Heart Attack vs. Cardiac Arrest: Understanding the Key Differences
Learn how heart attacks and cardiac arrests differ in symptoms, causes, treatment, and prevention to be prepared and save lives.
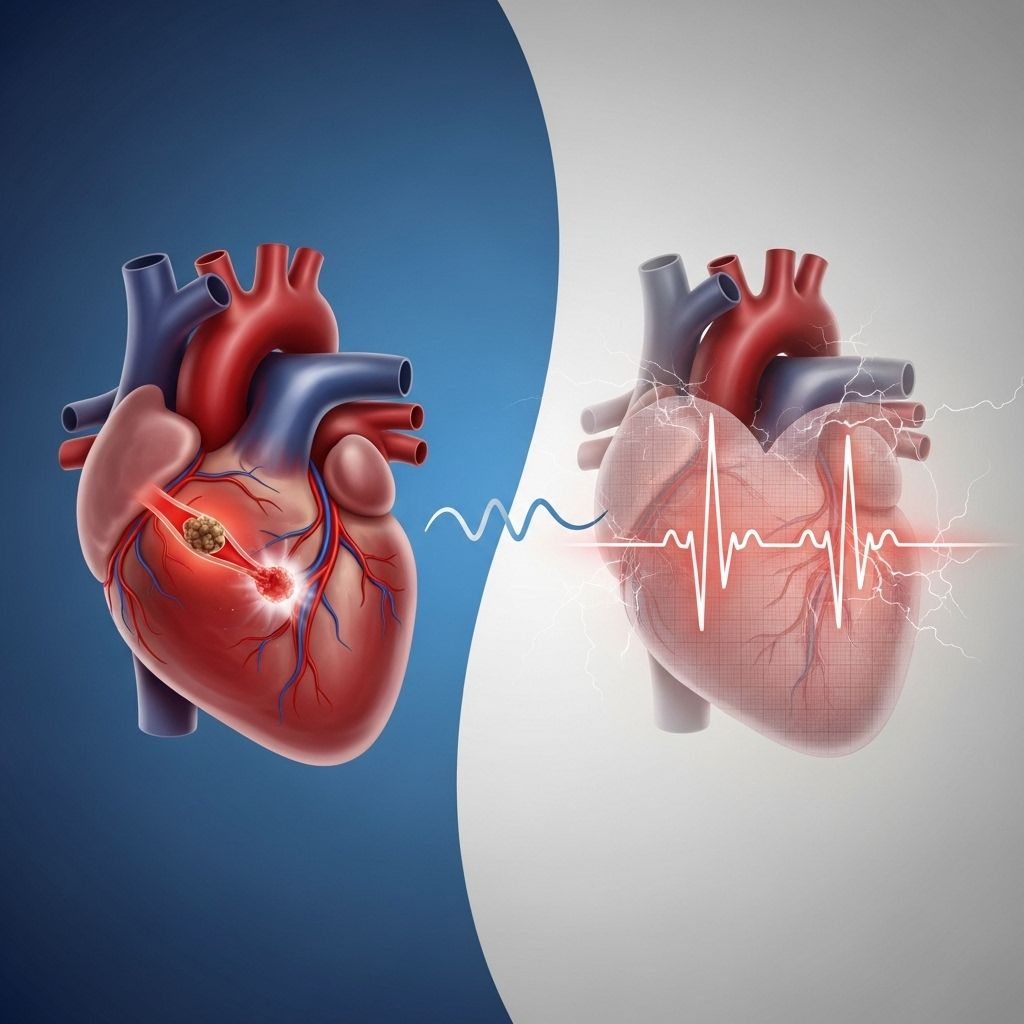
Both heart attacks and cardiac arrests are serious and potentially fatal emergencies involving the heart, but they are very different conditions with unique causes, symptoms, treatment approaches, and long-term risks. Understanding these distinctions is vital not just for healthcare professionals but for everyone, as quick recognition and response can save lives. This comprehensive guide explains what sets heart attacks and cardiac arrest apart, outlines their symptoms and risk factors, and offers practical advice for emergency situations and prevention.
Overview: Heart Attack vs. Cardiac Arrest
| Heart Attack | Cardiac Arrest | |
|---|---|---|
| Main Cause | Blocked blood flow to the heart muscle (circulation problem) | Electrical malfunction causing the heart to stop (electrical problem) |
| Typical Symptoms | Chest pain, shortness of breath, nausea, sweating | Sudden collapse, loss of consciousness, no pulse, no breathing |
| Onset | May be gradual or sudden | Always sudden and unexpected |
| Heart Stops? | Rarely | Yes, heart stops pumping effectively |
| Emergency Response | Call 911, medications, possible surgery | Call 911, immediate CPR and defibrillation |
| Common Link | Can increase risk of cardiac arrest | May be triggered by a heart attack |
What Is a Heart Attack?
