Diabetic Neurogenic Bladder: Symptoms, Causes, Diagnosis & Treatment
Explore how diabetes affects bladder control, key symptoms, underlying causes, diagnosis, complications, and modern management strategies.
Diabetic Neurogenic Bladder: Overview, Symptoms, Causes, Diagnosis & Treatment
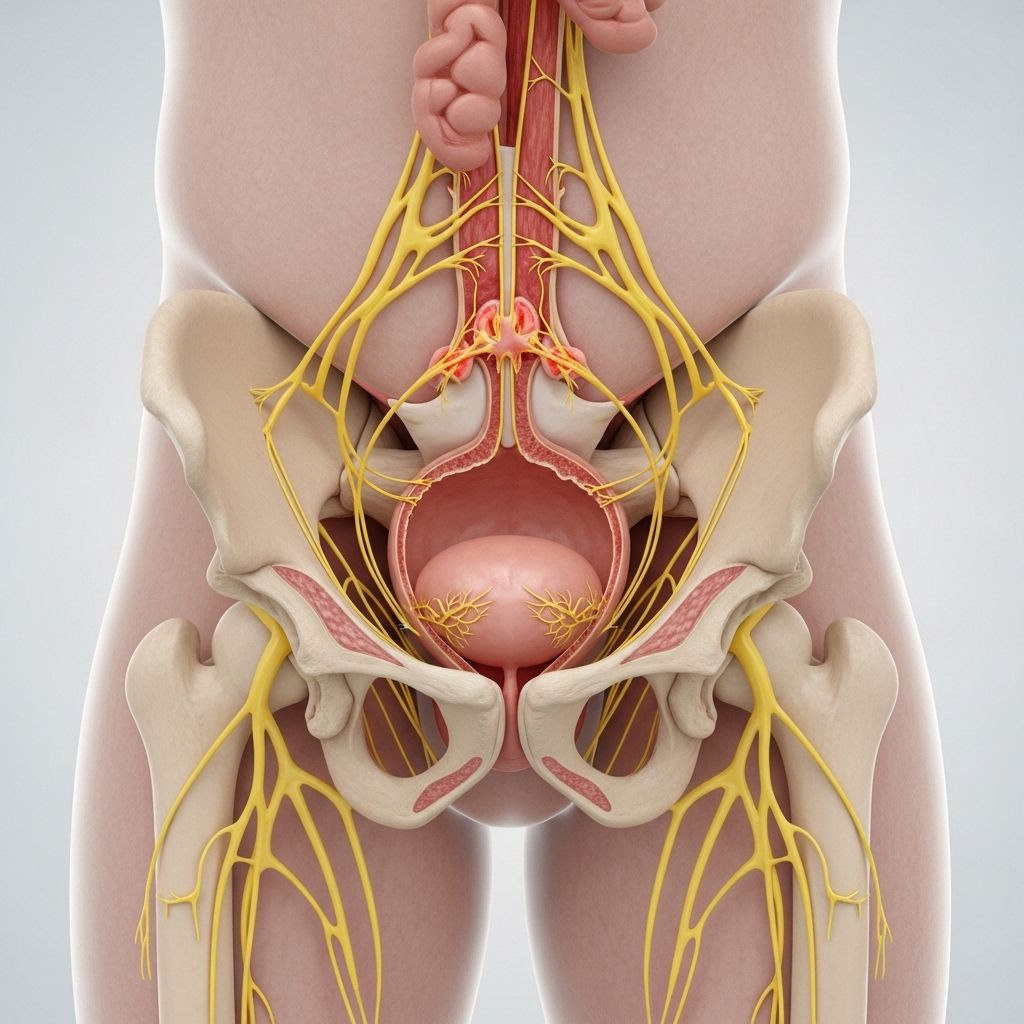
Diabetic neurogenic bladder is a condition caused by nerve damage stemming from diabetes, resulting in impaired bladder control. This article comprehensively covers its symptoms, causes, risk factors, diagnosis, complications, and treatment options.
What Is Diabetic Neurogenic Bladder?
Neurogenic bladder refers to bladder dysfunction resulting from impaired nerve signaling between the brain, spinal cord, and bladder muscles. In diabetes, chronic high blood sugar can damage nerves—a condition known as diabetic neuropathy. Neurogenic bladder is categorized by the inability to sense a full bladder, problems emptying, or a loss of voluntary control over urination.
How Diabetes Leads to Bladder Problems
- Persistently high blood sugar can damage the autonomic nerves supplying the bladder.
- This affects communication between the bladder muscles and the brain.
- Neuropathy results in loss of sensation, abnormal contraction, or incomplete emptying.
Symptoms of Diabetic Neurogenic Bladder
Symptoms vary depending on whether the bladder is overactive, underactive, or both. The severity and nature of nerve damage guide clinical presentation.
Common Symptoms
- Frequent urination in small amounts, often more than eight times per day.
- Urgency—a sudden, intense need to urinate.
- Difficulty starting urination or feeling of incomplete emptying.
- Incontinence—leakage or loss of bladder control.
- Urinary retention—inability to empty the bladder fully, leading to buildup and leakage.
- Loss of sensation—not feeling when the bladder is full.
If not managed, chronic retention can cause frequent urinary tract infections (UTIs), which may progress to kidney damage over time.
Causes of Neurogenic Bladder in Diabetes
The primary cause is diabetic neuropathy—nerve damage due to persistent hyperglycemia.
Other Contributing Causes
- Spinal cord injury
- Multiple sclerosis and other neurological disorders
- Stroke
- Pelvic trauma or surgery
- Vitamin B12 deficiency
- Heavy metal poisoning
- Alcohol abuse
However, among these, diabetes-induced nerve damage is the most common cause in people with diabetes.
