Diabetic Macular Edema: Symptoms, Causes, Treatment & Vision Tips
Comprehensive guide to diabetic macular edema: causes, symptoms, diagnosis, treatment strategies, and living well with vision changes.
Diabetic Macular Edema (DME) is a serious eye condition that directly threatens your central vision, primarily affecting individuals with diabetes. Timely recognition and medical intervention are crucial to prevent vision deterioration or even blindness. This comprehensive guide will help you understand DME, its risk factors, how it’s diagnosed, all current treatment options, and how to maintain the best possible quality of life when living with this condition.
What Is Diabetic Macular Edema?
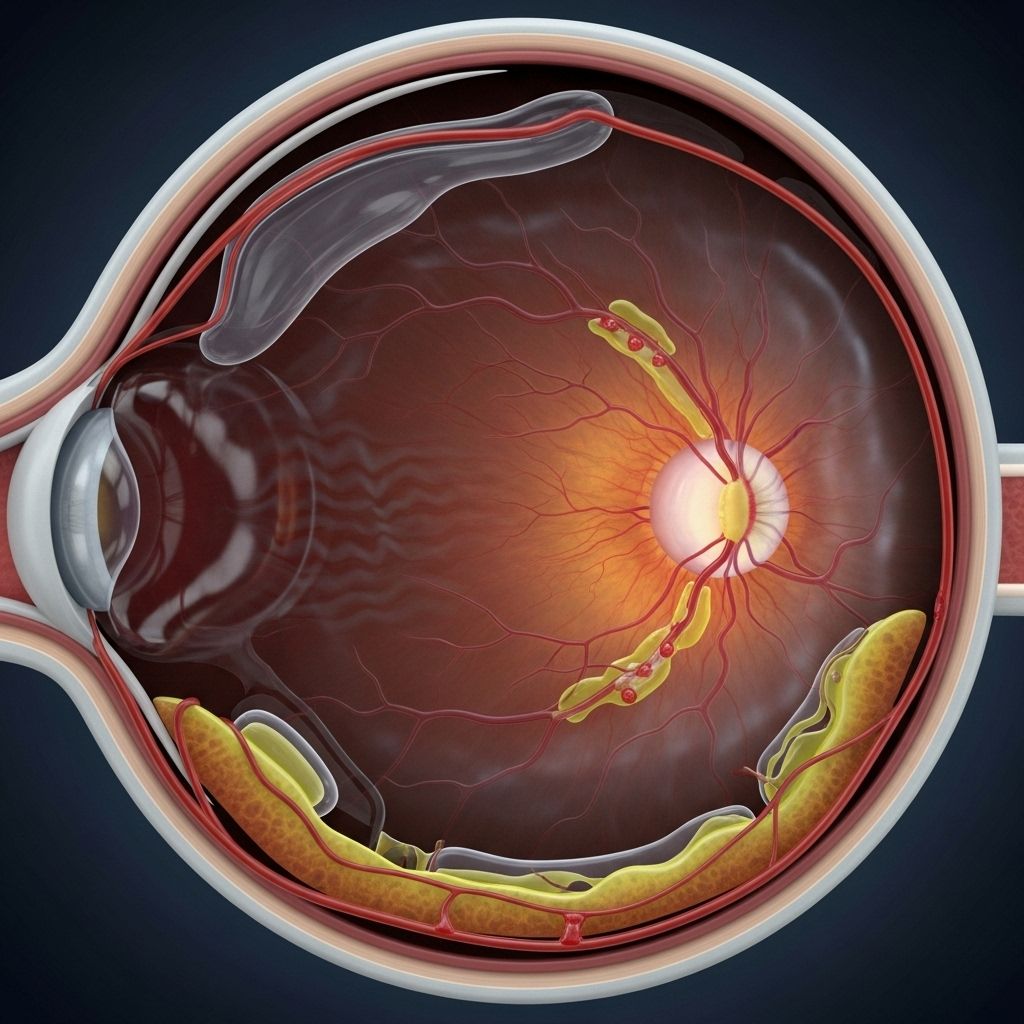
Diabetic Macular Edema (DME) is a condition where fluid accumulates in the macula, the central part of the retina responsible for sharp, straight-ahead vision. This swelling occurs because diabetes can damage the blood vessels in the retina, causing them to leak fluid and proteins into the macula. The result is thickening, swelling, and subsequently impaired vision.
- DME is a leading cause of vision loss among people with type 1 and type 2 diabetes.
