Diabetic Retinopathy Fundoscopy: Examining and Managing Eye Health in Diabetes
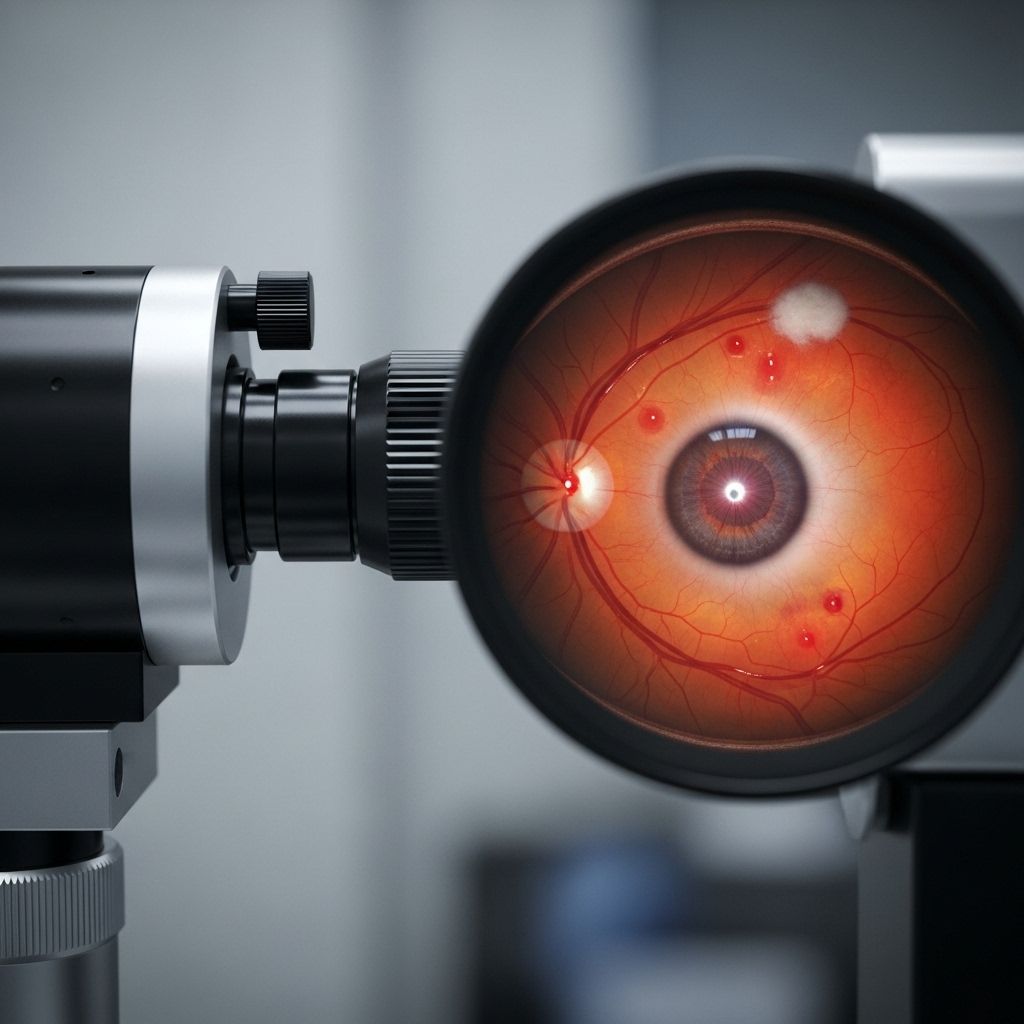
Explore how fundoscopy helps detect and manage diabetic retinopathy by identifying early retinal changes before symptoms develop.
Understanding Diabetic Retinopathy and the Role of Fundoscopy
Diabetic retinopathy is a progressive eye disease affecting people with diabetes, resulting from chronic high blood sugar levels damaging the blood vessels in the retina—the light-sensitive tissue at the back of the eye. Early detection and monitoring are crucial in preventing vision loss, and fundoscopy (also called ophthalmoscopy) is a key clinical exam for diagnosing and tracking changes in the retina. This article explains what diabetic retinopathy is, why fundoscopy is important, what to expect during the exam, and how the condition can be managed.
What is Diabetic Retinopathy?
