Diabetic Amyotrophy: Understanding, Diagnosis, and Treatment
Explore the causes, symptoms, diagnosis, and treatment options for diabetic amyotrophy, a rare and painful complication of diabetes.
Diabetic Amyotrophy: An In-Depth Guide
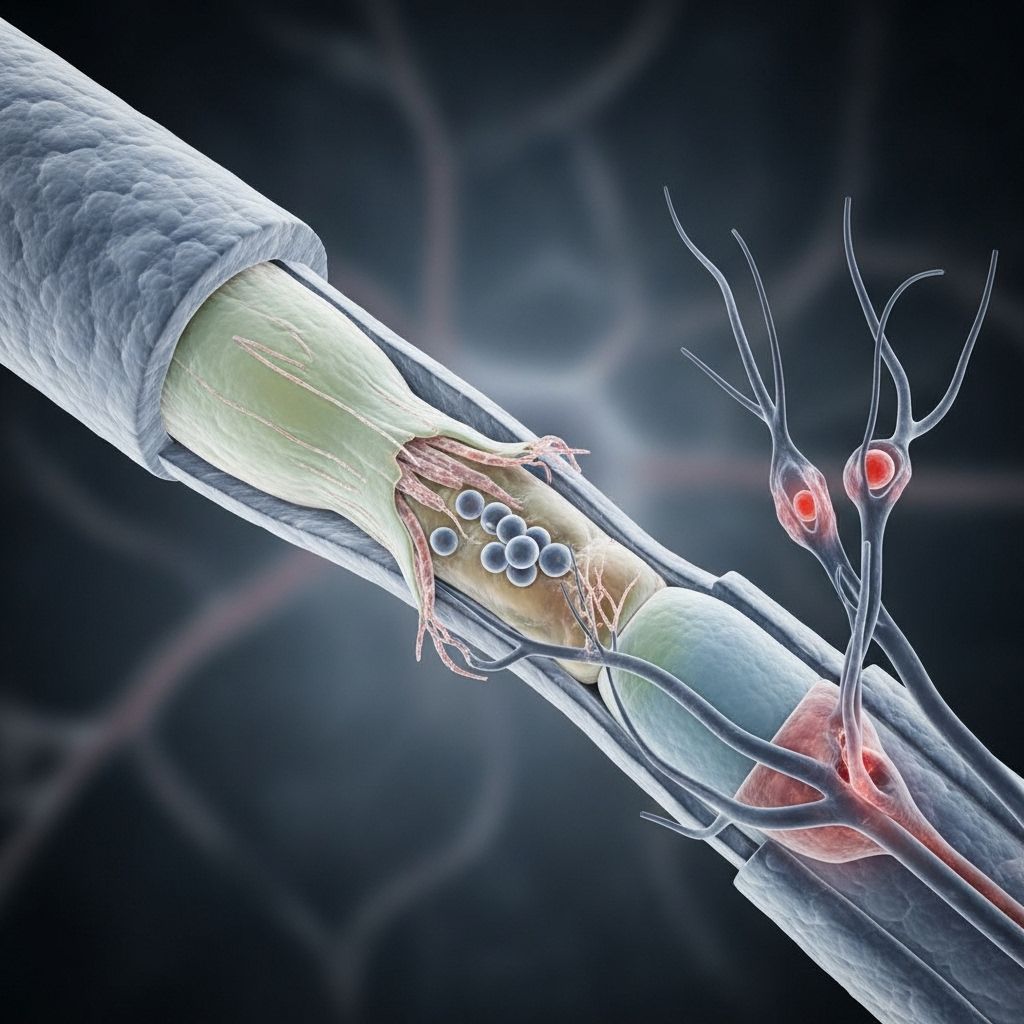
Diabetic amyotrophy is a rare yet severe nerve complication seen in people with diabetes. Unlike more typical forms of diabetic neuropathy that affect the feet and lower legs, this condition is characterized by intense pain and progressive weakness in specific areas such as the thighs, hips, buttocks, legs, and, in some cases, the chest and abdomen. With only about 1% of adults with diabetes diagnosed with diabetic amyotrophy, understanding its distinct symptoms, diagnosis, and management is crucial for affected individuals and their caregivers.
Table of Contents
- What Is Diabetic Amyotrophy?