- It most often develops as part of diabetic retinopathy, the broader term for diabetes-induced retinal damage.
- The risk increases with the duration of diabetes and poor blood sugar control.
Symptoms of Diabetic Macular Edema
DME often develops silently, with mild symptoms at first, sometimes going unnoticed until vision is significantly affected. Early detection is vital, as prompt treatment can help preserve eyesight.
- Blurry vision or difficulty seeing details, especially for reading or recognizing faces.
- Objects in the center of vision may appear wavy or distorted.
- Colors may look faded or less vibrant than usual.
- Vision might be doubled or intermittently fluctuate in quality.
- Dark spots or “floaters” may appear in your field of vision.
- Symptoms can be worse in one eye, or appear in both.
Note: DME can progress to significant vision impairment or blindness if left untreated. Regular eye exams for people with diabetes are crucial even if vision seems normal.
What Causes Diabetic Macular Edema?
The driving force behind DME is chronic high blood sugar (hyperglycemia), which damages the tiny blood vessels in the retina. Over time, this damage makes vessels leak fluid into the macula. Several other factors can heighten this risk:
- High blood pressure (hypertension)
- High cholesterol levels
- Long duration of diabetes
- Kidney disease
DME is one consequence of diabetic retinopathy. As the disease advances, more abnormal blood vessels form and leak, exacerbating the swelling in the macula. DME is not just limited to people with longstanding diabetes; it can occasionally develop earlier, especially if blood sugar is poorly controlled.
Risk Factors for Diabetic Macular Edema
Certain groups and conditions increase your likelihood of developing DME:
- Duration of diabetes – risk rises as time goes on
- Poor blood sugar control
- Presence of diabetic retinopathy (especially moderate to severe)
- High blood pressure and cholesterol
- Pre-existing kidney disease
- Pregnancy
- Previous eye surgery or trauma
How Is Diabetic Macular Edema Diagnosed?
Prompt and accurate diagnosis is essential to managing DME. If you have diabetes, your doctor or an eye specialist will use a variety of tests:
- Dilated Eye Exam: Drops are used to enlarge your pupils, allowing direct visualization of the retina.
- Optical Coherence Tomography (OCT): This imaging technique creates a cross-sectional image of the retina, letting doctors see the presence and amount of swelling in the macula.
- Fluorescein Angiography: A special dye is injected into your bloodstream and images are captured to reveal leaking retinal blood vessels.
- Visual acuity tests and other assessments may help determine the severity of vision loss.
Early diagnosis not only helps preserve vision but also guides treatment choices.
How Is Diabetic Macular Edema Treated?
While there is no cure for DME, a range of effective treatments exist to reduce swelling, prevent further vision loss, and, in some cases, restore partial vision. The best approach is customized to each individual based on disease severity, overall health, and personal needs.
Medical Management of Underlying Conditions
- Controlling blood sugar close to normal can prevent DME from worsening.
- Managing high blood pressure and cholesterol can further protect your vision.
- Lifestyle improvements (such as healthy eating, regular exercise, and consistent diabetes management) support all additional treatments.
Targeted Ophthalmic Treatments
Anti-VEGF Injections
A breakthrough in DME therapy, anti-VEGF (vascular endothelial growth factor) medications target and block the protein responsible for abnormal vessel growth and leakage. The medication is injected directly into the eye after numbing drops are applied for comfort. This helps stabilize, and sometimes improve, vision.
- Common anti-VEGF drugs: Aflibercept (Eylea), Bevacizumab (Avastin), Brolucizumab-dbll (Beovu), Ranibizumab (Lucentis)
- Some newer medications can target additional vessel growth proteins (e.g., Faricimab-svoa [Vabysmo] targets both VEGF and Angiopoietin-2).
- Frequency: Typically one injection per month for the first 4–6 months, followed by reduced frequency as the eye stabilizes.
- Effectiveness: Not all individuals respond equally, and not all drugs are suitable for everyone (e.g., some should be avoided in pregnancy).
Focal Laser Therapy
Longstanding but still valuable in certain cases, focal or grid laser therapy uses directed laser light to seal or destroy leaking blood vessels in the retina. While it may leave minor permanent blind spots, it helps slow the progression of vision loss and preserves remaining vision when anti-VEGF therapies are insufficient or not tolerated.
Corticosteroids
Steroid injections or slow-release steroid implants placed in the eye can help reduce macular swelling in certain forms of DME. Corticosteroids may be used alone or in combination with other treatments, particularly when anti-VEGF therapy is not effective or contraindicated. Potential side effects (elevated eye pressure, cataract formation) require careful monitoring by your specialist.
