Dilated Cardiomyopathy: Causes, Symptoms, Diagnosis, and Treatment
Comprehensive guide to causes, symptoms, diagnosis, and management of dilated cardiomyopathy, including FAQs and patient resources.
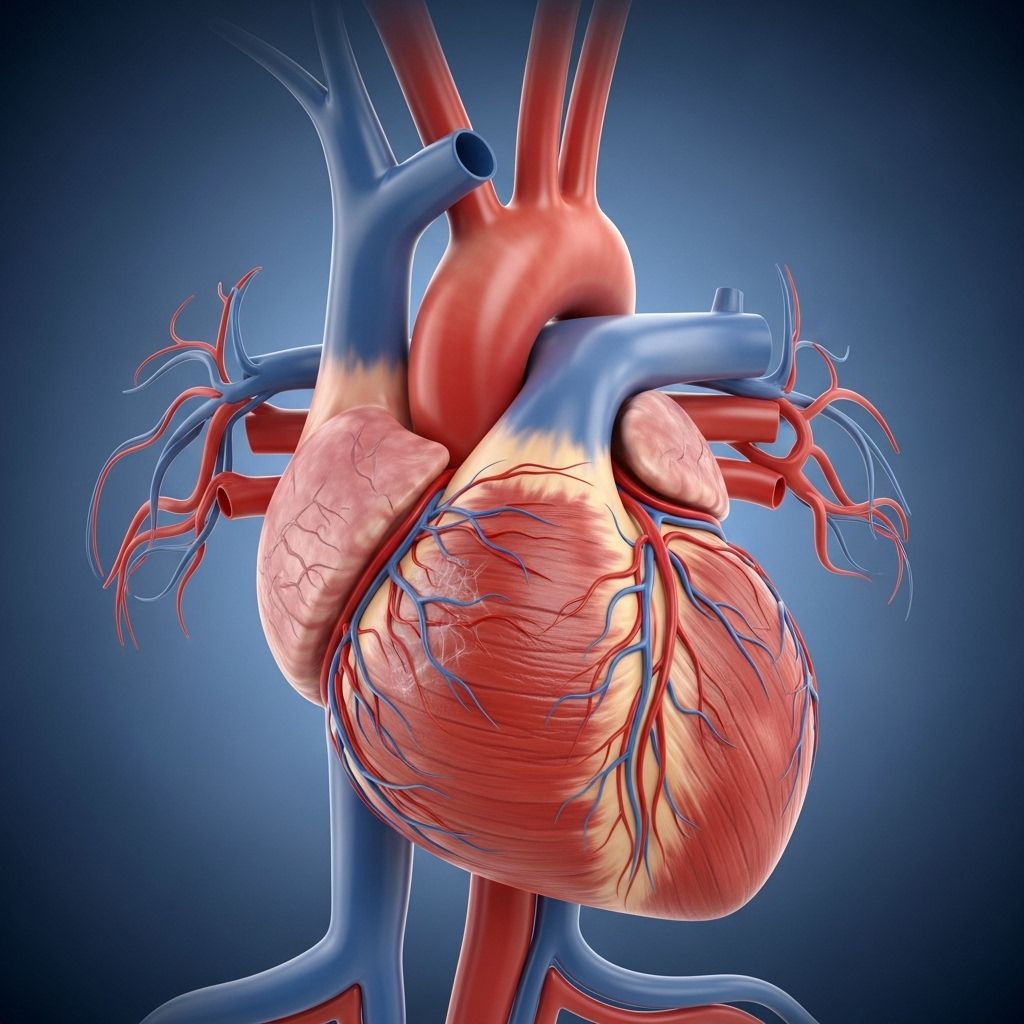
Dilated cardiomyopathy (DCM) is a heart condition characterized by the weakening and enlargement of the left ventricle — the main pumping chamber of the heart. This structural change reduces the heart’s ability to pump blood efficiently to the rest of the body, leading to a variety of symptoms and potential complications. Early recognition, diagnosis, and treatment are essential for managing DCM and supporting heart health.