- Symptoms and Sign Presentation
- Causes and Risk Factors
- Diagnosis
- Treatment Options
- Outlook and Prognosis
- Preventing Diabetic Amyotrophy
- Frequently Asked Questions
- Sources & References
What Is Diabetic Amyotrophy?
Diabetic amyotrophy is a rare form of diabetic neuropathy, also called:
- Proximal neuropathy
- Diabetic lumbosacral radiculoplexus neuropathy
- Bruns-Garland syndrome
This complication results from damage to peripheral nerves and primarily affects older adults diagnosed with type 2 diabetes, though it can also occur in people with type 1 diabetes and younger individuals. Notably, diabetic amyotrophy differs from other diabetes-related nerve damage in both presentation and progression.
| Feature | Diabetic Amyotrophy | Typical Diabetic Neuropathy |
|---|---|---|
| Main Location | Thighs, hips, buttocks, legs, sometimes chest/abdomen | Feet, lower legs |
| Main Symptoms | Intense pain, muscle weakness, muscle wasting, weight loss | Pain, numbness, tingling, slow progression |
| Onset | Sudden or rapid | Gradual over years |
Symptoms and Sign Presentation
Diabetic amyotrophy often manifests with distinct pain and muscle symptoms that set it apart from other diabetic neuropathies:
- Intense pain in the hip, thigh, buttocks, or legs (often asymmetric, starting on one side)
- Muscle weakness in the affected areas, making movement and standing difficult
- Muscle wasting (atrophy) over time, especially in the thighs
- Stomach pain, especially in cases involving abdominal muscle nerves
- Weight loss accompanying the onset of symptoms
- Difficulty rising from a chair or standing up
- Foot drop—the inability to lift the front part of the foot, causing stumbling or dragging when walking
Most individuals experience symptoms on one side of the body, but around a third of cases progress to both sides. Thoracic involvement may cause radiating, belt-like chest or abdominal pain and pseudohernia due to weakness in the intercostal muscles.
Symptoms Table
| Symptom | Description |
|---|---|
| Pain | Severe, burning, or stabbing in hips, thighs, or buttocks |
| Muscle Weakness | Difficulty moving or standing, pronounced fatigue |
| Muscle Wasting | Visible thinning of muscles over time |
| Stomach Pain | Sharp or severe pain, less common |
| Foot Drop | Dragging or inability to lift part of the foot |
Causes and Risk Factors
Although high blood sugar levels are known to damage nerves, the exact cause of diabetic amyotrophy is not fully understood. Unlike other long-term nerve complications, diabetic amyotrophy can occur even when blood sugar is well-managed. Proposed mechanisms include small-vessel inflammation and nerve ischemia, which restrict blood supply to the affected nerves.
Risk Factors
- Type 2 diabetes: More frequent than type 1
- Male gender: Higher prevalence among men
- Older age: Common in middle-aged and older adults
- Rapid correction of blood sugars: Sudden drops after initial diagnosis may increase risk
- Duration of diabetes: Many affected individuals have not had diabetes for very long
Diabetic amyotrophy is NOT directly linked to poor glucose management—individuals with well-controlled diabetes may still develop symptoms.
Diagnosis
Correctly diagnosing diabetic amyotrophy is essential, as several conditions share similar features. The diagnostic process involves:
- Clinical examination—to assess symptoms and muscle strength
- Medical history—especially diabetes status and onset of symptoms
- Blood tests—to evaluate blood glucose and rule out other causes
- Imaging studies—MRI, CT scan, or X-ray to exclude spinal disease or muscle infarction
- Nerve conduction studies / Electromyography (EMG)—to measure nerve and muscle function
- Spinal tap—to look for inflammation in the nervous system
Conditions to Rule Out:
- Degenerative spine disease—may cause thigh pain and muscle weakness
- Diabetic muscle infarction—leads to pain, swelling, and muscle changes
- Meralgia paresthetica—burning, tingling, and pain in the thighs
Due to the complexity, diagnosis often involves collaboration between endocrinologists, neurologists, and physical therapists.
Treatment Options
There is no single cure for diabetic amyotrophy, but several approaches provide significant symptom relief and help promote recovery:
- Diabetes management: Tight control of blood sugar levels—through medication, diet, and exercise—is essential, although it does not guarantee prevention or resolution.
- Pain relief medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), gabapentin, pregabalin (nerve pain agents), and certain antidepressants are often prescribed.
- Physical therapy: Exercise, stretching, and muscle strengthening programs help maintain mobility and minimize muscle wasting. Therapists may also introduce supportive aids, such as reachers, walkers, or raised seats.