Other Supportive Measures
- Low vision aids (magnifying glasses, telescopic lenses, special lamps, large-print reading materials, etc.) help individuals adapt to vision loss and maintain independence.
- Vision rehabilitation specialists can teach adaptive skills to maximize daily function.
Treatment Comparison Table
| Treatment | Method | Main Benefit | Common Side Effects / Limitations |
|---|---|---|---|
| Anti-VEGF Injections | Drug injected into eye | Reduces swelling, can restore some vision | Discomfort at injection site, requires frequent visits |
| Focal Laser Therapy | Laser application to retina | Slows further vision loss | Possible small permanent blind spots |
| Corticosteroids | Injection/implant in eye | Reduces swelling, especially in some cases where anti-VEGF not suitable | Risk of cataracts, increased eye pressure |
| Low Vision Aids | Devices, technology, training | Improves quality of life, independence | Does not restore vision, adaptation required |
Complications and Long-Term Outlook
If left untreated, diabetic macular edema can cause progressive central vision loss and even permanent blindness. However, with prompt diagnosis and modern treatment options, many people retain functional vision. Proper disease management and regular monitoring are essential to prevent relapses or progression.
Preventing Diabetic Macular Edema
- Carefully manage your blood sugar through medication, diet, and lifestyle.
- Monitor and control your blood pressure and cholesterol through regular check-ups and medications if needed.
- Attend annual comprehensive dilated eye exams – more frequent evaluations if you already have diabetic eye disease.
- Follow your diabetes treatment regimen consistently and promptly report any vision changes to your healthcare provider.
Awareness and early intervention are crucial to preserving your sight.
Living Well with Diabetic Macular Edema
Vision loss can feel overwhelming, but with proper tools, support, and training, most people can maintain active, independent lives.
Low Vision Rehabilitation
Vision rehabilitation specialists and occupational therapists can teach adaptive strategies and recommend practical aids:
- Magnifiers for reading and daily tasks
- Improved lighting in living and working spaces
- Contrast-enhanced materials (bold print, high-contrast colors)
- Audio books, voice-activated computers, and screen readers
- Orientation and mobility training for navigation
Support groups and patient organizations can provide community and emotional support during adjustment.
Frequently Asked Questions (FAQs)
What is diabetic macular edema, and how does it differ from diabetic retinopathy?
Diabetic macular edema is a specific complication of diabetic retinopathy where swelling from leaking blood vessels occurs in the macula, the center of the retina responsible for sharp vision. While diabetic retinopathy is general retinal damage from diabetes, DME specifically causes central vision loss and distortion.
Who is at risk for developing DME?
People with any type of diabetes (type 1, type 2, or gestational) are at risk, especially if they’ve had diabetes for many years, have poor blood sugar control, high blood pressure, or existing diabetic retinopathy.
Can diabetic macular edema be cured?
There is no cure, but with medical and ophthalmic management, the swelling can often be reduced or stabilized, preserving – and sometimes partially restoring – vision.
Do anti-VEGF injections hurt?
Most patients experience only minor discomfort, as the eye is thoroughly numbed before the injection. Some may feel pressure or a mild sting. Your eye doctor will make the experience as comfortable as possible.
Can I still drive or work after a diagnosis of DME?
It depends on the severity of your vision loss. With proper treatment, many maintain enough vision for everyday tasks, but you may need special assessments or rehabilitation support to help adapt.
References
- Information adapted from the National Eye Institute, Prevent Blindness, WebMD, and Cleveland Clinic eye health resources.
References
- https://www.webmd.com/diabetes/diabetic-macular-edema-treatment
- https://www.elmanretina.com/services/treatments-and-services/diabetic-macular-edema/
- https://preventblindness.org/diabetic-macular-edema-dme/
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/macular-edema
- https://my.clevelandclinic.org/health/diseases/24733-diabetes-related-macular-edema
- https://www.macularsociety.org/macular-disease/macular-conditions/diabetic-macular-oedema/
- https://www.mayoclinic.org/diseases-conditions/diabetic-retinopathy/multimedia/diabetic-macular-edema/img-20124558
- https://www.mdfoundation.com.au/about-macular-disease/diabetic-eye-disease/about-diabetic-macular-oedema/
- https://www.mayoclinic.org/diseases-conditions/diabetic-retinopathy/symptoms-causes/syc-20371611
Read full bio of medha deb