A heart attack, medically termed myocardial infarction, occurs when blood flow to part of the heart muscle is blocked, usually by a clot or build-up of plaque in a coronary artery. Without sufficient oxygen, the heart muscle tissue begins to suffer damage and may die if the blockage isn’t promptly cleared. In most cases, the heart continues to beat during a heart attack, but parts of the muscle can be severely compromised.
- Cause: A blockage in one or more coronary arteries reduces or stops blood flow to the heart muscle.
- Typical Symptoms:
- Chest discomfort or pain (can be sharp, tight, or squeezing)
- Pain radiating to neck, jaw, back, or arms
- Shortness of breath
- Nausea or vomiting
- Cold sweat
- Lightheadedness or fainting
- Variability: Symptoms may be mild, severe, start suddenly, or progress slowly. Some people, especially women, may have less typical symptoms like fatigue, indigestion, or upper abdominal discomfort.
If the blockage is not treated quickly, damage to the heart muscle increases, leading to potentially permanent impairment of heart function. Immediate emergency care is essential.
What Is Cardiac Arrest?
Cardiac arrest happens when the heart experiences a sudden electrical malfunction, leading it to stop beating effectively or altogether. This disrupts the flow of oxygen-rich blood to the brain and vital organs. Without immediate intervention, cardiac arrest results in rapid loss of consciousness and can quickly be fatal.
- Cause: An electrical disorder, often a life-threatening arrhythmia (abnormal rhythm) such as ventricular fibrillation or ventricular tachycardia, disrupts the normal pumping action of the heart.
- Typical Symptoms:
- Sudden collapse
- Loss of consciousness
- Absence of pulse and breathing
- Sometimes preceded by dizziness or chest discomfort, but usually occurs with no warning
- Rapid Progression: Brain and organ damage start within minutes; death occurs if circulation is not restored promptly with CPR and defibrillation.
Causes: Blockage vs. Electrical Malfunction
Heart Attack: The “Plumbing” Problem
Most heart attacks are caused by coronary artery disease, where fatty deposits (plaques) build up on artery walls. If a plaque ruptures, a blood clot can form, blocking blood flow.
- Primary triggers:
- Plaque buildup and rupture in coronary arteries
- Blood clot (thrombosis)
- Severe artery spasm (rare)
- Risk factors: High cholesterol, high blood pressure, smoking, diabetes, obesity, sedentary lifestyle, family history
Cardiac Arrest: The “Electrical” Problem
Cardiac arrest is most often triggered by disturbances in the heart’s electrical system, resulting in dangerous rhythms that stop effective pumping. While sometimes occurring in healthy people, arrest is more often linked to underlying heart disease.
- Common causes:
- Ventricular fibrillation (disorganized electrical activity)
- Ventricular tachycardia (very rapid heartbeat)
- Heart failure
- Certain inherited heart conditions
- Severe trauma, electric shock, or drowning
- Drugs or severe electrolyte disturbances
- Risk factors: Previous heart attack, cardiomyopathy, other heart conditions, electrolyte imbalance, drug misuse, genetic predispositions
Key Symptoms: How to Recognize Each Emergency
Heart Attack Symptoms
- Chest pain or discomfort (often in the center or left side)
- Pain or discomfort in arms, back, neck, jaw, or stomach
- Shortness of breath
- Breaking out in a cold sweat
- Nausea or vomiting
- Dizziness or light-headedness
- Fatigue (especially in women)
Cardiac Arrest Symptoms
- Sudden collapse without warning
- No pulse or breathing
- Person becomes unresponsive, unconscious
- Occasionally, preceded by palpitations, chest discomfort, dizziness, or shortness of breath—but usually strikes without warning
Relationship Between Heart Attack and Cardiac Arrest
While the two conditions are distinct, they are sometimes related:
- A heart attack can trigger cardiac arrest, especially if the heart muscle becomes so damaged that it induces a fatal arrhythmia.
- During or soon after a heart attack, people are at higher risk of experiencing cardiac arrest.
- Both conditions often share similar risk factors, such as age, existing heart disease, high blood pressure, and others.
Emergency Response: What To Do
If You Suspect a Heart Attack
- Call emergency services (911) immediately.
- Encourage the person to stop all activity and rest.
- If not allergic or contraindicated, administer aspirin and have them chew it (to help thin blood).
- Monitor vital signs and provide reassurance until help arrives.
If You Suspect Cardiac Arrest
- Check for responsiveness—no response, no pulse, and no normal breathing means cardiac arrest is likely.
- Call emergency services (911) immediately.
