How Accurate Are CT Scans for Detecting Lung Cancer?
Understand the benefits, limitations, and accuracy of CT scans for early lung cancer detection, including risks and screening recommendations.
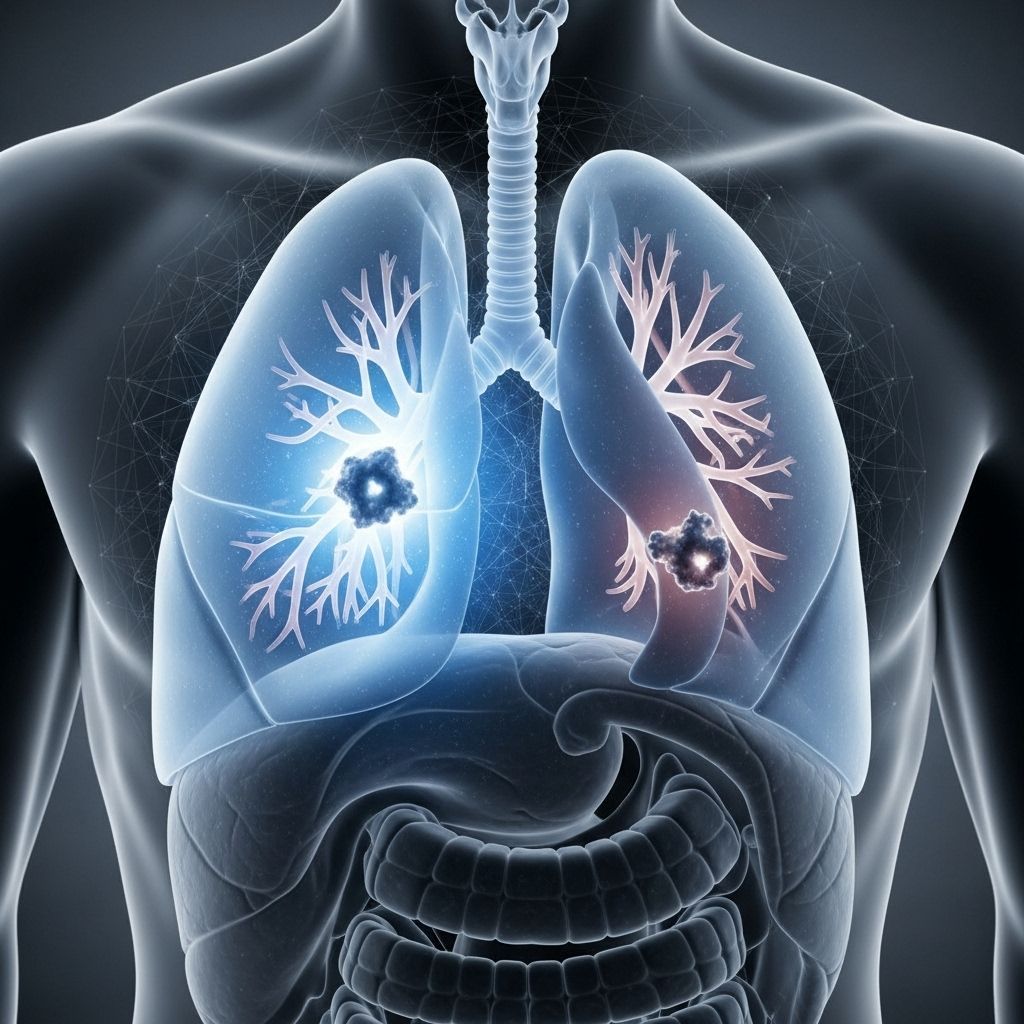
Lung cancer remains the leading cause of cancer-related deaths worldwide. Early detection is crucial for effective treatment, and low-dose computed tomography (LDCT) scans have emerged as a vital tool in lung cancer screening. This article provides a detailed overview of the accuracy, benefits, limitations, and recommendations for using CT scans to detect lung cancer in high-risk individuals.
What Is a CT Scan?
A computed tomography (CT) scan is a specialized imaging test that uses X-rays to create cross-sectional images of the body. In the context of lung cancer, a CT scan generates highly detailed pictures of the lungs and surrounding tissues. The low-dose version (LDCT) uses much less radiation and is specifically recommended for screening people at high risk for lung cancer.