- Neuropathic pain management: Prescription agents like amitriptyline, duloxetine, and anticonvulsants target nerve pain specifically.
- Other pain control modalities: Spinal cord stimulation, transcutaneous electrical nerve stimulation (TENS), and occasionally steroids, though evidence is mixed for steroid benefit.
- Strong painkillers: Opioids may be considered, but only for severe symptoms and under close supervision due to risks.
- Psychological support: Coping with chronic pain and mobility loss requires emotional and mental health care.
Most people improve symptomatically over time, but complete recovery is rare, and some deficits may persist for months or years.
Outlook and Recovery Prognosis
Diabetic amyotrophy is generally self-limiting, but recovery can take months to years. Pain often improves first, followed by muscle strength gains, though not everyone regains full function. Persistent muscle weakness or wasting may remain, affecting quality of life and mobility. Early intervention and rehabilitation maximize the chances for better outcomes.
Key Prognosis Points
- Pain typically lessens as weakness increases
- Most individuals regain significant strength, but full recovery is rare
- Some muscle function loss can be permanent
- Weight loss during acute stages may be reversed
- Symptoms may also recur or worsen gradually in some cases
Preventing Diabetic Amyotrophy
Unlike many diabetic complications, diabetic amyotrophy is difficult to prevent. General diabetes care strategies—such as blood sugar control, smoking cessation, and maintaining a healthy weight—help prevent other nerve and vascular complications but are less effective for this particular syndrome. The one exception is avoiding rapid correction of blood glucose levels after initial diagnosis, which may lower risk.
- Maintain steady and moderate improvements in glucose levels.
- Focus on overall diabetes care to protect against other complications.
- Seek early medical advice if sudden pain and weakness develop.
Frequently Asked Questions (FAQs)
Q: Who can get diabetic amyotrophy?
A: Although it’s more common among older men and adults with type 2 diabetes, anyone with diabetes may develop this rare complication even if their glucose levels are relatively well-controlled.
Q: What makes diabetic amyotrophy different from other diabetic neuropathies?
A: Diabetic amyotrophy mainly affects the proximal muscles (thighs, hips, buttocks), often comes on suddenly, and features pronounced pain and muscle wasting—unlike the slow, distal progression of typical diabetic neuropathy in the feet and hands.
Q: Is recovery possible for people with diabetic amyotrophy?
A: Many people see gradual improvement over several months to years, especially with therapy and good diabetes management, but most do not regain full muscle strength.
Q: Will painkillers cure the condition?
A: Painkillers and neuropathic medications can relieve discomfort but do not address the underlying nerve damage. Physical therapy plays a critical role in managing muscle function loss.
Q: Should I be worried if I develop sudden thigh pain and weakness?
A: Yes—seek medical attention promptly, as these symptoms could signal diabetic amyotrophy or another serious neurologic condition requiring evaluation and treatment.
Sources & Further Reading
- AANEM – Diabetic Amyotrophy: Muscle and Nerve Disorders
- NCBI Bookshelf – Diabetic Amyotrophy
- American Diabetes Association – Understanding Neuropathy and Diabetes
- Healthline Editorial Policy
Takeaway
Diabetic amyotrophy is a distinct and painful form of neuropathy seen rarely in adults with diabetes, often leading to muscle weakness, wasting, and chronic discomfort. Early recognition, prompt diagnosis, and a comprehensive approach to pain management and physical rehabilitation are key to improving outcomes. Even for those with well-controlled diabetes, being vigilant for new muscle pain and weakness is vital for receiving the best possible care.
References
- https://patient.info/diabetes/diabetes-mellitus-leaflet/diabetic-amyotrophy
- https://www.medlink.com/articles/diabetic-amyotrophy
- https://www.webmd.com/diabetes/diabetic-amyotrophy
- https://www.healthline.com/health/diabetes/diabetic-amyotrophy
- https://www.ncbi.nlm.nih.gov/books/NBK560491/
- https://primerevivalresearch.com/blogs/diabetic-amyotrophy/
- https://practicalneurology.com/diseases-diagnoses/neuromuscular/diabetic-amyotrophy/30445/
- https://www.mayoclinic.org/diseases-conditions/diabetic-neuropathy/symptoms-causes/syc-20371580
Read full bio of Sneha Tete












