Cortical Cataract: Causes, Symptoms, and Treatments
Learn about the causes, progression, symptoms, and surgical solutions for cortical cataracts, a leading cause of vision problems in aging adults.
Cortical Cataract: Understanding This Common Eye Condition
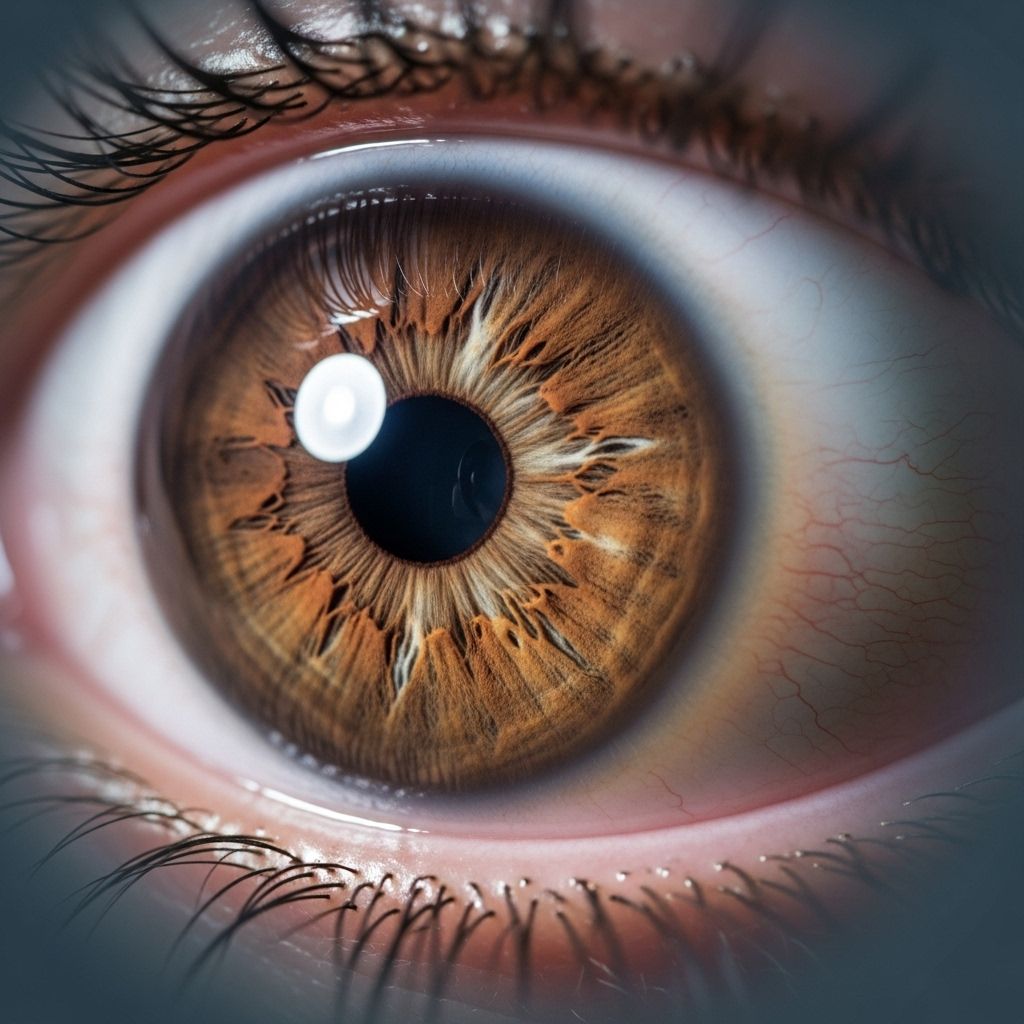
Cortical cataracts are a prevalent type of age-related cataract characterized by cloudy or opaque areas that form in the cortex, or outer edge, of the eye’s natural lens. These clouded streaks typically begin at the lens periphery and grow toward the center in a spoke-like pattern, disrupting the passage of light and affecting vision. Recognizing symptoms, understanding risk factors, and knowing treatment options are vital for managing this condition and preventing vision loss.
What Are Cortical Cataracts?
