All About Coronary Steal Syndrome: Causes, Symptoms, Diagnosis, and Management
A comprehensive guide to understanding coronary steal syndrome, its causes, symptoms, diagnosis, treatment, and outlook.
All About Coronary Steal Syndrome
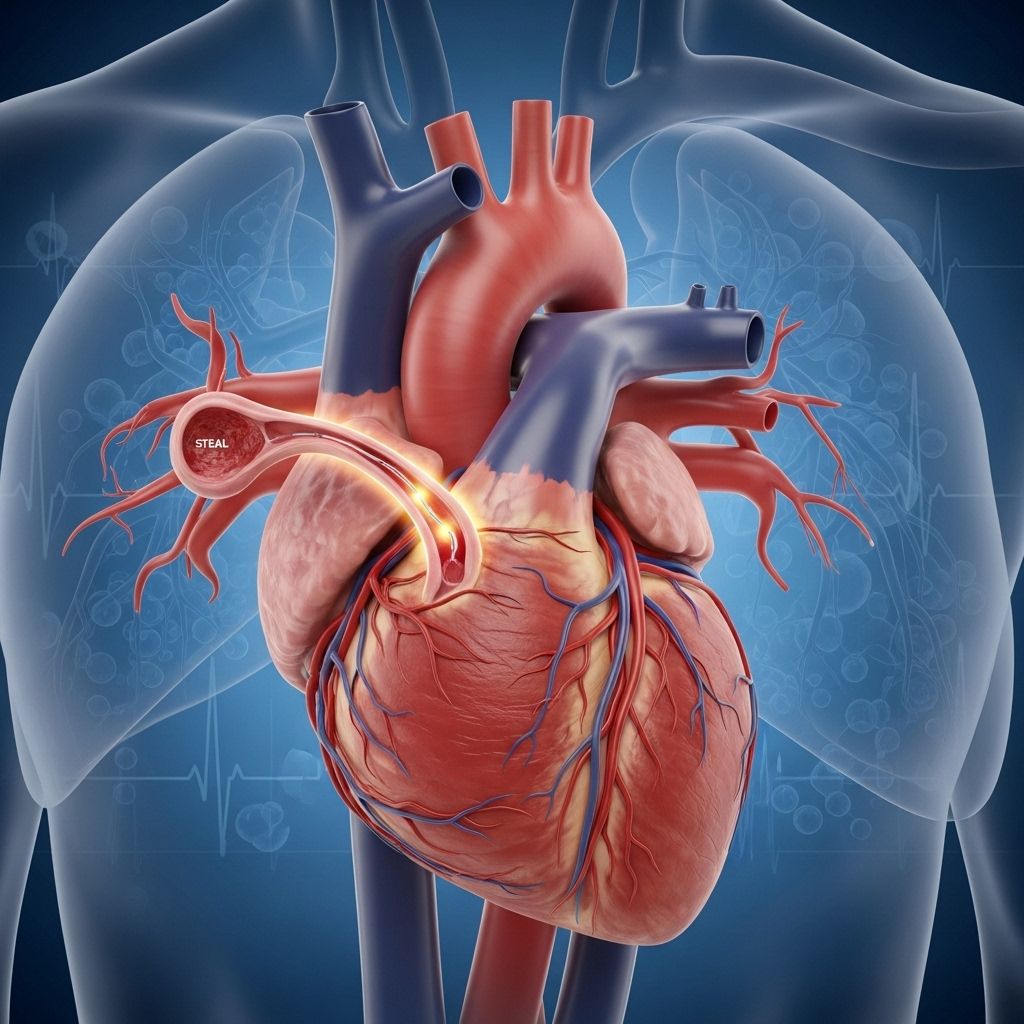
Coronary steal syndrome is a rare but important cardiovascular condition in which blood intended for a specific region of the heart is rerouted, or “stolen”, by other blood vessels. This disruption in normal blood flow can deprive heart tissue of oxygen, potentially causing chest pain and increasing the risk of heart attack. Understanding this phenomenon is crucial for patients, caregivers, and healthcare professionals alike.
Contents
- What Is Coronary Steal Syndrome?
- Types of Coronary Steal Syndrome
- Causes: Why Does Coronary Steal Happen?
- Symptoms: What to Watch For
- Diagnosis: How Is It Detected?