Risk Factors
- Poorly controlled diabetes (prolonged high blood sugar levels)
- Long-standing diabetes (many years with the condition)
- Other diabetic complications (retinopathy, nephropathy, peripheral neuropathy)
- Older age
- Family history of neuropathy
- Lifestyle factors (sedentary lifestyle, smoking, excess alcohol use)
Complications Associated with Diabetic Neurogenic Bladder
Unmanaged neurogenic bladder can lead to several significant health challenges:
- Urinary Tract Infections (UTIs): Retained urine creates a breeding ground for bacteria.
- Kidney Damage: Chronic bladder retention can back up into the kidneys, causing infection or failure.
- Incontinence: Social, mental, and physical effects due to uncontrolled urine leakage.
- Bladder Stones: Stagnant urine increases stone formation risk.
- Skin Irritation: From constant wetness in the genital area.
Diagnosis of Diabetic Neurogenic Bladder
Early diagnosis prevents complications and improves outcomes. Diagnosis starts with a thorough clinical evaluation and may require specialized tests.
| Diagnostic Tool | Description |
|---|---|
| Medical history & symptom review | Discuss pattern, frequency, urgency, leakage, and sensation changes. |
| Physical examination | Includes neurological assessment. |
| Urinalysis/Urin Culture | Screens for infection and blood in urine. |
| Bladder diary (voiding diary) | Tracks frequency, volume, and triggers over several days. |
| Post-void residual measurement | Ultrasound or catheterization to measure retained urine. |
| Urodynamic studies | Assess bladder function and nerve responses. |
| Imaging tests | Ultrasound, CT, or MRI to evaluate anatomy. |
What to Expect During Diagnosis
- Comprehensive symptom review and medical history
- Possible referral to urologists or neurologists for specialized testing
- Bladder function assessment—timed voiding, post-void residuals
Treatment Options for Diabetic Neurogenic Bladder
Management focuses on symptom control, reducing risk of complications, and improving quality of life.
Non-Pharmacologic Treatments
- Lifestyle modifications:
- Scheduled voiding (timed urination)
- Fluid management (monitoring intake)
- Dietary adjustments (reducing bladder irritants)
- Bladder diary to identify patterns
- Pelvic floor exercises (Kegels) to strengthen bladder control
- Monitoring and managing blood glucose: Optimal diabetes control can reduce progression.
Medications
- Anticholinergics: Reduce bladder contractions in overactive bladder cases.
- Beta-3 adrenergic agonists: Relax bladder muscle and alleviate urgency.
- Alpha-blockers: Aid in relaxing the bladder neck for easier emptying.
Procedural Interventions
- Catheterization: For underactive bladder or significant retention. Includes intermittent and indwelling options.
- Botulinum toxin (Botox) injection: Used in some cases to relax an overactive bladder muscle.
- Nerve stimulation therapy: Procedures such as sacral neuromodulation may help bladder nerve function.
- Surgery: Reserved for severe, refractory cases—eg. bladder augmentation or sphincter implantation.
Prevention and Self-management
- Maintain target blood glucose levels with diet, exercise, and medication.
- Address risk factors such as hypertension, obesity, and smoking.
- Regular monitoring of urinary symptoms and kidney function.
- Early consultation with healthcare provider for new or worsening urinary symptoms.
Living with Diabetic Neurogenic Bladder
Adjusting to daily life with neurogenic bladder involves education, proactive management, and support from healthcare professionals and peers.
- Bladder management plans tailored to individual needs.
- Communication with healthcare providers to monitor for complications.
- Utilizing community support groups for emotional and practical assistance.
- Adhering to diabetes care reduces risk of further complications.
Frequently Asked Questions (FAQs)
What is the main cause of neurogenic bladder in people with diabetes?
Nerve damage from poorly controlled blood glucose levels (diabetic neuropathy) is the main cause of neurogenic bladder in diabetes.
Can diabetic neurogenic bladder be cured?
Neurogenic bladder is typically a chronic condition. Managing diabetes and using targeted treatments can prevent progression and reduce symptoms.
What are the signs that I may have diabetic neurogenic bladder?
Common signs include difficulty emptying the bladder, frequent urination in small amounts, urgency, loss of bladder control, and urinary retention.
How can I prevent bladder complications from diabetes?
Effective blood glucose management, routine urinary symptom monitoring, and prompt treatment of infections can help prevent complications.
Are there support groups or resources available?
Many diabetic and urologic organizations offer education and support. Ask your healthcare provider for recommendations.
Key Takeaways
- Diabetic neurogenic bladder results from nerve damage due to diabetes
- Early symptom recognition is essential for preventing complications
- Lifestyle changes and medical interventions can significantly improve quality of life
- Close management of diabetes is critical in prevention and treatment
If you suspect bladder problems related to diabetes, consult your healthcare provider as early management leads to the best outcomes.
References
- https://www.diabetes.co.uk/diabetes-complications/neurogenic-bladder.html
- https://nafc.org/bhealth-blog/the-link-between-diabetes-and-neurogenic-bladder/
- https://www.wellspect.us/bladder-and-bowel-dysfunction/diabetes/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3153010/
- https://my.clevelandclinic.org/health/diseases/15133-neurogenic-bladder
- https://www.urologyhealth.org/urology-a-z/n/neurogenic-bladder
- https://www.hopkinsguides.com/hopkins/view/Johns_Hopkins_Diabetes_Guide/547019/all/Bladder_Disorders_in_Diabetes
- https://www.bladderandbowel.org/associated-illness/diabetes-incontinence/
Read full bio of medha deb