- Standard CT: Typically used for diagnosing abnormalities when symptoms are present or as follow-up for suspected cancer.
- Low-dose CT (LDCT): Designed for screening, using much less radiation than a standard CT, and aimed at detecting lung cancer in asymptomatic, high-risk individuals.
Low-dose CT is currently the only screening tool recommended by major health agencies, including the Centers for Disease Control and Prevention (CDC), for early detection of lung cancer in high-risk groups.
- LDCT scans can identify nodules or masses in the lungs, often before symptoms occur, enabling earlier intervention and improved outcomes.
- The accuracy of CT scans for lung cancer detection is high. Studies report that CT can be over 90% accurate in identifying lung tumors and 75% to 80% accurate in detecting involvement in chest lymph nodes.
- LDCT scans produce detailed images, helping doctors distinguish between different types of tissue, tumors, and other abnormalities that might be missed by a chest X-ray.
Important point: While LDCT scans are highly effective in identifying suspicious lung nodules, they are not perfect. They cannot reliably distinguish between benign (non-cancerous) and malignant (cancerous) nodules, often requiring additional diagnostic procedures for confirmation.
CT Scans versus Chest X-Rays
| Feature | Low-Dose CT (LDCT) | Chest X-ray |
|---|---|---|
| Image detail | High, cross-sectional | Low, two-dimensional |
| Sensitivity | Very high | Much lower |
| Tumor detection size | Smaller tumors (>2-3 mm) | Larger tumors only (>1 cm) |
| Radiation exposure | Low | Lower |
| Recommended for screening? | Yes | No |
CT scans can detect smaller nodules than chest X-rays and are the gold standard for lung cancer screening in people at high risk. In contrast, chest X-rays often miss early, small, or otherwise hidden tumors, leading to delayed diagnosis.
Understanding False-Positive Results with CT Scans
False positives happen when a scan indicates the presence of a tumor or abnormality that examination later reveals is not cancer. This is a known risk associated with low-dose CT screening for lung cancer.
- Incidence: Research shows that false-positive rates for initial baseline LDCT screening range from 9.6% to 28.9%.
- Consequences: A false-positive test result can lead to significant emotional stress and anxiety. It may also mean more invasive follow-up procedures, such as needle biopsies or even surgeries, which carry their own risks (including infection, bleeding, and complications from anesthesia).
- Physicians usually follow up with additional imaging or tissue sampling to clarify unclear or suspicious findings from LDCT screening.
About Overdiagnosis
Overdiagnosis refers to the detection of cancers that would never cause symptoms or affect lifespan. In the context of LDCT screening:
- Some slow-growing tumors or nodules may be found that would not have affected the person during their lifetime, particularly in older adults or those with serious other health conditions.
- Overdiagnosis can result in unnecessary treatments, increased healthcare costs, and heightened emotional distress.
- It remains a limitation of screening but is nonetheless outweighed by the significant potential to detect treatable cancers early in high-risk individuals.
Benefits and Risks of LDCT Scans
Like all medical procedures, LDCT scans have both advantages and risks.
- Benefits:
- Facilitates early detection of lung cancer, often before symptoms start.
- Early-stage detection vastly improves survival rates: people diagnosed at stage 1 via CT screening may have long-term survival rates as high as 81% to 95% at 10–20 years.
- Can help monitor at-risk patients over time, tracking growth or changes in nodules found during earlier scans.
- Enables minimally invasive treatments, such as CT-guided biopsies or ablation, thereby improving patient comfort and outcomes.
- Risks:
- False-positive and false-negative results, as discussed.
- Overdiagnosis, leading to unnecessary intervention.
- Exposure to low levels of ionizing radiation, although much lower than standard CT scans.
- Potential complications from follow-up diagnostic procedures.
Lung Cancer Screening Recommendations
National and international health agencies recommend LDCT screening for people deemed high risk for developing lung cancer. These guidelines include the following criteria:
- Aged between 50–80 years (specific age ranges vary slightly by authority).
- Have a 20 pack-year or greater history of smoking (calculated as packs of cigarettes smoked per day multiplied by years smoked).
- Currently smoke or have quit within the past 15 years.
- No symptoms of lung cancer at the time of screening.
