Diagnosis and Treatment of Esophagitis: A Comprehensive Guide
Explore modern diagnostic strategies and effective treatments for esophagitis, ensuring lasting relief and gastrointestinal health.
Esophagitis refers to inflammation of the esophagus, the muscular tube that carries food from your mouth to your stomach. Prompt and accurate diagnosis is crucial to prevent complications and determine the most appropriate course of treatment. This guide details the diagnostic procedures, medical treatments, lifestyle changes, and surgical options commonly used for managing esophagitis.
Diagnosis
Diagnosing esophagitis involves a combination of thorough history-taking, physical examination, and specialized medical tests. Healthcare providers focus on pinpointing the type of esophagitis and ruling out other possible causes of symptoms.
Clinical Evaluation
- Discussion of symptoms: Healthcare providers will inquire about swallowing difficulties, chest pain, heartburn, regurgitation, or food impaction.
- Physical exam: General assessment may reveal signs associated with underlying causes, such as allergies or infections.
Common Diagnostic Tests
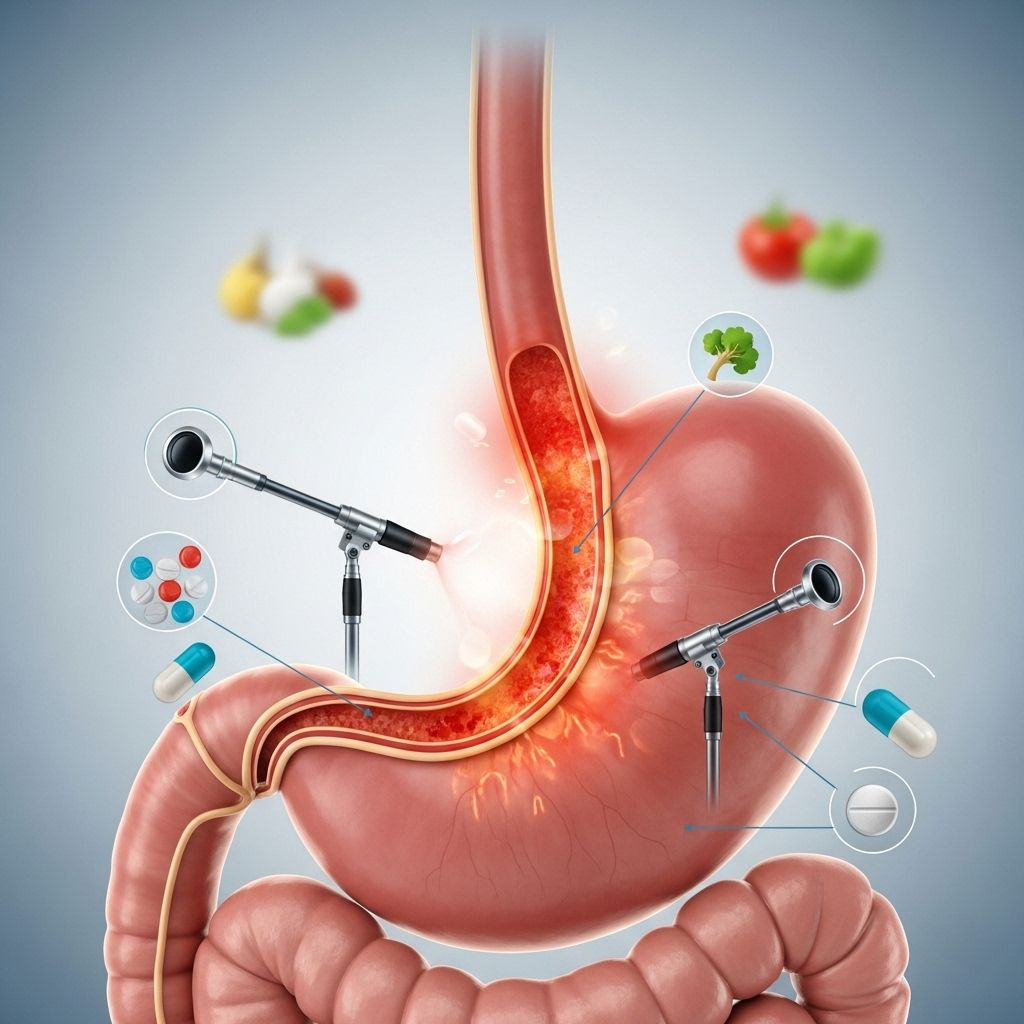
Endoscopy
Endoscopy involves inserting a flexible tube (endoscope) with a small camera through the mouth to directly view the esophagus, stomach, and upper small intestine.
