Current Treatment Options for Myelodysplastic Syndrome (MDS)
An in-depth guide to treatment approaches, therapies, and supportive care for managing myelodysplastic syndrome.
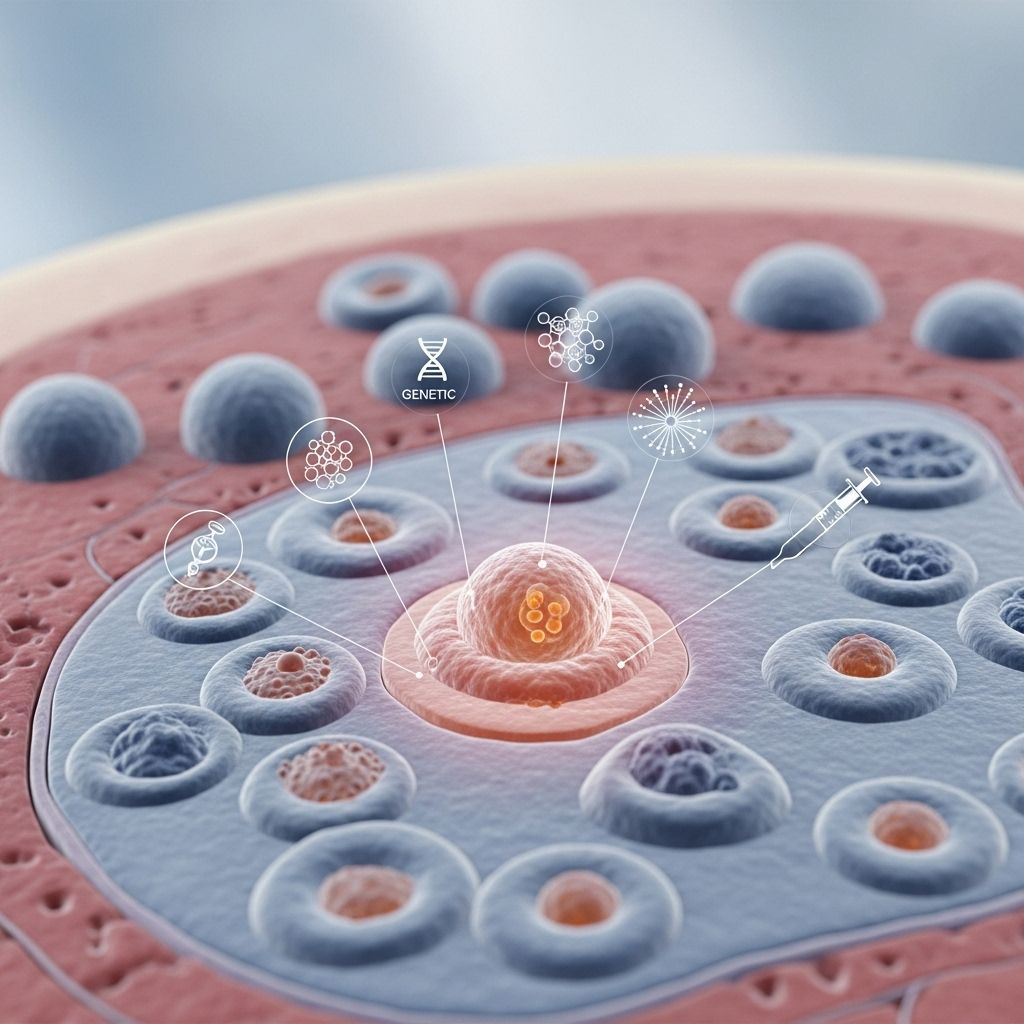
Myelodysplastic syndrome (MDS) refers to a group of bone marrow disorders that disrupt the normal production of healthy blood cells. Managing this condition involves a range of treatments, from medications and blood transfusions to stem cell transplantation and supportive care. The choice of therapy depends on factors such as the specific MDS subtype, its severity, and an individual’s age and overall health.
What Is Myelodysplastic Syndrome?