Diabetic retinopathy is an eye condition that can develop in individuals with either type 1 or type 2 diabetes. Persistently high blood glucose levels cause damage to the tiny blood vessels (capillaries) supplying the retina, leading to:
- Leaking or bleeding blood vessels
- Swelling and inflammation in retinal tissues
- Reduced oxygen supply (ischemia) and resulting tissue damage
Without timely intervention, these changes may progress, potentially leading to vision impairment and, in severe cases, blindness.
Key Causes and Risk Factors
- Duration of diabetes: The longer someone has diabetes, the higher their risk of developing retinopathy.
- Poorly controlled blood sugar: Chronic hyperglycemia increases harm to retinal vessels.
- Hypertension: High blood pressure exacerbates vascular damage in the retina.
- High cholesterol levels
- Pregnancy (can worsen blood glucose control)
How Diabetic Retinopathy Develops
The disease typically progresses in stages:
- Nonproliferative Diabetic Retinopathy (NPDR): Early stage marked by microaneurysms (tiny bulges in blood vessels), small retinal hemorrhages (“dot and blot” bleeding), hard exudates (deposits of fat/protein), and sometimes swelling in the macula (macular edema).
- Proliferative Diabetic Retinopathy (PDR): Advanced stage featuring the growth of new, fragile blood vessels (neovascularization) on the retinal surface and sometimes into the vitreous gel. These vessels are prone to leaking and bleeding, increasing the risk of severe vision loss, retinal detachment, and neovascular glaucoma.
What is Fundoscopy?
Fundoscopy is a clinical examination where an eye doctor (ophthalmologist or optometrist) uses a special instrument called an ophthalmoscope or a fundus camera to inspect the retina, optic nerve, and blood vessels at the back of the eye. It is also known as an ophthalmoscopic exam or retinal exam. The procedure is quick, usually lasting 5–10 minutes, but may take slightly longer if dilation drops are needed.
Types of Fundoscopy
- Direct fundoscopy: The examiner holds an ophthalmoscope close to the eye and looks through the pupil at the retina.
- Indirect fundoscopy: Uses a brighter light source and a handheld lens to view the retina in greater detail, often after pupil dilation.
- Fundus photography: Specialized cameras take detailed images of the retina for record-keeping and comparison over time.
Why is Fundoscopy Important for People with Diabetes?
Fundoscopy is the primary method for detecting early signs of diabetic retinopathy before the appearance of any symptoms. Early detection through regular screening makes prompt treatment possible, reducing the risk of vision loss. Retinal changes can begin years before a patient is aware of any visual disturbance, emphasizing the importance of routine retinal exams for all individuals with diabetes.
- Early detection: Identifies early abnormalities, such as microaneurysms, hemorrhages, or swelling, that can be managed before vision is affected.
- Monitoring disease progression: Enables eye doctors to monitor for worsening changes or response to therapy.
- Guiding treatment decisions: Results help determine whether interventions like laser surgery or injection therapy are needed.
What to Expect During a Fundoscopy Exam
Fundoscopy is a straightforward, outpatient procedure performed in a clinic or eye doctor’s office. Here’s what to expect during your visit:
- History and preparation: You’ll be asked about your medical and vision history. Sometimes, eye drops are used to dilate your pupils, making it easier for the doctor to see the retina.
- Exam procedure: The doctor will shine a light into your eye while you look in specific directions. You may be asked not to blink.
- Duration: The exam itself usually takes 5–10 minutes, but you may need to wait 15–30 minutes for dilation drops to take maximum effect.
- Comfort level: Dilating eye drops can cause mild stinging and sensitivity to light. Bring sunglasses and arrange for a ride home, as your vision may be blurry for a few hours.
