Essential Resources for Managing Diabetic Macular Edema
Comprehensive guide to diabetic macular edema, including symptoms, causes, treatment options, and lifestyle resources for patients.
Understanding Diabetic Macular Edema (DME)
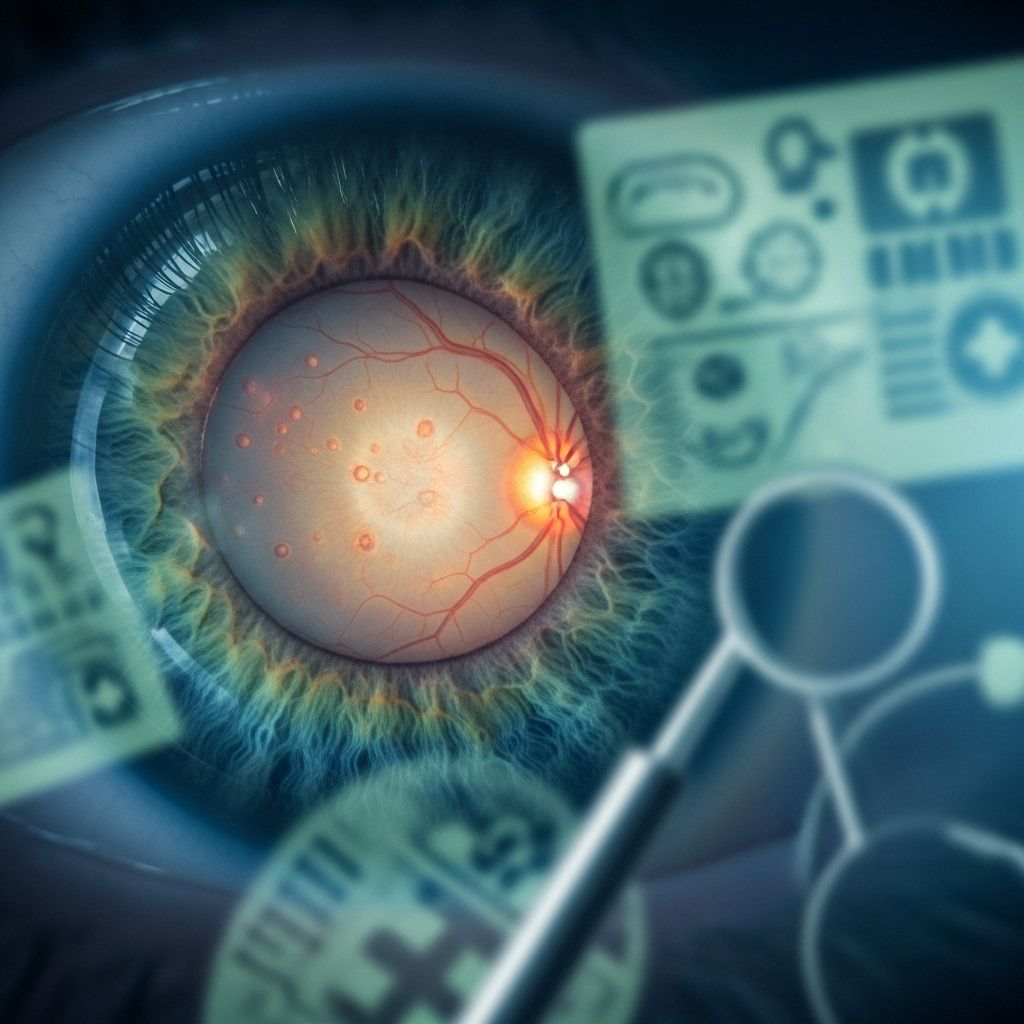
Diabetic macular edema (DME) is a serious eye condition that primarily affects individuals with diabetes. Characterized by swelling in the macula—the central region of the retina responsible for sharp, straight-ahead vision—DME is a leading cause of visual impairment and blindness among people living with diabetes.
This disease can have a profound impact on daily life, causing blurry vision, image distortion, faded colors, and even dark spots or floaters. These symptoms may hinder essential tasks such as reading, driving, taking medications, working, and maintaining independence.
Prevalence and Importance of Early Detection
DME affects approximately 10% of the 7.7 million Americans with diabetes, making it a major public health issue. Regular, comprehensive eye exams are crucial for early detection and effective management. Many people with diabetes may not notice swelling in their retina; only an eye care specialist can detect DME through a detailed examination.