What is Dilated Cardiomyopathy?
DCM is a form of cardiomyopathy — a disease of the heart muscle — in which the walls of the left ventricle become stretched and thin. As a result, the heart chamber enlarges, losing its ability to contract strongly and pump blood effectively. This can lead to heart failure and other serious health problems.
- Commonly affects adults under 50, but can appear at any age
- Affects men more often than women
- Can occur in people of all ethnic backgrounds
How Common is Dilated Cardiomyopathy?
DCM is one of the most common types of cardiomyopathy. In the United States, about 5 to 6 out of every 100,000 people develop DCM each year. While it often arises in younger adults, about 10% of cases are first diagnosed in individuals over 65 years of age. The condition is about three times more common in males than females and more common in people of African ancestry than in white populations.
Causes and Risk Factors
There are many possible causes of DCM. Sometimes, the cause cannot be identified (idiopathic DCM). In other instances, DCM develops due to known risk factors or health conditions, including:
- Genetic factors: Mutations in specific genes can lead to DCM, and it may run in families.
- Infections: Particularly viral infections (such as Coxsackievirus, HIV, and others) that damage heart muscle.
- Alcohol abuse: Prolonged heavy drinking can weaken the heart muscle.
- Toxins and drugs: Certain chemotherapy agents (e.g., doxorubicin), cobalt, lead, or mercury exposure can damage the heart.
- Autoimmune disorders: Conditions like lupus or sarcoidosis can affect the heart muscle.
- Metabolic and endocrine disorders: Such as thyroid overactivity (hyperthyroidism), diabetes, or nutritional deficiencies.
- Persistent abnormal heart rhythms: Chronic fast heart rhythms (tachycardia) can weaken the heart over time.
- Pregnancy: In rare cases, DCM can develop late in pregnancy or shortly after delivery (peripartum cardiomyopathy).
- Other causes: Conditions like thiamine deficiency (beriberi), certain infections (Chagas disease), and excessive catecholamine hormone levels (from adrenal tumors).
Symptoms of Dilated Cardiomyopathy
Symptoms may appear gradually or suddenly, depending on the cause and stage. Early on, people with DCM may have few or mild symptoms. As the condition progresses, symptoms typically worsen.
- Shortness of breath (dyspnea), especially with exertion or when lying down
- Fatigue or weakness
- Swelling (edema) in the legs, ankles, feet, or abdomen
- Rapid or irregular heartbeats (palpitations)
- Chest pain or discomfort, though this is less common
- Weight gain due to fluid buildup
- Difficulty breathing at night or the need to prop up with pillows (orthopnea)
- Frequent urination at night (nocturia)
- Reduced ability to exercise
- Cough, particularly when lying down
- Bulging neck veins (jugular venous distention)
Symptoms can range from mild to severe, and not everyone experiences the same signs. Occasionally, the first symptom of DCM is a serious complication, such as a heart arrhythmia or sudden cardiac arrest.
Complications of Dilated Cardiomyopathy
Untreated or advanced DCM can lead to a variety of serious health problems:
- Heart failure: The heart cannot supply enough blood and oxygen to the body, leading to severe fatigue and organ dysfunction.
- Arrhythmias: Irregular heartbeats — some potentially life-threatening — such as atrial fibrillation or ventricular tachycardia.
- Heart valve problems: Enlarged ventricles may stretch and distort the heart valves, causing them to leak (regurgitation).
- Blood clots and stroke: Blood pooling in the enlarged ventricle increases the risk of clot formation, which can travel and block blood flow to the brain or other organs.
- Sudden cardiac death: Rare but possible, especially if dangerous arrhythmias occur.
When to See a Doctor
Prompt medical evaluation is important if you develop symptoms such as unexplained shortness of breath, swelling, an irregular heartbeat, chest pain, or persistent fatigue. People with a family history of DCM or sudden cardiac death should discuss screening with their healthcare provider.