Your bone marrow is responsible for creating immature blood cells (stem cells) that eventually develop into three types of mature blood cells:
- Red blood cells (RBCs)
- White blood cells (WBCs)
- Platelets
In MDS, the bone marrow cannot produce enough healthy mature blood cells. Many stem cells either die in the marrow or fail to mature. This leads to lower numbers of functioning blood cells, a condition called cytopenia.
MDS is classified as a type of cancer, though it can progress at different rates and may sometimes transform into acute myeloid leukemia (AML).
Goals of MDS Treatment
The primary treatment goals for MDS are:
- Preventing severe complications (such as infections or anemia)
- Relieving symptoms and improving quality of life
- Slowing the progression of the disease
- Achieving long-term remission, where possible
Because MDS affects people differently, your healthcare team will personalize your treatment plan based on risk the category, symptoms, and personal health factors.
Types of Treatment for MDS
MDS can be managed by various approaches. The main types of treatment include:
- Supportive care
- Drug therapy and chemotherapy
- Immunotherapy or immunosuppressive therapy
- Stem cell transplantation
- New or experimental treatments (clinical trials)
- Lifestyle changes and natural remedies
Supportive Care
Supportive care aims to manage the symptoms and complications that arise from low blood counts, rather than addressing the underlying disease directly.
- Blood transfusions: Used to treat anemia (low RBCs) or thrombocytopenia (low platelets). These boost blood cell counts temporarily and relieve symptoms like fatigue and shortness of breath.
- Antibiotics or antiviral medications: Reduce the risk of infection in people with low white blood cell counts.
- Growth factors: Medications like erythropoietin or granulocyte colony-stimulating factor (G-CSF) promote the production of new blood cells in the bone marrow.
Supportive care treatments are often ongoing and are crucial to maintaining a person’s quality of life throughout their treatment journey.
Drug Therapy and Chemotherapy
Certain medications can slow disease progression, reduce the need for transfusions, or target the abnormal bone marrow cells directly.
- Hypomethylating agents:
- Azacitidine and decitabine help restore normal function to genes that control cell growth and death and can delay disease progression, particularly in higher-risk MDS.
- Immunomodulatory drugs:
- Lenalidomide is especially effective in patients with a specific chromosomal abnormality (“del(5q) syndrome”). It can reduce transfusion requirements and promote healthy blood cell production.
- Immunosuppressive therapy:
- Antithymocyte globulin (ATG) and cyclosporine can dampen an overactive immune response attacking the bone marrow. Suitable mainly for younger patients or those with certain subtypes of MDS.
- High-intensity chemotherapy:
- This approach uses strong drugs (e.g., cytarabine, daunorubicin, idarubicin) at high doses. Often reserved for cases where MDS has transformed into acute myeloid leukemia or as part of preparation for stem cell transplantation.
| Drug Type | Examples | Main Use |
|---|---|---|
| Hypomethylating Agents | Azacitidine, Decitabine | Slow disease progression |
| Immunomodulatory Drugs | Lenalidomide | Reduce transfusion needs (del(5q) subtype) |
| Immunosuppressive Therapy | ATG, Cyclosporin | Suppressed immune activity in bone marrow |
| High-Intensity Chemotherapy | Cytarabine, Daunorubicin | Treat AML or prepare for transplant |
Stem Cell Transplantation
A stem cell transplant is currently the only treatment capable of potentially curing MDS. The process involves high-dose chemotherapy (sometimes with radiation) to destroy abnormal bone marrow cells, followed by the infusion of healthy donor stem cells to rebuild healthy marrow.
Stem cell transplantation (also called allogeneic hematopoietic stem cell transplantation) is usually recommended for:
- Younger, medically fit individuals
- People with high-risk MDS likely to progress to leukemia
- Those with a suitable donor (genetically matched relative or unrelated donor)
While stem cell transplant offers the chance for long-term remission or cure, it has significant potential risks and side effects, including increased infection risk, graft-vs-host disease, and organ complications. Not all patients are eligible for this intense form of therapy, especially older adults or those with health problems.
Immunotherapy
Immunotherapy, or biologic therapy, helps activate the immune system to fight abnormal marrow cells. While not the mainstay for most people with MDS, immunotherapies are being explored further in research and may play a greater future role.