Common Symptoms of DME
- Blurry or wavy central vision
- Faded or dull colors
- Floaters or dark spots
- Difficulty with visual tasks (e.g., reading, driving)
It’s important to seek prompt medical attention if these symptoms occur, as untreated DME can lead to permanent vision loss and even legal blindness.
Causes and Risk Factors of Diabetic Macular Edema
The primary cause of DME is chronic high blood sugar levels, which damage the tiny blood vessels in the retina. When these vessels weaken, they leak fluid into the retina, resulting in swelling and impairment of the macula’s function.
Additional risk factors include:
- Hypertension: High blood pressure increases leakage and swelling.
- Duration of diabetes: Longer-term diabetes raises risk.
- Diabetic retinopathy: Progressive eye disease linked to uncontrolled diabetes.
- Inflammation and vascular dysfunction: Involvement of proteins such as VEGF and Ang-2, along with inflammatory chemokines and cytokines.
Pathophysiology Overview
- Damage to the blood-retina barrier allows fluid to accumulate within and underneath retinal layers.
- VEGF and other mediators—such as interleukins, matrix metalloproteinases, and TNF—contribute to inflammation, oxidative stress, and vascular changes.
- Changes occur in the neurovascular unit, disrupting retinal homeostasis.
Diagnosis and Monitoring of DME
Regular eye examinations are essential for the detection and monitoring of diabetic macular edema. If any symptoms of visual impairment arise, patients should immediately consult a retina specialist.
- Comprehensive Eye Exam: Includes visual acuity tests, dilated fundus examination, and retinal imaging (such as optical coherence tomography and fluorescein angiography).
- Assessment of Severity: Ophthalmologists evaluate the extent of leakage, thickness of the macula, and associated retinal changes to classify DME and guide treatment.
Consistent follow-ups are necessary to monitor disease progression and response to therapy.
Treatment Options for Diabetic Macular Edema
While there is currently no cure for DME, various treatments can reverse or slow disease progression, reduce symptoms, and preserve vision.
Controlling Underlying Conditions
- Blood Sugar Management: Keeping glucose levels close to normal is fundamental to prevent or slow eye damage.
- Blood Pressure Control: Maintaining healthy blood pressure reduces retinal vessel leakage.
Pharmacological Treatments
Anti-VEGF Therapy
Anti-VEGF medications block the vascular endothelial growth factor protein, stabilizing and preventing abnormal blood vessel growth and leakage in the retina.
| Anti-VEGF Medicine | Brand Name | Duration & Effect |
|---|---|---|
| Aflibercept | Eylea | Monthly injection, effective for severe vision loss. |
| Bevacizumab | Avastin | Monthly injection, commonly used for various DME cases. |
| Brolucizumab-dbll | Beovu | Monthly injection, newer agent targeting VEGF. |
| Ranibizumab | Lucentis | Monthly injection, standard anti-VEGF treatment. |
- Usually administered as a painless injection into the eye, after numbing drops.
- Typical schedule: One shot a month for first 4-6 months, then less frequent over time.
VEGF/Ang-2 Inhibitors
- Faricimab-svoa (Vabysmo): Blocks both VEGF and Ang-2 proteins, may last longer than standard anti-VEGF agents, stabilizes fragile blood vessels.
Steroid Therapy
- Corticosteroid injections or implants may be used for inflammation-related DME or when anti-VEGF therapy is ineffective.
Laser Photocoagulation
Laser treatment has traditionally been used to seal leaking blood vessels and prevent further fluid accumulation.
- Focal photocoagulation: Directly targets leaking areas in the retina.
- Reduces risk of severe vision loss but rarely restores lost vision.
Surgical Options
- Vitrectomy: Removal of vitreous gel to improve access to the retina may be considered in select cases (often when hemorrhage or severe disease present).
Managing Diabetes for Eye Health
- Adhere to prescribed medications and insulin routine.
- Maintain a balanced, healthy diet (focus on low-glycemic foods, fruits, vegetables).
- Exercise regularly to improve overall vascular health.
- Quit smoking and minimize exposure to secondhand smoke.
Involvement of a multidisciplinary team—including endocrinologists, ophthalmologists, and nutritionists—is ideal for comprehensive management.
