Diabetic Nephropathy: Symptoms, Diagnosis, and Treatment
Understand the signs, causes, diagnosis, and management strategies for diabetic nephropathy, a leading complication of diabetes.
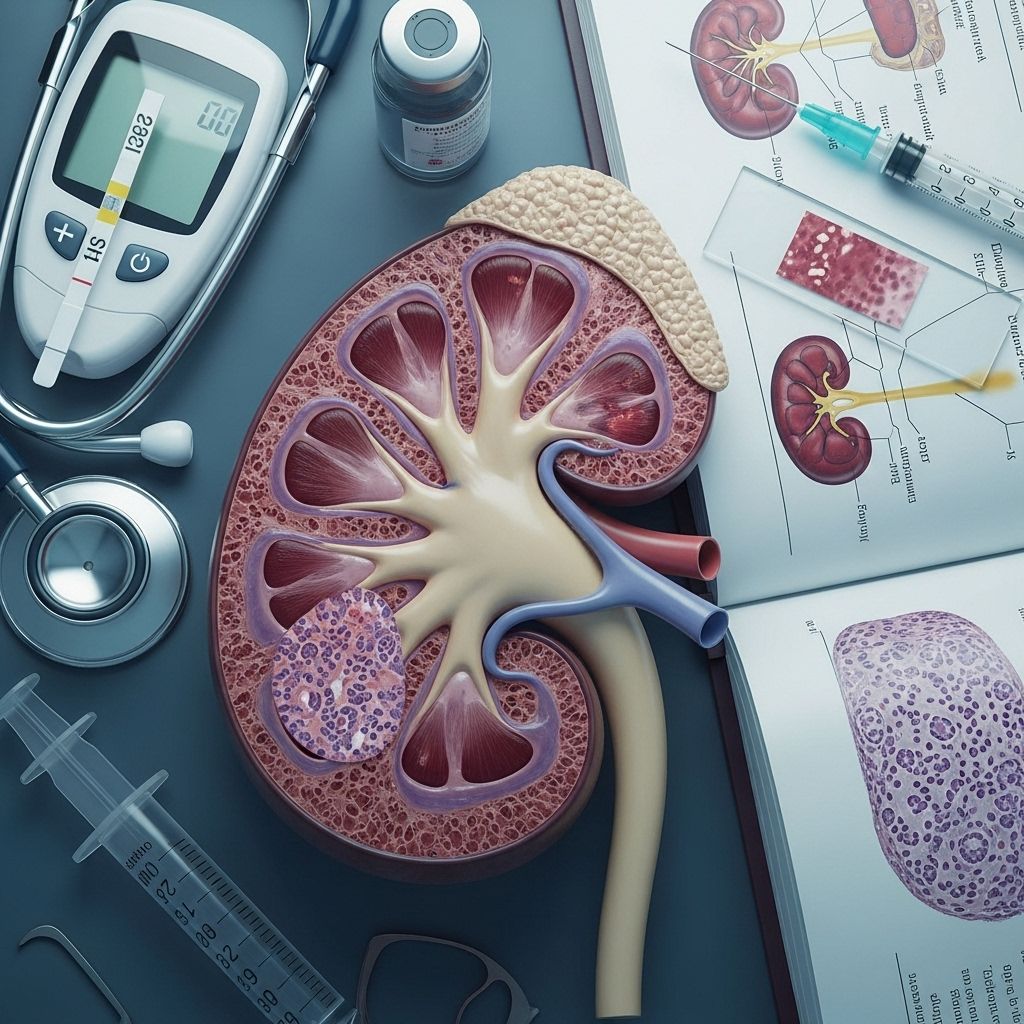
Diabetic nephropathy is a form of chronic kidney disease that develops as a complication of diabetes mellitus. Characterized by damage to the small blood vessels in the kidneys, it compromises their ability to remove waste and excess fluid from the body. With the prevalence of diabetes rising worldwide, understanding the early signs, diagnostic strategies, risk factors, and treatment options for diabetic nephropathy is critical for prevention and effective management.
What Is Diabetic Nephropathy?
Diabetic nephropathy is a progressive kidney disease caused by prolonged high blood sugar levels from diabetes, resulting in damage to the glomeruli — the filtering units in the kidneys. Over time, this leads to protein leaking into the urine (proteinuria), loss of kidney function, and eventually, kidney failure if left untreated. Both type 1 and type 2 diabetes can lead to diabetic nephropathy, but not everyone with diabetes will develop this complication.