A cortical cataract is a specific form of cataract where cloudiness develops in the cortical (outer) layer of the eye’s lens. The lens, located just behind the iris and pupil, focuses light onto the retina to produce clear vision. In cortical cataracts, changes in water content and the breakdown of lens proteins create clumps that scatter light. This results in opacity that appears as white, wedge-shaped spokes at the lens edge.
- The cortex is the outer region of the lens.
- Cataract formation here begins at the periphery and typically grows slowly inward.
- The affected lens scatter incoming light, causing visual symptoms such as glare and blurriness.
The Anatomy of the Eye Lens
The eye’s lens is a clear, flexible, and nearly colorless structure behind the iris. It is made of highly organized proteins arranged in layers:
- Nucleus: The central core of the lens.
- Cortex: The outer layer surrounding the nucleus, where cortical cataracts develop.
- Capsule: The thin, transparent envelope around the lens.
Causes and Risk Factors
Cortical cataracts can develop when natural changes occur with aging, but a number of risk factors can increase susceptibility. The primary cause is the age-related breakdown and clumping of proteins in the lens cortex. However, genetics, lifestyle choices, and systemic health conditions also play vital roles.
- Age: Most common in individuals over 60 years; risk increases with age.
- Diabetes: Higher blood sugar levels can cause changes in lens hydration and accelerate cataract formation.
- Hypertension: High blood pressure is linked to an increased risk of cataracts.
- UV Exposure: Prolonged or intense ultraviolet (UV) light exposure can damage lens proteins.
- Smoking: Tobacco use contributes to oxidative stress in the eye, promoting cataract formation.
- Diet: Poor nutrition, especially diets low in carotenoids or vitamin C, may heighten risk.
- Other risk factors: Family history of cataracts, history of eye trauma or injury, and high or very low refractive errors (myopia/hyperopia).
How Common Are Cortical Cataracts?
Cortical cataracts are among the most common forms of cataracts diagnosed worldwide. According to epidemiological studies:
- Incidence rises significantly after age 40.
- Over half of Americans have developed some form of cataract, including cortical, by age 80.
- Cortical cataracts account for a substantial portion of age-related vision impairment, especially in older adults.
The risk increases steadily with advancing age, and the condition remains a global health concern as the population ages.
Symptoms: How Cortical Cataracts Affect Vision
Because the cortex plays a major role in transmitting light, opacities in this area can lead to a wide range of visual changes and discomforts. The symptoms are often progressive, with subtle changes early on and more significant impairment as the cataract advances.
- Blurry or Hazy Vision: Reduced visual clarity; images may appear foggy or out of focus.
- Glare Sensitivity: Heightened discomfort from headlights, sunlight, or other bright lights. Halos or starbursts around light sources may appear.
- Night Vision Difficulties: Driving at night may become challenging due to increased glare and decreased contrast sensitivity.
- Reduced Color Perception: Colors may seem faded, dull, or yellowed. Differentiating between similar shades can be hard.
- Double Vision: Some people may notice double or ghosted images, usually in one eye (monocular diplopia).
- Poor Depth Perception: Objects may appear flatter and judging distances becomes problematic.
- Difficulty with Low Contrast: Struggling to see contrasts, particularly in low-light conditions.
Progression: How Fast Do Cortical Cataracts Develop?
Cortical cataracts usually develop gradually and can take years to significantly impair vision. Progression rates vary between individuals and can be influenced by risk factors such as unmanaged diabetes or excessive UV exposure. Without intervention, the clouded spokes expand from the cortex toward the lens center, eventually affecting the entire lens and causing more severe visual symptoms.
| Progression Stage | Symptoms and Vision Impact |
|---|---|
| Early | Subtle glare, mild blurring, few noticeable changes |
| Moderate | Increased glare, more pronounced blurring, trouble with night vision, faded color vision |
| Advanced | Significant vision loss, double vision, difficulty with daily tasks, possible functional blindness |
Diagnosis of Cortical Cataracts
An eye care professional can detect cortical cataracts through a comprehensive eye examination, which may include:
- Visual acuity test: Measures clarity of vision using eye charts.
