrenal insufficiency: Deficient ACTH causing low cortisol levels.
Symptoms of Pituitary Gland Disorders
Symptoms vary widely depending on the specific disorder and hormones affected.
| Hormone/Disorder | Excess (Symptoms) | Deficiency (Symptoms) |
|---|---|---|
| Growth Hormone (GH) | Acromegaly: enlarged hands, feet, jaw; joint pain; oily skin | Fatigue, decreased muscle mass, lack of vigor, increased body fat, social withdrawal |
| Prolactin | Galactorrhea, sexual dysfunction, menstrual irregularities, infertility | Usually no significant symptoms |
| ACTH/Cortisol | Cushing’s disease: weight gain (central), round face, purple stretch marks, high blood pressure, diabetes, muscle weakness | Adrenal insufficiency: fatigue, low blood pressure, weight loss, nausea, dizziness |
| TSH/Thyroid | Hyperthyroidism: tremors, palpitations, weight loss, anxiety | Hypothyroidism: fatigue, weight gain, cold intolerance, constipation, dry skin |
| ADH (Vasopressin) | Syndrome of inappropriate antidiuretic hormone (SIADH): water retention, low sodium | Diabetes insipidus: excessive urination, intense thirst, dehydration |
| LH/FSH (Gonadotropins) | Rare; precocious puberty | Irregular menstruation, infertility, low libido, erectile dysfunction, hot flashes |
Causes of Pituitary Gland Disorders
There are multiple potential causes of pituitary dysfunction:
- Tumors: Most commonly noncancerous (benign) adenomas, but rarely may be malignant.
- Genetic factors: Some rare inherited conditions increase risk (e.g., MEN1, familial isolated pituitary adenoma).
- Trauma or injury: Head injuries or surgery may disturb gland function.
- Infections: Meningitis, encephalitis, or other infections affecting the brain.
- Autoimmune disorders: The immune system mistakenly attacks the pituitary gland.
- Radiation therapy: Prior radiation to the brain, often for cancer treatment, can harm the gland.
Who Is at Risk for Pituitary Gland Disorders?
- Anyone can develop pituitary gland conditions regardless of age or gender.
- Increased risk if you have:
- A family history of pituitary disease
- History of head injury or trauma
- Certain genetic conditions
- Previous brain radiation therapy
- Women are more likely to develop some specific disorders, such as prolactinomas.
Diagnosing Pituitary Gland Disorders
Diagnosis involves several steps:
- History and physical exam: Review of symptoms, family and medical history, and a complete physical.
- Blood and urine tests: To measure hormone levels (such as ACTH, GH, prolactin, cortisol, TSH, thyroid hormones, LH, FSH, ADH).
- Stimulation or suppression tests: For certain hormones, evaluating how the body responds to stimulation or suppression agents.
- Imaging studies: Magnetic resonance imaging (MRI) of the brain is used to visualize the pituitary gland and detect tumors or anatomical abnormalities.
- Visual field testing: To assess for tumor-related pressure on the optic nerves.
Treatment of Pituitary Gland Disorders
Treatment strategies depend on the specific disorder, underlying cause, and the patient’s general health. Main options include:
- Medication: Used to correct hormone imbalances (for example, dopamine agonists for prolactinomas) or replace deficient hormones (e.g., synthetic thyroid hormone, corticosteroids).
- Surgery: Minimally invasive pituitary surgery (typically transsphenoidal surgery — through the nose and sphenoid sinus) is the main treatment for many pituitary tumors, especially those causing symptoms or excess hormone production.
- Radiation therapy: Reserved for tumors that cannot be completely removed surgically or recur after initial treatment. Radiation is used less frequently but may be necessary for aggressive or residual tumors.
- Ongoing monitoring: Many pituitary conditions require lifelong follow-up and regular hormone testing to ensure effective management and to monitor for recurrence.
Individualized care is key, often provided by a multidisciplinary team including endocrinologists, neurosurgeons, ophthalmologists, and, as needed, other specialists.
Complications and Long-Term Effects
- Pituitary disorders can lead to chronic hormonal deficiencies, requiring lifelong hormone replacement.
- Some tumors may recur after treatment, necessitating ongoing monitoring.
- Untreated hormonal imbalances can cause serious complications, including infertility, vision loss, cardiovascular disease, osteoporosis, and impaired growth or development.
- Psychological effects, such as depression or anxiety, may develop due to hormonal changes or chronic illness.
Living with Pituitary Gland Disorders
- Most patients can lead normal, productive lives with proper diagnosis and treatment.
- Lifelong hormone replacement or medication may be necessary.
- Regular follow-up with an endocrinologist is essential for monitoring symptoms and hormone levels.
- Support groups and educational resources can help patients and families cope with long-term management of pituitary diseases.
Frequently Asked Questions (FAQs) About Pituitary Gland Disorders
Q: Are pituitary tumors cancerous?
A: The vast majority of pituitary tumors (adenomas) are benign (noncancerous) and grow slowly. Malignant pituitary tumors are very rare.
Q: What is the most common symptom of a pituitary tumor?
A: Symptoms vary, but common issues include headaches, vision problems, menstrual disturbances, and sexual dysfunction. Some tumors may not cause symptoms and are found incidentally.
Q: Can pituitary gland disorders be cured?
A: Many pituitary disorders can be effectively managed or sometimes cured with surgery, medication, or radiation. Lifelong treatment may be required for certain hormonal deficiencies.
Q: Do pituitary disorders affect fertility?
A: Yes, disorders involving LH, FSH, or prolactin can disrupt reproductive hormone production, leading to infertility, menstrual irregularities, or diminished sex drive in both men and women. Treatment can often restore fertility.
Q: What are the early warning signs of a pituitary disorder?
A: Unexplained gradual changes such as persistent fatigue, unexplained weight change, vision problems, delayed growth or puberty, abnormal milk production, headaches, or sexual/reproductive problems should prompt evaluation. Early detection and treatment are important.
Summary
The pituitary gland plays a central role in the endocrine system, influencing a range of vital bodily functions through hormone production. Pituitary disorders — whether from tumors, trauma, genetic, or systemic causes — can result in diverse and sometimes subtle symptoms. Early recognition, proper diagnosis, and timely treatment are crucial in preventing serious complications and supporting overall health. Regular medical follow-up and patient education empower individuals affected by pituitary diseases to live healthy, fulfilling lives.
References
- https://www.ohsu.edu/sites/default/files/2019-06/Health-Care-Professionals-Guide-to-Pituitary-Disease.pdf
- https://www.uvmhealth.org/conditions-specialties/endocrinology/pituitary-gland-disorders
- https://www.emoryhealthcare.org/conditions/pituitary
- https://www.toplinemd.com/pemc-florida/a-comprehensive-guide-to-understanding-and-managing-pituitary-disorders/
- https://ravindrapatilneuro.com/pituitary-gland-disorders/
- https://www.pituitary.org.uk/information-index/pituitary-conditions/conditions/
- https://www.merckmanuals.com/home/hormonal-and-metabolic-disorders/pituitary-gland-disorders/overview-of-the-pituitary-gland
- https://pituitary.org/product/pituitary-patient-resource-guide/
Read full bio of Sneha Tete