Findings in Diabetic Retinopathy on Fundoscopy
| Finding | Description | Associated Stage |
|---|---|---|
| Microaneurysms | Small, round outpouchings of capillaries; earliest abnormality | NPDR |
| Retinal hemorrhages | “Dot and blot” intraretinal bleeding | NPDR & PDR |
| Hard exudates | Deposits of lipid and protein with sharp borders (yellowish) | NPDR |
| Cotton-wool spots | Pale fluffy areas—microinfarcts of nerve fibers | NPDR |
| Venous changes | Venous beading, dilation, or loops | NPDR |
| Neovascularization | Abnormal new blood vessel growth | PDR |
| Vitreous hemorrhage | Blood leakage into eye’s vitreous cavity | PDR |
| Traction retinal detachment | Retina pulled off its normal position by fibrous tissue and neovascularization | PDR |
Symptoms of Diabetic Retinopathy
Many people with diabetic retinopathy experience no symptoms in the early stages. As the disease progresses, symptoms may develop, including:
- Blurry vision
- Fluctuating vision
- Floating dark spots (floaters)
- Dark or empty areas in your field of vision
- Difficulty seeing at night
- Distorted or wavy vision
- Poor peripheral (side) vision
- Difficulty perceiving colors
- Sudden, severe vision loss (in advanced cases)
It’s important to note that these symptoms can also be caused by other eye problems. Only a comprehensive eye exam can determine if diabetic retinopathy is present.
Managing Diabetic Retinopathy
Once diagnosed, the main goals are to slow disease progression, preserve vision, and prevent complications. Management strategies include:
- Blood sugar control: Tight glucose management slows progression of retinopathy.
- Blood pressure and cholesterol control: Managing these risk factors supports eye health.
- Healthy lifestyle choices: Regular exercise, a balanced diet, and smoking cessation.
- Regular eye exams: Annual or more frequent screenings are crucial for catching changes early.
In more advanced cases, additional medical or surgical interventions may be necessary:
- Anti-VEGF injections: Medications injected directly into the eye block vascular endothelial growth factor, which causes abnormal new blood vessels to grow.
- Laser photocoagulation: Seals leaking blood vessels or shrinks abnormal ones, reducing risk of bleeding.
- Vitrectomy surgery: Removes vitreous gel and blood from the eye in severe bleeding or retinal detachment.
Frequently Asked Questions (FAQs)
What causes diabetic retinopathy to progress?
Poorly controlled blood sugar, high blood pressure, high cholesterol, duration of diabetes, and certain life events such as pregnancy can all accelerate progression.
Can diabetic retinopathy be reversed?
While some newer treatments (like anti-VEGF therapy) can help regress abnormal vessels and improve vision in certain cases, most of the damage from retinopathy is not fully reversible. The focus is on slowing or stabilizing the disease.
How often should people with diabetes get a fundoscopy?
The American Diabetes Association recommends an initial dilated and comprehensive eye exam at the time of diagnosis for adults with type 2 diabetes, and within 5 years for those with type 1 diabetes, then at least annually thereafter. More frequent exams may be needed if retinopathy is detected.
What should I do if I notice vision changes?
Any new symptoms such as blurred vision, floaters, dark spots, or vision loss require immediate evaluation by an eye doctor to rule out serious complications.
Is fundoscopy uncomfortable or risky?
Fundoscopy is noninvasive and causes minimal discomfort. Some people experience temporary blurring or light sensitivity due to dilation drops.
Preventing Diabetic Retinopathy
- Keep blood sugar levels as close to target range as possible.
- Monitor blood pressure and cholesterol regularly.
- Attend all scheduled eye exams, even if your vision feels normal.
- Avoid smoking and adopt heart-healthy lifestyle habits.
- Inform your eye doctor about changes in vision, pregnancy, or new health conditions.
Key Takeaways
- Diabetic retinopathy is a common complication of diabetes that may not cause symptoms in early stages.
- Fundoscopy or ophthalmoscopy is vital for early detection, diagnosis, and monitoring of retinal changes.
- Timely diagnosis allows for prompt intervention, reducing risk of severe vision loss.
- Effective management of blood sugar, blood pressure, and cholesterol are central to prevention and treatment.
- Regular eye screenings are essential for anyone with diabetes—do not wait for symptoms to appear.
References
- https://www.merckmanuals.com/professional/eye-disorders/retinal-disorders/diabetic-retinopathy
- https://www.healthline.com/health/diabetes/diabetic-retinopathy-fundoscopy
- https://www.universityhealth.com/blog/signs-of-diabetic-retinopathy
- https://www.ncbi.nlm.nih.gov/books/NBK560805/
- https://my.clevelandclinic.org/health/diseases/8591-diabetic-retinopathy
- https://eyewiki.org/Diabetic_Retinopathy
- https://geekymedics.com/fundoscopic-appearances-of-retinal-pathologies/
Read full bio of Sneha Tete