- Visual assessment: Providers look for evidence of inflammation, swelling, rings, furrows, strictures (narrowing), erosions, bleeding, or white plaques.
- Biopsy: Small tissue samples are often taken during endoscopy for microscopic analysis. This helps identify the type of inflammation, such as eosinophilic, infectious, or reflux-induced changes.
- Before the procedure, sedatives are usually provided to enhance patient comfort.
Esophageal Sponge Test
For some patients, a minimally invasive esophageal sponge test may be used. This involves swallowing a capsule attached to a string. Inside the stomach, it releases a sponge. The sponge is then withdrawn through the mouth, collecting tissue for analysis. This can help assess inflammation without the need for full endoscopy.
Imaging and Additional Tests
- Barium swallow X-ray: You drink a contrast liquid (barium), and X-rays track its path down the esophagus, revealing strictures, ulcers, or structural changes.
- Blood tests: May be ordered if allergic or infectious causes are suspected. Eosinophil counts and immunoglobulin E (IgE) levels may be elevated in eosinophilic esophagitis.
Specialized Testing for Allergens
- For eosinophilic esophagitis, allergy testing may be performed to identify dietary or environmental triggers.
| Test | Purpose | Key Findings |
|---|---|---|
| Endoscopy | Visualize esophagus, obtain tissue samples | Inflammation, strictures, plaques, erosions |
| Biopsy | Microscopic diagnosis | Eosinophils, infections, cell changes |
| Barium swallow | Assess structure and motility | Strictures, narrowing, ulcers |
| Esophageal Sponge | Sample tissue noninvasively | Inflammatory cells |
| Blood tests | Check allergic response or infection | High eosinophil/IgE count |
Treatment Options
Treatment for esophagitis is determined by the underlying cause, severity, and duration of symptoms. Therapy often includes one or more of the following strategies:
Medications
- Proton pump inhibitors (PPIs): These medications (e.g., omeprazole, lansoprazole) are commonly prescribed to decrease acid production and promote healing. They are standard therapy for reflux-induced esophagitis and can help in other forms when acid reflux is a factor.
- Topical steroids: Swallowed corticosteroids (e.g., fluticasone, budesonide) are used for eosinophilic esophagitis. These medicines reduce inflammation by delivering a localized anti-inflammatory effect with minimal systemic absorption.
- Monoclonal antibodies: Dupilumab (Dupixent) is an advanced treatment for eosinophilic esophagitis, approved for those aged 12 and older. It targets specific pathways in allergic inflammation and is reserved for moderate to severe cases.
- Antacids and H2 blockers: Over-the-counter antacids and H2 receptor antagonists (e.g., famotidine) may be used for milder symptoms or adjunct therapy in reflux-related esophagitis.
- Antibiotics, antifungals, antivirals: In cases caused by infections (e.g., candida, herpes virus), targeted antimicrobial medications are necessary.
Dietary and Lifestyle Modification
- Food elimination diet: For eosinophilic esophagitis, an elimination diet — often removing common allergens like dairy, wheat, soy, eggs, nuts, and seafood — may be recommended. Foods are gradually reintroduced to determine which ones cause reactions.
- Smaller, frequent meals: Large meals and late-night eating can aggravate reflux. Smaller, more frequent meals may reduce symptoms.
- Weight management: Maintaining a healthy weight can alleviate pressure on the stomach and reduce reflux risk.
- Avoiding trigger foods and substances: Spicy foods, alcohol, caffeine, and tobacco often worsen symptoms for many people.
Procedures and Surgery
- Esophageal dilation: For significant narrowing (strictures), a provider may gently stretch the esophagus during endoscopy to ease swallowing difficulties. This is important for strictures seen in chronic or advanced cases.