Living with Diabetic Macular Edema
Receiving a diagnosis of DME may be overwhelming, but with proper treatment and support, many individuals maintain their quality of life and independence.
- Adhere to Treatment: Consistently follow prescribed eye injections, medications, and lifestyle modifications.
- Psychological Support: Seek counseling or join support groups to help manage anxiety or depression related to vision loss.
- Utilize Adaptive Devices: Options like magnifiers, screen readers, and large-print materials improve access to information and communication.
- Occupational Therapy: Specialists offer strategies to enhance functionality at home and work.
- Stay Connected: Regular appointments with healthcare providers help monitor vision and address challenges promptly.
Resources for Patients and Caregivers
- National organizations such as the American Diabetes Association and National Eye Institute offer comprehensive information, advocacy, and educational material.
- Support groups connect individuals with shared experiences and provide emotional encouragement.
- Local retina specialists and diabetes educators offer personalized care strategies.
Frequently Asked Questions (FAQs)
What is diabetic macular edema?
DME is a diabetes complication in which fluid leaks into the macula of the retina, leading to swelling and impaired central vision.
What causes DME?
DME is caused by chronic high blood sugar damaging retinal blood vessels, causing leakage and fluid accumulation.
Is DME curable?
There is no absolute cure, but treatments such as anti-VEGF injections, laser therapy, and lifestyle changes can significantly slow progression and improve symptoms.
How can I lower my risk for DME?
- Control blood sugar and blood pressure.
- Adopt a healthy lifestyle—diet, exercise, and avoid smoking.
- Attend regular eye exams with a retina specialist.
What should I do if I experience changes in my vision?
Promptly schedule a comprehensive eye examination with an ophthalmologist or retina specialist.
Does every person with diabetes get DME?
No, but long-term diabetes, poor glycemic control, and other risk factors increase the likelihood. Regular monitoring is essential.
Are there resources to help me live with DME?
- Educational material and advocacy from organizations like the American Diabetes Association and National Eye Institute.
- Local and virtual support groups.
- Vision rehabilitation specialists and occupational therapists.
Additional Tips for Managing DME
- Keep all medical appointments for eyes and diabetes.
- Monitor blood glucose and pressure at home.
- Educate yourself about DME, its treatments, and prevention strategies.
- Advocate for regular insurance coverage of eye exams.
- Communicate with your care team about any changes or difficulties.
- Seek financial support resources for treatment costs, if needed.
Summary Table: Key Points about DME
| Aspect | Details |
|---|---|
| Prevalence | ~10% of Americans with diabetes have DME |
| Primary Cause | Chronic hyperglycemia damaging retinal vessels |
| Symptoms | Blurry vision, faded colors, dark spots |
| Diagnosis | Eye exam, imaging, regular monitoring |
| Treatment | Anti-VEGF injections, laser therapies, lifestyle management |
| Support | Education, support groups, adaptive technologies |
Key Resources and Support Channels
- American Diabetes Association: National advocacy and patient resources.
- National Eye Institute: Eye health information and research updates.
- Local Retina Specialists & Ophthalmologists: Professional eye care and DME management.
- Diabetes Educators: Guidance for holistic diabetes management.
- Occupational Therapists: Training in adaptive living strategies for vision impairment.
- Vision Rehabilitation Services: Support for independent living and technology solutions.
Staying informed, proactive in your care, and connected with expert resources can help you successfully manage diabetic macular edema, protect your vision, and maintain quality of life.
References
- https://www.elmanretina.com/services/treatments-and-services/diabetic-macular-edema/
- https://www.webmd.com/diabetes/diabetic-macular-edema-treatment
- https://eyewiki.org/Diabetic_Macular_Edema
- https://my.clevelandclinic.org/health/diseases/24733-diabetes-related-macular-edema
- https://www.macularsociety.org/macular-disease/macular-conditions/diabetic-macular-oedema/
- https://preventblindness.org/diabetic-macular-edema-dme/
- https://www.mayoclinic.org/diseases-conditions/diabetic-retinopathy/multimedia/diabetic-macular-edema/img-20124558
- https://www.mdfoundation.com.au/about-macular-disease/diabetic-eye-disease/about-diabetic-macular-oedema/
Read full bio of medha deb