How Is Dilated Cardiomyopathy Diagnosed?
Diagnosing DCM involves a combination of medical history, physical examination, diagnostic testing, and sometimes genetic counseling when a hereditary cause is suspected.
Steps in Diagnosis
- Medical history: Including personal and family history of heart disease, symptoms, medication use, substance use, and recent illnesses.
- Physical examination: Listening for heart murmurs, checking for swelling, observing neck veins, and assessing overall health.
Common Diagnostic Tests
- Electrocardiogram (ECG): Measures the electrical activity of the heart and identifies arrhythmias or conduction problems.
- Echocardiogram: Ultrasound imaging to assess heart size, wall thickness, pumping function (ejection fraction), and valve function.
- Chest X-ray: Shows heart enlargement or evidence of fluid buildup in the lungs.
- Blood tests: Look for signs of heart failure, kidney or thyroid disease, infection, and other causes.
- Cardiac MRI: Provides detailed images of the heart’s structure and function, helpful for complex or unclear cases.
- Stress testing: Assesses how the heart handles increased workload and may detect hidden coronary artery disease.
- Coronary angiography: To identify blocked arteries if symptoms suggest coronary artery disease.
- Endomyocardial biopsy: Rarely, a small sample of heart tissue is taken to identify specific causes, such as infection or infiltration.
- Genetic testing: May be suggested in families with inherited forms of cardiomyopathy.
Treatment Options for Dilated Cardiomyopathy
While there is no cure for most cases of DCM, many people live long and productive lives with proper treatment. Management aims to address underlying causes, relieve symptoms, prevent complications, and improve quality of life.
Medications
A set of heart failure medications are used to optimize heart function and prevent worsening symptoms:
- ACE inhibitors and ARBs: Lower blood pressure and reduce heart strain.
- Beta blockers: Slow heart rate, reduce arrhythmia risk, and lower blood pressure.
- Aldosterone antagonists: Help the body eliminate extra salt and fluid; protect heart muscle.
- Diuretics (water pills): Reduce fluid buildup and swelling.
- SGLT2 inhibitors: A diabetes medication now also used to reduce heart failure risk.
- Neprilysin inhibitors: Improve heart function by helping eliminate sodium and reduce blood pressure.
- Digoxin: Sometimes used to improve heart pumping strength and control some arrhythmias.
- Anticoagulants (blood thinners): Prevent blood clots if the risk is high.
- Anti-arrhythmic drugs: Used when arrhythmias are present or likely.
Lifestyle Changes
- Quit smoking and limit alcohol: Both can worsen heart failure.
- Heart-healthy diet: Emphasize whole grains, fruits, vegetables, lean protein; limit sodium and saturated fat.
- Regular physical activity: Participating in mild to moderate exercise as recommended, or Cardiac Rehabilitation if referred by your doctor.
- Monitor weight: Sudden increases can signal fluid retention.
- Manage blood pressure and cholesterol: Keep both within target ranges.
- Stay current with vaccinations: Especially flu and pneumonia vaccines to reduce infection risk.
Medical Devices and Surgical Treatments
- Implantable cardioverter-defibrillator (ICD): Stops dangerous arrhythmias and reduces sudden cardiac death risk.
- Cardiac resynchronization therapy (CRT) device: A special pacemaker that coordinates heartbeats for those with electrical conduction delays.
- Left ventricular assist device (LVAD): A mechanical pump to help a weakened heart, often as a bridge to heart transplantation or as destination therapy.
- Heart valve surgery: To repair or replace leaky valves identified as contributing to heart failure.
- Heart transplantation: Considered in advanced cases where standard treatments are not effective.
Prevention Strategies
While not all cases of DCM can be prevented, the following steps can help reduce risk:
- Avoid excessive alcohol and drugs known to harm the heart.
