Diabetic Retinopathy vs. Diabetic Macular Edema: Causes, Symptoms, and Key Differences Explained
Understand the critical differences and connections between diabetic retinopathy and diabetic macular edema to protect your vision and manage diabetes-related eye risks.
Diabetic Retinopathy vs. Diabetic Macular Edema: The Essential Guide
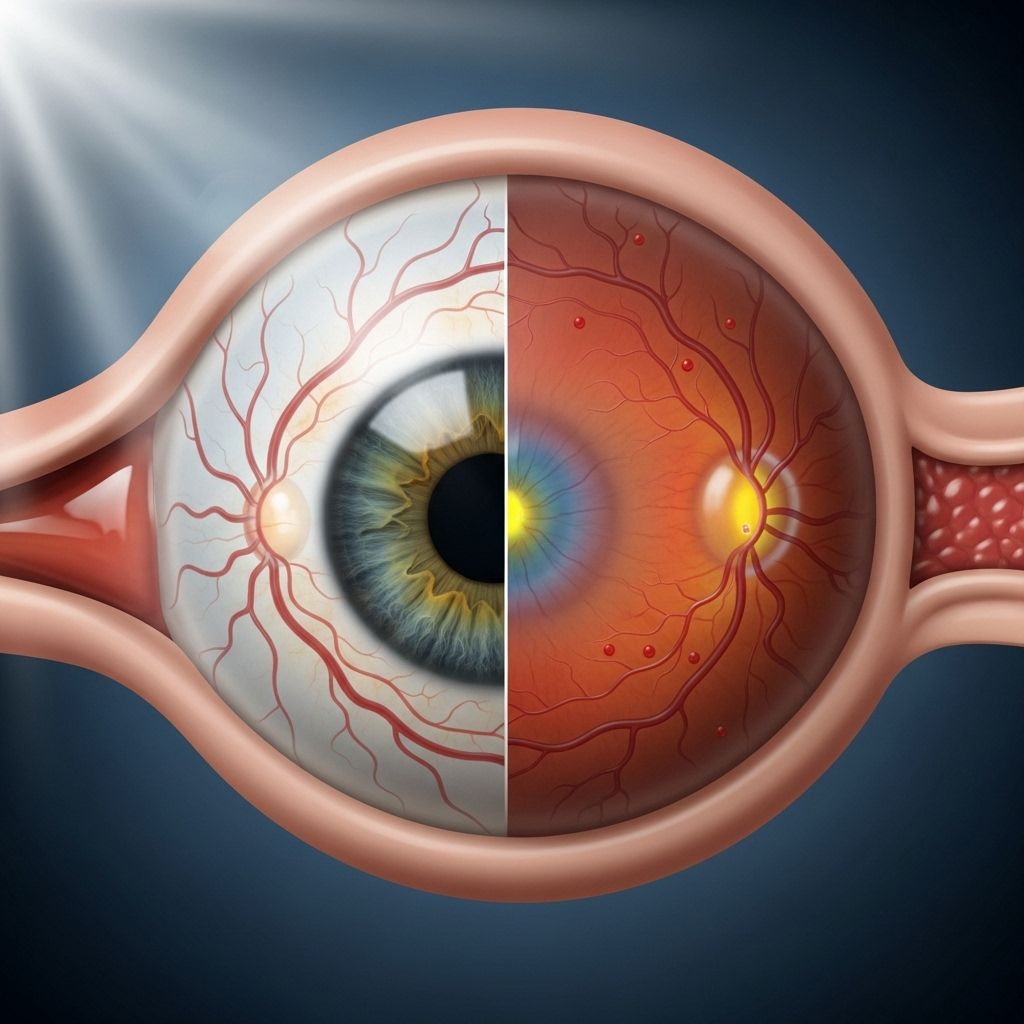
Diabetic retinopathy (DR) and diabetic macular edema (DME) are two serious eye conditions, both closely linked to diabetes. While they can both result in vision loss, understanding how they differ in causes, symptoms, progress, and management is vital for anyone living with diabetes. This guide explains everything you need to know about these diabetes-related eye disorders—including their impact, diagnosis, prevention, and frequently asked questions.
Are Diabetic Retinopathy and Diabetic Macular Edema the Same?