An annual LDCT screening is recommended for those meeting these criteria, provided the individual remains healthy enough to undergo curative lung surgery if cancer is detected.
Screening Frequency
- Annual LDCT screening is generally suggested for eligible individuals, based on ongoing risk.
- If no nodules are found, routine yearly screening continues.
- If suspicious findings are present, further imaging or biopsy may be required to confirm or rule out cancer.
Other Lung Cancer Screening and Diagnostic Tools
While LDCT has emerged as the screening standard, other tools can be useful in the diagnosis and management of lung cancer:
- PET scans: Used mainly after an abnormal CT, PET scans help determine if detected nodules are metabolically active (more likely to be cancerous).
- MRI scans: Sometimes used to assess potential cancer spread into the brain or other organs.
- Sputum cytology: Examines mucus from the lungs to look for cancer cells.
- Biopsy: A tissue sample, obtained via needle, bronchoscopy, or surgery, remains the definitive diagnostic standard.
Improving Outcomes with Early Detection
Research has confirmed that annual LDCT screening can dramatically improve long-term survival rates. Early-stage detection (stage 1A) has the most pronounced impact on chances for successful treatment and extended survival:
- A large long-term study showed that people diagnosed at stage 1 with CT screening had a 20-year survival rate of 81%.
- Survival rates for stage 1A cancer detected with screening may reach up to 95%.
These findings highlight the lifesaving potential of regular LDCT screening for eligible high-risk populations and reinforce the role of early intervention in changing the outlook for lung cancer.
Key Considerations Before Getting a CT Scan for Lung Cancer
- Discuss your personal risk profile with your doctor, including smoking history and any other relevant factors.
- Be prepared for possible follow-up tests if your screening shows lung abnormalities.
- Understand the potential for false positives, overdiagnosis, and the risks associated with follow-up procedures.
- Balance the benefits of early detection against the risks of unnecessary interventions — a discussion best guided by a healthcare professional familiar with the latest guidelines.
Frequently Asked Questions (FAQs)
How often should I get a CT scan for lung cancer?
Guidelines recommend annual LDCT scans for people at high risk, as long as their risk status remains unchanged and they are healthy enough for treatment if cancer is found.
Is a CT scan safe for lung cancer screening?
LDCT scans use significantly less radiation than standard CT scans and are considered safe for regular screening in eligible individuals. However, there is still a small risk from radiation exposure and potential complications from follow-up tests.
What happens if my CT scan finds a lung nodule?
A lung nodule will usually need further evaluation. This may include repeat imaging at a future date to see if the nodule changes in size, or a biopsy to determine if the nodule is cancerous. Not all nodules are cancer — many are benign and harmless.
Can a CT scan always tell if a nodule is cancerous?
No. A CT scan can detect a nodule’s size, shape, and location, but it cannot definitively tell if it is cancerous. Biopsy and/or other imaging tests are often needed for a conclusive diagnosis.
Are there alternatives to a CT scan for lung cancer screening?
Currently, LDCT is the only recommended screening tool for lung cancer in high-risk populations. Other imaging methods may be used for diagnosis or staging, but not for initial screening.
Summary
Low-dose CT scans have revolutionized early detection of lung cancer in high-risk individuals by providing high sensitivity and detailed imaging. Although not free of risks, such as false positives and overdiagnosis, LDCT remains the standard of care for lung cancer screening. People considering screening should consult with their healthcare provider to thoroughly assess their risk factors and understand the benefits and limitations of this powerful diagnostic tool.
References
- https://www.healthline.com/health/lung-cancer/how-accurate-is-ct-scan-for-lung-cancer
- https://www.mylungcancerteam.com/resources/what-does-a-ct-scan-show-about-lung-cancer-diagnosis-accuracy-and-results
- https://www.mainlinehealth.org/blog/lung-cancer-diagnosis-and-treatment
- https://www.medicalnewstoday.com/articles/screening-sharply-improves-lung-cancer-long-term-survival
- https://www.healthline.com/health/lung-cancer/screening-and-early-detection
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3709596/
- https://mednexus.org/doi/10.1097/CM9.0000000000002353
- https://www.medicalnewstoday.com/articles/ct-scan-for-lung-cancer
Read full bio of medha deb