- Surgical interventions: Rarely needed, but considered for severe or unresponsive esophagitis, or if complications like perforation occur.
Alternative and Adjunctive Therapies
- Allergy management: If allergies play a role, allergy medications or immunotherapy may help control inflammation.
- Patient education: Understanding triggers, medication use, correct administration of swallowed steroids, and adherence to dietary recommendations can greatly improve long-term outcomes.
Monitoring and Follow-Up
After initiating treatment, follow-up is essential to monitor symptom improvement and check for complications. Repeat endoscopy or other assessments may be necessary if symptoms persist, worsen, or return after initial improvement.
Potential Complications
If not properly treated, esophagitis can lead to potentially serious complications:
- Chronic pain and swallowing difficulties: Persistent inflammation can cause ongoing symptoms.
- Stricture formation: Scarring and narrowing of the esophagus may occur, requiring dilation procedures.
- Barrett’s esophagus: In severe cases of chronic inflammation from reflux, precancerous changes can develop.
- Esophageal ulcers: Deep erosions may bleed, cause pain, or lead to infection.
- Perforation: Rarely, severe inflammation can create a hole in the esophagus, a medical emergency.
Prevention Strategies
Some of the best ways to prevent the recurrence of esophagitis or reduce your risk include:
- Manage underlying conditions (allergies, reflux, immune issues)
- Follow dietary guidance and avoidance of personal triggers
- Avoid tobacco and moderate alcohol consumption
- Use medications as directed
- Promptly report new or worsening symptoms to your healthcare provider
When to Seek Medical Care
It’s important to consult a healthcare professional promptly if you experience:
- Frequent or severe difficulty swallowing
- Pain unrelieved by over-the-counter medicines
- Unintentional weight loss or chronic vomiting
- Food impaction (food stuck in the esophagus)
- Bleeding (vomiting blood, or black/tarry stools)
Frequently Asked Questions (FAQ)
What causes esophagitis?
Esophagitis can result from acid reflux (GERD), medications, infections, allergens (as in eosinophilic esophagitis), or physical injury. Accurate diagnosis helps identify the specific type and cause.
How is esophagitis treated?
Treatment depends on the cause and may include acid suppression (PPIs), topical steroids, dietary changes, treating infections, or esophageal dilation for strictures.
Can esophagitis resolve on its own?
Mild cases related to brief irritation may resolve with simple interventions, but untreated or recurrent esophagitis often requires ongoing management to prevent complications and recurrence.
Are there long-term risks associated with esophagitis?
Yes. Chronic esophagitis, particularly from reflux or eosinophilic causes, can lead to strictures, Barrett’s esophagus, or rarely esophageal cancer. Long-term follow-up is important for those at risk.
How long does it take to heal esophagitis?
This depends on severity and cause. With appropriate therapy, healing can occur within weeks. Chronic forms may require long-term or repeating treatments.
Conclusion
An accurate diagnosis and tailored treatment plan are vital for effectively managing esophagitis. Collaboration between patient and healthcare providers, timely interventions, and ongoing follow-up offer the best path toward relief and prevention of complications.
References
- https://www.mayoclinic.org/diseases-conditions/esophagitis/care-at-mayo-clinic/mac-20361414
- https://www.mayoclinic.org/diseases-conditions/eosinophilic-esophagitis/care-at-mayo-clinic/mac-20372209
- https://www.mayoclinic.org/diseases-conditions/eosinophilic-esophagitis/diagnosis-treatment/drc-20372203
- https://www.youtube.com/watch?v=aq0WorgaRsQ
- https://www.mayoclinic.org/diseases-conditions/esophagitis/diagnosis-treatment/drc-20361264
- https://www.mayoclinic.org/diseases-conditions/esophagitis/symptoms-causes/syc-20361224
- https://www.mayoclinic.org/diseases-conditions/eosinophilic-esophagitis/symptoms-causes/syc-20372197
- https://www.mayoclinic.org/diseases-conditions/esophageal-cancer/diagnosis-treatment/drc-20356090
- https://www.kuh.ku.edu.tr/mayo-clinic-care-network/mayo-clinic-health-information-library/diseases-conditions/esophagitis
Read full bio of medha deb