Diabetic retinopathy and diabetic macular edema are related but distinct conditions. Diabetic retinopathy refers to the overall damage diabetes can cause to the retina—the light-sensitive tissue lining the back of the eye. Diabetic macular edema, or DME, is a specific complication of diabetic retinopathy that affects the macula, the central part of the retina responsible for sharp, straight-ahead vision and color perception.
| Condition | Definition | Main Symptoms | Cause |
|---|---|---|---|
| Diabetic Retinopathy | Damage to retinal blood vessels due to high blood sugar | Blurred/fluctuating vision, floaters, poor night vision, no early symptoms | Chronic hyperglycemia weakens and bursts small blood vessels in the retina |
| Diabetic Macular Edema | Swelling of the macula from fluid leakage caused by retinopathy | Blurry/double vision, floaters, dull colors, trouble recognizing faces, blind spots | Leaky blood vessels from diabetic retinopathy cause fluid accumulation in the macula |
Key Differences
- Diabetic retinopathy can occur without DME.
- All cases of DME in diabetes result from diabetic retinopathy.
- Both conditions may progress without obvious symptoms at first, emphasizing the need for regular eye exams if you have diabetes.
Diabetic Retinopathy: Causes, Stages, and Risks
Diabetic retinopathy is a progressive disease stemming from elevated blood sugar levels over long periods. The retina, a layer of tissue at the back of the eye, is crucial for sensing light and sending visual information to the brain. Chronically high blood sugar levels interfere with the blood flow to the retina and damage small blood vessels, causing them to bulge, weaken, and sometimes leak fluid or blood into retinal tissues.
Stages of Diabetic Retinopathy
- Nonproliferative Diabetic Retinopathy (NPDR): Early stage. Blood vessels leak fluid, causing swelling, but new blood vessel growth has not yet begun.
- Proliferative Diabetic Retinopathy (PDR): Advanced stage. The eye attempts to compensate for lack of blood supply by forming new, fragile blood vessels, which are prone to leaking and can result in scar tissue.
Complications of Advanced Retinopathy
- DME (Diabetic Macular Edema)
- Retinal detachment
- Vitreous hemorrhage (bleeding inside the eye)
- Elevated eyeball pressure
- Nerve damage
- Glaucoma
- Partial or complete vision loss
Who Is at Risk?
- Both type 1 and type 2 diabetes can develop retinopathy.
- Approximately 75% of people with type 1 and 50% with type 2 diabetes experience retinopathy in their lifetime.
- Long-term high blood sugar increases risk and severity.
- Poor control of blood pressure and cholesterol further heighten risks.
Diabetic Macular Edema: Definition, Symptoms, and Impact
DME is a direct complication of diabetic retinopathy, impacting the macula—the center of the retina. The macula is responsible for central vision and perceiving fine details and color. As diabetic retinopathy progresses, blood vessel leakage overwhelms the retina’s ability to absorb excess fluid, leading to swelling and thickening of the macula.
Symptoms of Diabetic Macular Edema
- Blurred or distorted vision
- Double or wavy vision
- Dark spots or floaters
- Blind spots
- Dull or faded color perception
- Trouble recognizing faces
- Difficulty with tasks requiring detailed sight (e.g., reading fine print)
- Partial or complete vision loss
It’s possible to have significant DME and notice hardly any symptoms, depending on the location and severity of the swelling.
Can Diabetic Macular Edema Occur Without Retinopathy?
No—DME cannot occur without diabetic retinopathy. If you have DME and diabetes, you always have retinopathy. However, retinopathy can occur without DME, especially in earlier stages.
Notably, macular edema itself isn’t exclusive to diabetes. People can develop macular edema from other causes such as:
- Complications from eye surgery (cataract, glaucoma, or retina procedures)
- Age-related macular degeneration
- Blocked retinal veins due to high blood pressure, glaucoma, or atherosclerosis
- Inflammatory conditions (e.g., uveitis, retinal necrosis, toxoplasmosis)
Early Detection and Eye Health in Diabetes
Both diabetic retinopathy and DME may develop silently in their initial phases. For this reason, routine diabetic eye exams are essential for early detection and the best chance to preserve vision. Many ophthalmologists recommend annual eye screenings for people with diabetes, more frequent visits for those with known retinal changes, or risk factors for rapid progression.
Typical Progression and Signs
- Early stages may cause no symptoms at all.
- As retinopathy progresses, symptoms like blurry vision, floaters, dark spots, and poor night vision may arise.
- DME primarily impacts central vision and detail, making reading and facial recognition difficult.
Diagnosis: How Are These Conditions Identified?
Diagnosis is typically made during a comprehensive eye exam, which may include:
- Visual acuity testing to assess clarity of vision.
- Dilated eye examination where special eye drops widen the pupil for clearer retinal assessment.
- Optical coherence tomography (OCT) to measure retinal thickness and fluid accumulation.
- Fluorescein angiography to detect blood vessel leaks and evaluate retinal circulation.
Treatment Options for Diabetic Retinopathy and DME
Treatment approaches depend on the stage, severity, and specific symptoms of each condition.