Clinical Trials and Emerging Therapies
Researchers are continually investigating new approaches to treating MDS. Clinical trials may explore:
- Novel drug combinations or agents (e.g., luspatercept, imetelstat)
- Targeted therapies based on genetic mutations
- Different transplantation strategies or supportive care tactics
Taking part in a clinical trial could offer access to promising new treatments, especially if standard therapies have not worked.
Natural Remedies and Lifestyle Approaches
While there is no alternative cure for MDS, incorporating certain lifestyle habits and natural remedies can help support general health and symptom management.
- Healthy nutrition: Consuming iron-rich foods, getting sufficient vitamins and minerals, and staying hydrated can help manage anemia and fatigue.
- Staying active: Light to moderate physical activity tailored to your energy level can support your well-being and circulation.
- Hand hygiene and infection control: Reduces the risk of infection when immune defenses are low.
- Managing stress: Relaxation techniques, counseling, and support groups can help cope with the psychological aspects of MDS.
Always consult your healthcare provider before starting any complementary therapies or making significant lifestyle changes, especially if you are undergoing active treatment.
Prognosis and Outlook
The long-term outlook for someone with MDS depends on several factors:
- Specific MDS subtype and risk level (as evaluated by genetic tests, blast counts, and other markers)
- Age and overall health
- Response to treatment
- Eligibility for stem cell transplant
Lower-risk MDS cases may be managed for years with medication and supportive care, while higher-risk cases require more aggressive therapy. For many, MDS is a chronic disease needing ongoing management to control symptoms and complications.
Some people may eventually develop acute myeloid leukemia (AML), a more aggressive form of blood cancer. Early and ongoing management of MDS is critical for best outcomes.
Frequently Asked Questions (FAQs)
What are the first signs of myelodysplastic syndrome?
The earliest symptoms of MDS result from low blood cell counts and may include fatigue, frequent infections, bruising or bleeding easily, and shortness of breath. In some cases, MDS is discovered incidentally during routine blood tests.
Can myelodysplastic syndrome be cured?
For many people, MDS is a chronic disease managed by medications and supportive care, but not cured. The only treatment known to offer a potential cure is an allogeneic stem cell transplant, which is suitable primarily for younger, healthy individuals.
Who is at risk for MDS?
MDS is most common in individuals over age 65. Other risk factors include prior chemotherapy or radiation for other cancers, certain inherited genetic conditions, and exposure to toxins like benzene.
How does MDS differ from leukemia?
While both are blood cancers, MDS is characterized by ineffective production of mature blood cells, leading to cytopenias, while acute leukemia involves a rapid increase in immature abnormal cells. Over time, MDS can progress to acute myeloid leukemia (AML) in some cases.
Should I consider a clinical trial for MDS?
Many people with MDS can benefit from participating in clinical trials, especially if standard therapies have been exhausted or if the disease has high-risk features. Ask your medical team about promising trials suitable for your case.
Key Points to Discuss With Your Doctor
- What type and risk category is my MDS?
- What are the goals of my treatment plan?
- What therapies are most appropriate for my age and health?
- What side effects or complications should I anticipate?
- Am I eligible for a stem cell transplant or clinical trials?
- How will my quality of life be monitored and supported?
Summary
Myelodysplastic syndrome presents complex challenges, but advances in therapy and a personalized, holistic approach mean that many people can achieve good symptom control and quality of life. New treatments and ongoing research continue to improve outlooks for those living with MDS.
References
- https://www.healthline.com/health/myelodysplastic-syndrome
- https://www.cancer.gov/types/myeloproliferative/patient/myelodysplastic-treatment-pdq
- https://haematologica.org/article/view/11858
- https://www.healthline.com/health/leukemia/myelodysplastic-syndrome-treatment
- https://www.healthline.com/health/video/break-it-down-anemia-in-mds-bt
- https://pubmed.ncbi.nlm.nih.gov/36066514/
- https://www.healthline.com/health/video/how-to-increase-red-blood-cells
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6142467/
- https://www.nature.com/articles/s41408-022-00765-8
Read full bio of Sneha Tete