- Begin chest compressions (Hands-Only CPR):
- Push hard and fast in the center of the chest at a rate of 100–120 compressions per minute.
- If an Automated External Defibrillator (AED) is available, use it as soon as possible. Follow its instructions.
- Continue CPR until professional help arrives or the person responds.
Which is More Serious?
Both conditions are emergencies and can be fatal if not treated swiftly. However:
- Cardiac arrest is more immediately life-threatening. Without CPR and defibrillation, most people die within minutes.
- Heart attacks are also dangerous; untreated, they can lead to severe heart damage, disability, or death, and may potentially trigger cardiac arrest.
Risk Factors: Who Is at Risk?
- Advanced age
- Family or personal history of heart disease
- High blood pressure
- High cholesterol
- Diabetes
- Obesity or overweight
- Smoking or tobacco use
- Physical inactivity
- Chronic stress
- Drug or alcohol misuse
- Certain inherited or congenital heart conditions (especially for cardiac arrest)
Managing these factors through a heart-healthy lifestyle and regular check-ups lowers risk of both conditions.
Prevention: How to Reduce Your Risk
- Adopt a heart-healthy diet (low in saturated fat, high in fiber, rich in fruits and vegetables)
- Exercise regularly (most adults should aim for 150 minutes/week of moderate physical activity)
- Quit smoking and avoid secondhand smoke exposure
- Maintain a healthy weight
- Control blood pressure, cholesterol, and blood sugar through medication and lifestyle, as advised
- Limit alcohol intake
- Manage stress with relaxation, mindfulness, or counseling
- Discuss with your doctor about regular screening and risk assessment, especially if you have a family history or other risk factors
Frequently Asked Questions (FAQs)
How is cardiac arrest different from a heart attack?
A heart attack is caused by a blood flow blockage to the heart muscle (a circulation problem), while cardiac arrest comes from a sudden electrical malfunction in the heart that interrupts its pumping action (an electrical problem). Heart attacks may trigger cardiac arrest but are not always linked.
What should I do if someone collapses in front of me?
First, check if the person is responsive and breathing. If not, call 911 immediately, start chest compressions (CPR), and use an AED if available. Rapid response is crucial for survival in cardiac arrest.
Are there warning signs before cardiac arrest?
Cardiac arrest often strikes with little or no warning, but sometimes symptoms like palpitations, chest discomfort, shortness of breath, or dizziness may occur briefly beforehand. Most commonly, there are no clear early signs.
Can someone survive a heart attack or cardiac arrest?
Yes, rapid emergency treatment greatly improves survival for both. With heart attacks, restoring blood flow to the heart quickly reduces permanent damage. In cardiac arrest, immediate CPR and defibrillation provide the best chances of survival. Every minute counts.
Is it possible to have both a heart attack and cardiac arrest?
Yes. A heart attack can trigger a dangerous arrhythmia, leading to cardiac arrest. People recovering from a heart attack are also at higher risk for cardiac arrest in the hours and days afterward.
How can I lower my risk of either condition?
Adopt a healthy lifestyle: eat well, exercise, avoid tobacco, manage stress, control risk factors like blood pressure and cholesterol, and have regular check-ups. Promptly address any new symptoms by seeking medical advice.
Key Takeaways
- Heart attacks are caused by blocked arteries restricting blood flow to the heart; the heart usually continues beating.
- Cardiac arrest is caused by a sudden electrical failure, stopping the heart from pumping blood and causing immediate collapse.
- Both require immediate emergency care — 911, CPR, and/or defibrillation can save lives.
- Recognizing symptoms and acting quickly is crucial for the best outcomes.
- Maintaining a heart-healthy lifestyle and managing risk factors reduces your risk of both conditions.
References
- https://www.jnj.com/health-and-wellness/whats-the-difference-between-a-heart-attack-and-cardiac-arrest
- https://www.heart.org/en/health-topics/heart-attack/about-heart-attacks/heart-attack-or-sudden-cardiac-arrest-how-are-they-different
- http://www.wth.org/blog/the-facts-cardiac-arrest-is-not-the-same-a-heart-attack/
- https://www.uchealth.com/en/media-room/articles/know-the-signs-help-save-a-life-sudden-cardiac-arrest-vs-heart-attack
- https://www.henryford.com/Services/Cardiology/Support/Diagnosis/Heart-attack-vs-sudden-cardiac-arrest
- https://www.bhf.org.uk/informationsupport/heart-matters-magazine/medical/heart-attack-and-cardiac-arrest
- https://my.clevelandclinic.org/health/diseases/21736-cardiac-arrest
- https://www.nghs.com/heart/differences-heart-attack-cardiac-arrest
- https://www.youtube.com/shorts/BbGdAJ5XbOQ
Read full bio of medha deb