Early Symptoms of Diabetic Nephropathy
In the initial stages, diabetic nephropathy may not cause noticeable symptoms. The early damage can only be detected through laboratory testing. As the disease advances, several symptoms may develop:
- Protein in the urine (proteinuria): Often the first clinical sign, detected before noticeable symptoms appear.
- Swelling (edema): Swelling in the hands, feet, ankles, or around the eyes due to fluid retention.
- Increased need to urinate: Especially at night (nocturia), as the kidneys lose filtering ability.
- High blood pressure: Worsening hypertension due to kidney impairment.
- Fatigue and weakness: Resulting from the build-up of waste and imbalance of minerals in the blood.
- Nausea or vomiting: Particularly as kidney function deteriorates.
- Poor appetite and unintended weight loss
- Difficulty concentrating: Due to toxin build-up affecting brain function.
- Persistent itching: Waste accumulation in the blood can lead to skin irritation.
Because symptoms often do not appear until significant kidney damage has occurred, routine screening is crucial for people with diabetes.
Stages of Diabetic Nephropathy
Diabetic nephropathy develops gradually and can be classified into the following stages:
- Stage 1: Hyperfiltration — kidneys work harder but may still function normally.
- Stage 2: Microalbuminuria — small amounts of albumin (protein) are detected in urine.
- Stage 3: Macroalbuminuria (overt nephropathy) — large amounts of protein present in urine, blood pressure increases.
- Stage 4: Advanced kidney damage — reduced kidney function, high blood pressure, and swelling.
- Stage 5: End-stage renal disease (ESRD) — kidneys fail, requiring dialysis or transplantation.
Causes and Risk Factors
Diabetic nephropathy results primarily from chronically high blood sugar levels damaging kidney blood vessels. Several other risk factors influence its development and progression:
- Poor blood glucose control: Uncontrolled diabetes is the leading cause.
- High blood pressure: Accelerates kidney injury.
- Duration of diabetes: Risk increases with the number of years spent living with diabetes.
- Family history: Genetics plays a role; a family history of diabetes or kidney disease increases risk.
- Smoking: Further damages blood vessels and increases risk.
- Obesity: Can worsen diabetes and hypertension, thus impacting kidneys.
- High cholesterol: Exacerbates vascular and kidney damage.
- Ethnicity: African American, Hispanic, Native American, and Asian American individuals may have a higher risk.
| Risk Factor | Impact |
|---|---|
| Poor Blood Sugar Control | Directly causes kidney vessel damage |
| High Blood Pressure | Speeds up kidney decline |
| Long-standing Diabetes | Risk rises with disease duration |
| Genetics/Family History | Higher risk if relatives are affected |
| Smoking | Exacerbates vascular damage |
| Obesity and High Cholesterol | Increase the workload and strain on kidneys |
How is Diabetic Nephropathy Diagnosed?
Diagnosing diabetic nephropathy involves multiple steps to assess kidney function and identify early changes.
- Urine tests: The annual screening test is measurement of albumin-to-creatinine ratio (ACR) — a high ratio suggests protein leakage from kidney damage.
- Blood tests: Assess glomerular filtration rate (GFR) by measuring waste products (such as creatinine) in the blood to estimate how well kidneys filter blood.
- Blood pressure measurement: Regular monitoring, since hypertension commonly accompanies kidney impairment.
- Additional tests: In some cases, kidney ultrasound or biopsy may be required to rule out other causes or confirm diagnosis.
People with diabetes are advised to have their urine checked for protein at least once a year, as early detection dramatically improves outcomes.
Prevention and Early Intervention
Prevention hinges on tight control of blood glucose and blood pressure. Actions to lower the risk of diabetic nephropathy include:
- Adhering strictly to diabetes medication regimens
- Maintaining hemoglobin A1c within target ranges
- Controlling blood pressure (usually aiming for <130/80 mm Hg)
- Limiting dietary salt and unhealthy fats
- Not smoking
- Maintaining a healthy weight through diet and exercise
- Regular monitoring of kidney function, especially in those with diabetes
Treatment Options for Diabetic Nephropathy
There is no cure for diabetic nephropathy, but early treatment can significantly slow disease progression, reduce complications, and preserve kidney function.