Diabetic Retinopathy
- Blood sugar control: Maintaining healthy glucose levels is fundamental to slowing progression.
- Blood pressure & cholesterol management: Reduce additional vascular injury risk.
- Laser therapy (photocoagulation): Focal or panretinal lasers seal leaking blood vessels and prevent further deterioration.
- Vitrectomy: Surgical removal of blood, scar tissue, or vitreous gel for severe bleeding or retinal detachment.
- Anti-VEGF injections: Medications injected into the eye to reduce abnormal blood vessel growth and leakage.
Diabetic Macular Edema
- Anti-VEGF injections: Highly effective therapy to reduce fluid and swelling in the macula.
- Steroid injections or implants: May be used for persistent edema not responsive to anti-VEGF.
- Focal or grid laser therapy: Used in select cases to target leaky blood vessels.
- Blood sugar & systemic risk control: Always recommended as part of the management plan.
Most modern treatments are relatively painless and can prevent substantial vision loss—especially when started early.
Prevention and Vision Protection
Living with diabetes doesn’t have to lead to vision loss. Several strategies greatly reduce the risk and severity of diabetic eye disease:
- Regular eye exams—even if you have no symptoms
- Careful blood sugar management
- Controlling blood pressure and cholesterol
- Not smoking
- Physical activity and healthy diet
Early intervention is critical. Vision lost from advanced diabetic retinopathy or DME may not be recoverable, but vision can often be preserved or improved if treatment is started before irreversible damage occurs.
Frequently Asked Questions (FAQs)
Q: Can you have diabetic retinopathy without macular edema?
A: Yes. Diabetic retinopathy affects the retina as a whole, and DME is specifically a complication involving swelling of the macula. Not all people with diabetic retinopathy develop DME.
Q: Is diabetic macular edema exclusive to diabetes?
A: No. While diabetic retinopathy is the most common cause of DME, macular edema can result from other non-diabetic causes such as eye surgery, vein occlusions, or inflammatory conditions.
Q: How often should someone with diabetes get an eye exam?
A: Annual eye exams are recommended. Those already diagnosed with retinopathy or DME may need more frequent screenings depending on their individual risk.
Q: Are symptoms of diabetic retinopathy and DME always obvious?
A: No. Both conditions can progress with few or no symptoms, especially in early stages. Vision changes are more common with DME due to the macula’s role in fine detail and color vision.
Q: Is treatment for diabetic retinopathy and DME painful?
A: Modern treatments like injections and laser therapy are generally quick and minimally uncomfortable. Most procedures are performed in-office and can be very effective when started early.
Summary Table: Diabetic Retinopathy vs. Diabetic Macular Edema
| Feature | Diabetic Retinopathy | Diabetic Macular Edema |
|---|---|---|
| Main Location | Retina (entire) | Macula (center of retina) |
| Main Cause | Chronic high blood sugar damages retinal vessels | Leaky vessels (from retinopathy) cause macular swelling |
| Main Symptoms | Blurry vision, floaters, poor night vision, no/little early symptoms | Blurry and wavy vision, blind spots, trouble recognizing faces |
| Diabetes Link | Can occur in both type 1 and type 2 diabetes | Almost always linked to diabetic retinopathy |
| Treatment | Blood sugar control, laser, injections, surgery | Anti-VEGF injections, steroids, laser, blood sugar control |
| Prevention | Manage diabetes, regular eye exams | Prevent progression of retinopathy and treat early |
Takeaway: Protecting Your Eyesight With Diabetes
If you live with diabetes, protecting your eyesight is within reach. Diabetic retinopathy and diabetic macular edema are serious risks, but with regular eye care, sustained blood sugar control, and prompt medical attention, vision loss can often be prevented or minimized. Stay informed, attend regular eye screenings, and work closely with your healthcare team to keep your vision clear and healthy for years to come.
References
- https://www.healthline.com/health/diabetes/diabetic-retinopathy-vs-diabetic-macular-edema
- https://www.sylvaineyecare.com/blog/diabetic-macular-edema-vs-retinopathy-spotting-the-difference-early.html
- https://www.medicalnewstoday.com/articles/diabetic-retinopathy-vs-macular-edema
- https://www.healthcentral.com/article/dme-vs-amd-whats-the-difference
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4775164/
- https://bluefinvision.com/blog/diabetic-maculopathy-vs-retinopathy-understanding-the-differences/
- https://www.shreyaeyecentre.com/diabetic-retinopathy-vs-other-diabetic-eye-diseases-know-the-difference/
- https://diabetesjournals.org/care/article/26/9/2653/22508/Diabetic-Retinopathy-and-Diabetic-Macular
Read full bio of medha deb












