Cortical Cataract: Causes, Symptoms, Diagnosis, and Treatment
Learn how cortical cataracts affect your vision, why they form, and which treatments offer the best outcomes for preserving eye health.
Cortical Cataract: What Is This, and How Does It Affect Your Eyes?
Cortical cataracts form when the outer edge (cortex) of your eye’s lens becomes cloudy, affecting how you see. This gradual clouding, led by changes in lens water content and protein clumping, leads to increasingly blurry vision, problems with night sight, heightened glare sensitivity, and even, eventually, significant vision loss if untreated. With appropriate care—including lifestyle changes and surgical intervention—cortical cataracts can be effectively managed or even reversed, restoring clear vision for millions globally.
Understanding the Eye Lens and Cortical Cataracts
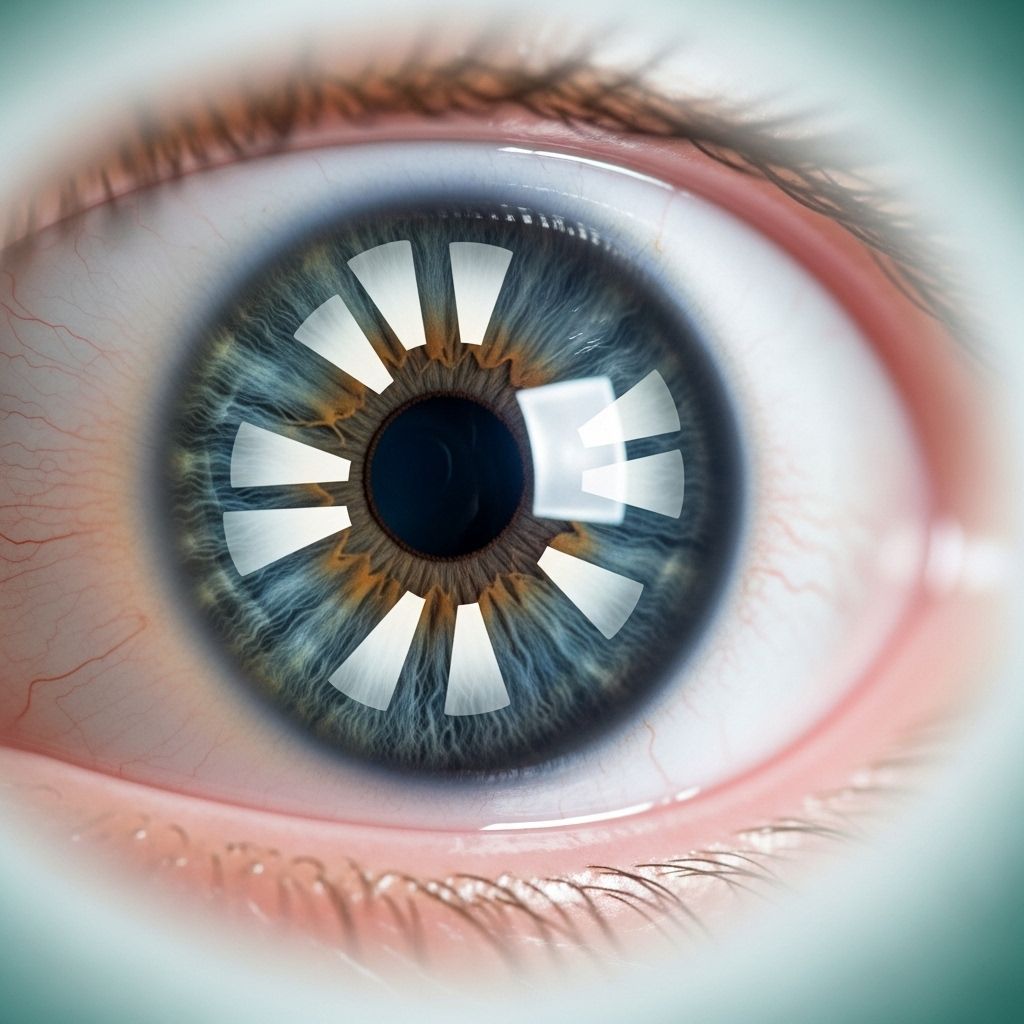
The lens of your eye—a curved, transparent disk found just behind the pupil and iris—focuses incoming light onto the retina, allowing you to see clearly at varying distances. The lens has a central “nucleus” and an outer layer called the cortex. A cortical cataract specifically affects this cortical layer, resulting in the development of cloudy streaks or wedge-like opacities at the lens periphery which may gradually move toward the center.