Glycemic Control
Maintaining blood sugar levels within the recommended range is the cornerstone of prevention and management. This may involve:
- Consistent use of insulin or oral diabetes medications as prescribed
- Frequent monitoring of blood glucose
- Adopting carbohydrate-counting and healthy eating strategies
Blood Pressure Management
- Strict blood pressure control is essential (target often <130/80 mm Hg)
- ACE inhibitors (ramipril, lisinopril, etc.) and angiotensin receptor blockers (ARBs) (losartan, valsartan) are often used—these medications offer kidney protection even in people without hypertension
- Other antihypertensive agents as needed
Cholesterol and Lipid Control
- Statins and other cholesterol-lowering medications may reduce additional vascular strain and slow progression of kidney damage
Medications Specific to Diabetic Nephropathy
- SGLT2 inhibitors (e.g., empagliflozin, dapagliflozin) lower blood sugar and protect kidney function
- GLP-1 receptor agonists (e.g., liraglutide, semaglutide) support glycemic and cardiovascular health
- Finerenone (Kerendia): a specialized medication that reduces kidney scarring and failure risk in type 2 diabetes-associated CKD
Dietary and Lifestyle Adjustments
- Limiting protein intake to reduce kidney strain (as recommended by your healthcare team)
- Reducing sodium (salt) intake to help manage blood pressure and reduce swelling
- Limiting foods high in potassium and phosphorus if advised (such as bananas, avocados, dairy, and processed meats)
- Choosing healthy fats and avoiding saturated/trans fats
- Staying physically active within safe limits
- Quitting smoking and moderating alcohol intake
Advanced Kidney Care
If diabetic nephropathy progresses to advanced or end-stage kidney disease, more intensive interventions may be required:
- Dialysis: Mechanical removal of toxins and excess fluid when kidneys can no longer function adequately
- Kidney transplant: A healthy kidney from a donor may be needed for long-term survival
Living with Diabetic Nephropathy
Living with diabetic nephropathy involves careful management of diabetes, kidney health, and overall wellness. Important recommendations include:
- Adhering to prescribed medications and dietary recommendations
- Keeping all scheduled appointments and laboratory tests
- Monitoring blood glucose and blood pressure at home
- Reporting new or worsening symptoms promptly
- Seeking support from diabetes educators, nutritionists, and kidney specialists
Complications of Diabetic Nephropathy
- Persistent or worsening high blood pressure
- Hyperkalemia: High blood potassium
- Fluid retention: Swelling in extremities, lungs, or around eyes
- Cardiovascular disease: Higher risk of heart attack, stroke, and heart failure
- End-stage renal disease (ESRD): Requiring dialysis or transplantation
- Anemia: As kidneys produce less erythropoietin, leading to low red blood cell count
Frequently Asked Questions (FAQs)
What is the earliest sign of diabetic nephropathy?
The earliest detectable sign is usually the presence of small amounts of protein (microalbuminuria) in the urine, which often causes no obvious symptoms.
Can diabetic nephropathy be reversed?
There is no known cure or reversal, but with prompt intervention and ongoing disease management, progression can be slowed or, in some cases, halted.
How often should people with diabetes be screened for kidney disease?
Annual urine and blood tests are the standard recommendation for all people with diabetes, or more frequently if risk factors are present or early abnormalities are detected.
What role does diet play in kidney health for diabetics?
A kidney-friendly diet can ease the burden on the kidneys, limit further damage, and help manage blood sugar and pressure; common recommendations include modest protein intake, reduced sodium, and limited high-potassium and high-phosphorus foods.
What should be done if kidney function continues to decline?
If kidney function drops despite optimal blood sugar and blood pressure control, referral to a nephrologist is vital for specialized care, and discussions about dialysis or transplantation may be needed.
Additional Resources
- American Diabetes Association: Living with Diabetes and Kidney Disease
- National Kidney Foundation: Kidney Disease in Diabetes
- Consult your healthcare provider for up-to-date and personalized medical advice
References
- https://www.mayoclinic.org/diseases-conditions/diabetic-nephropathy/diagnosis-treatment/drc-20354562
- https://www.webmd.com/diabetes/diabetes-kidney-disease
- https://www.healthline.com/health/type-2-diabetes/nephropathy
- https://www.ncbi.nlm.nih.gov/books/NBK534200/
- https://www.mayoclinic.org/diseases-conditions/diabetic-nephropathy/symptoms-causes/syc-20354556
- https://www.aafp.org/pubs/afp/issues/2019/0615/p751.html
- https://www.medicalnewstoday.com/articles/319686
- https://phoenixchildrens.org/specialties-conditions/diabetic-nephropathy-kidney-disease
Read full bio of Sneha Tete