- Slit-lamp examination: Uses a special microscope to assess the lens and other eye structures in detail.
- Pupil dilation: Expands the pupil to allow a clear view of the lens and retina.
- Retinal exam: Checks for other eye conditions that may contribute to symptoms.
Treatment Options
There is currently no way to reverse or cure cortical cataracts with medication or lifestyle changes alone. Management focuses on delaying their progression and ultimately removing the cloudy lens when vision loss impairs quality of life.
Non-Surgical Management
- Updated Eyeglasses Prescription: In early stages, a new prescription for glasses may temporarily improve vision.
- Brighter Lighting: Using improved lighting at home and work can make reading or performing tasks easier.
- Magnifying Devices: Helpful for reading and close-up work.
- Driving Precautions: Avoiding night driving, especially in cases of glare sensitivity.
Surgical Treatment
When cataracts progress to the point that they significantly impede daily activities, cataract surgery is the only effective treatment. During this safe and common procedure:
- The cloudy natural lens is removed via a minimally invasive technique, often involving ultrasound (phacoemulsification).
- A clear, artificial intraocular lens (IOL) is implanted in its place.
- Most surgeries take fewer than 30 minutes, and recovery is usually swift with rare complications.
The success rate for cataract surgery is extremely high, and most individuals experience dramatic improvements in vision, color perception, and overall quality of life.
Potential Complications
- If left untreated, advanced cortical cataracts can lead to significant and irreversible vision loss or blindness.
- After surgery, rare complications may include infection, retinal detachment, swelling, or posterior capsule opacification (‘secondary cataract’).
Prevention and Eye Health Tips
While aging is the single largest risk factor, certain lifestyle measures can reduce your risk or slow cataract progression:
- Protect Eyes from UV: Always wear sunglasses that block UVA/UVB rays outdoors.
- Control Underlying Conditions: Manage diabetes and high blood pressure with regular medical care.
- Eat a Nutrient-Rich Diet: Include plenty of colorful fruits and vegetables for antioxidants, carotenoids, and vitamin C.
- Avoid Smoking and Excessive Alcohol: Both increase oxidative damage to eye tissues.
- Schedule Routine Eye Exams: Early detection and monitoring are vital for effective management.
Living with Cortical Cataracts
Early diagnosis and regular eye care are crucial for preserving vision. Many patients adjust well in the initial stages, but monitoring for symptom progression allows timely surgical intervention. Communicating any changes in vision to your eye care provider ensures personalized and effective care.
Frequently Asked Questions (FAQs)
What is the main cause of cortical cataracts?
The leading cause is age-related changes in the lens, with protein clumping in the cortex. Other contributing factors include diabetes, hypertension, smoking, and excessive UV light exposure.
Can cortical cataracts lead to total blindness?
Yes, if left untreated, advanced cortical cataracts can cause severe vision loss and functional blindness. However, cataract surgery can typically restore sight.
Is surgery always required for cortical cataracts?
Not in the early stages. Glasses and visual aids may help temporarily, but surgery is the definitive treatment once significant vision disruption occurs.
How can I lower my risk of developing cortical cataracts?
Wearing UV-protective eyewear, eating a healthy diet rich in antioxidants, managing chronic health conditions, and avoiding smoking are all effective strategies.
What should I expect after cataract surgery?
Most patients experience substantial improvement in vision within a few days. It is an outpatient procedure, and risks are minimal when performed by experienced surgeons. Proper postoperative care ensures optimal recovery.
References
- https://www.allaboutvision.com/conditions/cataracts/cortical/
- https://www.medicalnewstoday.com/articles/cortical-cataracts
- https://www.healthline.com/health/eye-health/cortical-cataract
- https://bestcataractsurgeons.com/complete-guide-to-cortical-cataracts/
- https://www.medicalnewstoday.com/articles/posterior-subcapsular-cataract
- https://www.mayoclinic.org/diseases-conditions/cataracts/symptoms-causes/syc-20353790
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4687256/
- https://www.britannica.com/science/cataract-eye
- https://www.morningtoneye.com.au/how-long-can-cataract-surgery-be-postponed/
Read full bio of Sneha Tete