- The cortex is responsible for much of the lens’s flexibility and focusing power.
- As cortical opacities progress, more of your visual field is affected—sometimes leading to severe impairment.
How Do Cortical Cataracts Develop?
Cortical cataracts arise as proteins in the lens cortex break down and clump together. The initial changes often start as wedge- or spoke-shaped streaks at the edge of the lens. Over time, cloudiness can advance toward the center, causing increasing vision problems.
Main Causes
- Aging is the most common trigger due to natural changes in lens structure over time.
- Genetic factors and a family history of cataracts can increase risk.
- Metabolic conditions like diabetes substantially raise the chance of cataract formation.
- Eye trauma or injuries may disrupt lens integrity, speeding cataract progression.
- Medication use, especially long-term corticosteroids, has been linked to higher risk.
- Radiation therapy to the head or eyes may contribute to lens opacification.
- Previous eye surgery, such as for glaucoma, might also predispose you to cortical cataracts.
Risk Factors That Speed Up Cataract Formation
- Smoking and tobacco exposure
- High alcohol intake
- Chronic ultraviolet (UV) sunlight exposure without adequate eye protection
- Certain prescription medications: ACE inhibitors, fibrates, and alpha-glucosidase inhibitors (evidenced in a 2020 Singapore study)
Prevalence and Demographics
Cataracts—of which cortical cataracts are a key type—are an extraordinarily common eye condition, particularly with aging. In the United States alone, more than half of people over 80 years old either have a cataract or have undergone cataract surgery. Cortical cataracts represent one of the main subtypes along with nuclear and posterior subcapsular cataracts.
- While they can affect all age groups, cortical cataracts are most prevalent in older adults.
- A 2019 study reported that 85% of farsighted individuals scheduled for cataract surgery had cortical cataracts, compared to 37% of nearsighted patients and 82% of those with typical vision.
How Cortical Cataracts Affect Vision
As the lens cortex clouds, patients notice a gradual—but relentless—change in their vision. The impact and symptoms are directly related to how close the opacities are to the center (visual axis) and how much of the lens is involved.
Common Symptoms
- Blurry or hazy vision
- Notable trouble seeing at night, especially during activities such as driving
- Sensitivity to bright lights or glare (commonly from headlights or sunlight)
- Muted or yellowish colors; difficulty distinguishing hues
- Double vision in one eye (diplopia) or distorted vision
- Halos or blurriness around lights
- Frequent changes in eyeglass prescriptions, particularly worsening farsightedness
These symptoms can slowly reduce independence, making reading, driving, and enjoying daily life more challenging. Most cortical cataracts are painless but significantly impact quality of life.
Progression and Stages
Cortical cataracts typically develop slowly. The speed can vary by individual, ranging from months to many years. Without medical intervention, the spoke-like opacities can merge and cover more of the lens, further disrupting vision.
| Stage | Description |
|---|---|
| Early | Small wedge-shaped opacities at the lens’s periphery; minimal symptoms. |
| Moderate | Opacities expand toward the center, causing mild blur, glare, or color changes. |
| Advanced | Cataract covers a substantial part of the lens, significantly impairing vision and daily functioning. |
| Mature | The entire lens is cloudy. Profound vision loss, possible legal blindness without surgery. |
The timeline depends on risk factors, age, underlying health, and whether the cortical cataract occurs alongside other types (such as nuclear or posterior subcapsular cataracts).
Diagnosis
Healthcare providers or eye specialists diagnose cortical cataracts via a comprehensive eye examination. Evaluation typically includes:
- Visual acuity testing: To measure how clearly you can see at various distances.
- Slit-lamp examination: The ophthalmologist uses a bright microscope to inspect the lens’s cortex for evidence of cloudiness or spokes.
- Retinal exam: Assessing the health of the retina and the degree to which the cataract impairs visualization.
- Patient history: Reviewing risk factors such as medical conditions, medication use, trauma, and family history.
Treatment Options for Cortical Cataracts
Treatment choices vary based on the severity of vision impairment and patient needs. Although early-stage cortical cataracts may not require intervention, regular monitoring is vital to track progression.
Non-Surgical and Conservative Treatments
- Eyeglasses or contact lenses: Prescription adjustments may help compensate for mild lens changes.
- Brighter lighting and anti-glare tools: Useful for reading and activities requiring sharp vision.