- Manage chronic health conditions: Control high blood pressure, diabetes, and thyroid disorders.
- Protect against infections: Stay current on vaccinations; practice good hygiene.
- Genetic counseling: If you have a family history, discuss screening and prevention with a healthcare provider.
Living with Dilated Cardiomyopathy
A diagnosis of DCM can be life-changing, but many people find they can lead fulfilling lives by following their treatment plan and making healthy lifestyle choices. Here are some tips:
- Take medications exactly as prescribed.
- Follow up regularly with your healthcare team.
- Report changes in symptoms promptly.
- Participate in cardiac rehabilitation if recommended.
- Join a support group or connect with others living with heart conditions.
Prognosis
The outcome for people with DCM varies depending on the underlying cause, the severity at diagnosis, response to therapy, and other medical problems. Some individuals experience stable symptoms for many years, while others may need advanced therapies. Early and effective management improves outcomes and quality of life for most people.
Frequently Asked Questions (FAQs)
What causes dilated cardiomyopathy?
DCM can result from genetic conditions, infections, toxins (like chemotherapy or alcohol), metabolic or endocrine disorders, autoimmune diseases, and sometimes no clear cause is found.
Is dilated cardiomyopathy reversible?
Depending on the underlying cause, some cases (such as those due to alcohol or certain infections) may improve if the trigger is removed, but most require lifelong management.
Can children get dilated cardiomyopathy?
Yes. Although DCM is most common in adults, it can also occur in infants and children, often due to genetic causes, infections, or metabolic disorders.
Is it safe to exercise with DCM?
Light to moderate exercise is generally safe and helpful for most people with DCM, but always consult your doctor for recommendations. Cardiac rehabilitation programs offer supervised, safe activity plans.
How serious is dilated cardiomyopathy?
DCM is a serious condition that requires medical attention. With appropriate treatment, many people can manage symptoms and maintain a good quality of life. In some cases, however, DCM can progress to advanced heart failure or life-threatening arrhythmias.
What is the life expectancy with dilated cardiomyopathy?
Prognosis varies widely. Some people live many years with well-controlled symptoms, while others may require advanced treatments. Early diagnosis and consistent care improve chances of longer and better quality life.
Key Points
- Dilated cardiomyopathy is a condition where the heart’s main pumping chamber enlarges and weakens, reducing its efficiency.
- Common causes include genetics, infections, alcohol, toxins, and metabolic disorders, but many cases have no identifiable cause.
- Symptoms include shortness of breath, fatigue, edema, and palpitations.
- Diagnosis relies on tests such as echocardiogram, ECG, chest X-ray, and blood work.
- Treatment typically includes heart failure medications, lifestyle changes, and sometimes devices or surgery.
- Timely care can help people with DCM live longer, healthier lives.
Additional Resources
- American Heart Association: Patient education and support resources
- Heart Failure Society of America: Guidance and information for patients and families
- Genetic counseling services: Recommended for those with a family history of cardiomyopathy
References
- https://www.merckmanuals.com/professional/cardiovascular-disorders/cardiomyopathies/dilated-cardiomyopathy
- https://utswmed.org/conditions-treatments/dilated-cardiomyopathy/
- https://www.pennmedicine.org/conditions/dilated-cardiomyopathy
- https://www.mayoclinic.org/diseases-conditions/dilated-cardiomyopathy/diagnosis-treatment/drc-20353155
- https://my.clevelandclinic.org/health/diseases/16932-dilated-cardiomyopathy
- https://www.mayoclinic.org/diseases-conditions/dilated-cardiomyopathy/symptoms-causes/syc-20353149
- https://www.ncbi.nlm.nih.gov/books/NBK441911/
- https://www.youtube.com/watch?v=3GTSVYocP8c
- https://my.clevelandclinic.org/health/diseases/16841-cardiomyopathy
Read full bio of Sneha Tete