- Magnifying lenses: Assist with focused tasks such as reading or sewing.
- UV-protective sunglasses: Reducing sunlight exposure can help slow progression and ease symptoms.
- Healthy lifestyle changes: Avoiding tobacco, moderating alcohol, controlling diabetes, and maintaining good nutrition may delay onset and slow advancement.
Cataract Surgery
When cortical cataracts interfere with daily life, surgical removal of the cloudy lens remains the only definitive cure. The operation is typically a phacoemulsification procedure, where the surgeon breaks up and removes the cataract-affected lens and replaces it with a clear artificial intraocular lens (IOL).
- The surgery is usually performed on an outpatient basis and boasts a high success rate for restoring vision.
- Modern techniques are highly safe, although minor risks (infection, lens dislocation, retinal detachment) remain.
Complications of Untreated Cortical Cataracts
If untreated, advanced cortical cataracts can cause profound, even permanent, vision loss. Because the clouding grows from the outside in, it can ultimately cover the entire lens, leading to:
- Severe visual impairment or blindness
- Reduced independence and quality of life
- Increased risk of falls or other injuries due to poor vision
Fortunately, healthcare advances mean blindness from cortical cataracts is largely preventable for people who have access to evaluation and surgery.
Preventing and Slowing the Progression of Cortical Cataracts
While aging is an inevitable risk factor, certain lifestyle habits and environmental strategies can help slow the development and progression of cortical cataracts:
- Consistent use of UV-protective sunglasses outdoors.
- Quitting smoking and avoiding tobacco exposure.
- Limiting alcohol consumption to moderate levels.
- Careful management of systemic diseases like diabetes.
- Regular comprehensive eye exams—especially after age 40.
- Healthy diet rich in antioxidants and nutrients beneficial to eye health.
There’s no proven way to entirely prevent all cataracts, but adopting these steps may minimize risk and delay the need for intervention.
Outlook and Prognosis
With timely detection and treatment, the vast majority of patients with cortical cataracts regain most, if not all, of their lost vision following cataract surgery. Outcomes are highly favorable, and surgery is considered one of the safest and most effective procedures in medicine. Early-stage patients often see meaningful improvement with lifestyle changes and vision correction, highlighting the value of regular eye checkups.
Frequently Asked Questions (FAQs) About Cortical Cataracts
Q: What are the first signs of a cortical cataract?
A: Patients typically notice blurry vision, greater difficulty seeing at night, increased glare (particularly from lights), and loss of color vibrancy. The condition often progresses painlessly and gradually.
Q: Can young people develop cortical cataracts?
A: While most common in older adults, anyone with significant eye trauma, underlying medical conditions (such as diabetes), radiation exposure, or genetic risk can develop cortical cataracts, even at a younger age.
Q: Are cortical cataracts reversible with medication?
A: Currently, there are no approved medications that reverse established cortical cataracts. Non-surgical approaches only help manage symptoms in early stages. Surgery is the definitive treatment for significant vision loss.
Q: Does cataract surgery cure cortical cataracts?
A: Yes. Surgery replaces the cloudy lens with a clear artificial one, typically restoring lost vision. The improvement is rapid and long-lasting for most patients.
Q: Is it possible to prevent cortical cataracts?
A: While not always preventable due to aging, practicing healthy habits (UV protection, avoiding smoking, managing diabetes, limiting alcohol) and having regular eye exams can slow progression and improve long-term visual outcomes.
Key Takeaways
- Cortical cataracts are a leading cause of age-related vision loss, caused by clouding of the lens cortex.
- Symptoms like blurry vision, increased glare, and color changes progress gradually over time.
- Diagnosis requires a comprehensive eye exam; treatment depends on severity.
- Preventive care and healthy lifestyle choices can slow progression, but surgery is highly effective if needed.
References
- https://www.medicalnewstoday.com/articles/cortical-cataracts
- https://www.healthline.com/health/eye-health/cortical-cataract
- https://eyewiki.org/Cataract
- https://resources.healthgrades.com/right-care/cataract-surgery/cortical-cataract
- https://bestcataractsurgeons.com/complete-guide-to-cortical-cataracts/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC1473213/
- https://www.medicalnewstoday.com/articles/posterior-subcapsular-cataract
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4097885/
- https://www.ncoa.org/article/cataracts-what-you-know-can-save-your-vision/
Read full bio of medha deb