- Treatment Options
- Living and Coping with Coronary Steal Syndrome
- Outlook and Prognosis
- Frequently Asked Questions (FAQs)
What Is Coronary Steal Syndrome?
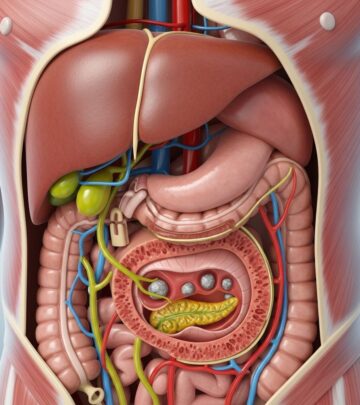
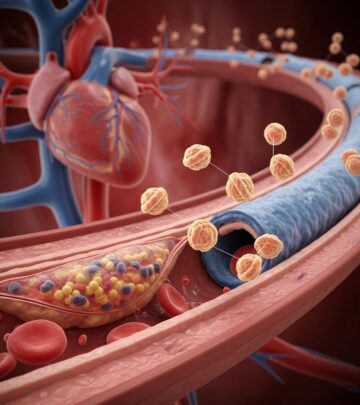
Coronary steal syndrome occurs when blood that would normally flow through a narrowed coronary artery is diverted to other blood vessels, depriving the affected part of the heart muscle of vital oxygen and nutrients. This “stealing” often results from differences in blood flow resistance between the arteries and can occur because of conditions that alter normal coronary circulation, such as medication use, surgery, or congenital abnormalities.
The phenomenon is called a “steal” because healthy blood vessels are dilated (opened), providing an easier alternative pathway for blood. This relatively lower resistance route draws blood away from already compromised heart regions, worsening their oxygen supply and potentially triggering symptoms or myocardial ischemia (insufficient blood flow to the heart muscle).
Types of Coronary Steal Syndrome
Several variations of coronary steal syndrome exist, each relating to different underlying conditions or triggers:
- Classic Coronary Steal: Blood is diverted from a stenotic (narrowed) artery to healthy vessels, often following medication use or collateral vessel formation.
- Post-surgical Steal: Can develop after coronary artery bypass grafting (CABG) if newly grafted vessels fail to supply adequate blood to the intended arteries.
- Congenital Steal: About 41% of cases are due to congenital heart disease, such as abnormal arterial-vein connections (arteriovenous fistulas), which can create new, unintended pathways for blood flow.
- Related Vascular Access Steal Syndromes: Variations can occur with subclavian or peripheral arteries, particularly where multiple vessels compete for blood supply.
Causes: Why Does Coronary Steal Happen?
Coronary steal syndrome is a consequence of abnormal blood flow dynamics within the heart, driven by one or more of the following mechanisms:
- Atherosclerosis: The most common cause, in which plaque buildup within coronary arteries narrows the passageway, predisposing to blood flow “stealing.”
- Vasodilator Drugs: Medications that widen blood vessels can unintentionally divert blood away from already narrowed arteries by opening healthy vessels further.
- Coronary Artery Bypass Grafting (CABG): Sometimes, bypass procedures do not restore optimal flow, or graft failure can create regions prone to steal.
- Congenital Heart Abnormalities: Structural defects such as arteriovenous fistulas increase the risk of steal by creating abnormal pathways that bypass normal arterial circulation.
- Peripheral Arterial Disease and Other Vascular Disorders: Conditions affecting arteries outside the heart, especially those supplying the arms or brain, can also create steal phenomena (such as subclavian steal syndrome).
Table: Main Causes and Contributing Factors
| Cause | Description |
|---|---|
| Atherosclerosis | Plaque buildup narrows arteries, impeding normal blood supply. |
| Vasodilator Medication | Widens blood vessels, diverting blood to less resistant paths. |
| CABG Surgery | Bypass grafts may not achieve intended blood flow distribution. |
| Congenital Abnormalities | Arteriovenous fistulas or abnormal arterial attachments create alternative pathways. |
| Peripheral and Subclavian Artery Disease | Can lead to related ‘steal’ syndromes outside the heart. |
Symptoms: What to Watch For
Symptoms of coronary steal syndrome may range from mild or unnoticed to severe and disabling. The chief symptom is usually chest pain (angina), especially during times when the heart’s demand for oxygen increases, such as physical activity or emotional stress.
Additional symptoms can include:
- Dizziness or lightheadedness
- Shortness of breath
- Fatigue or weakness
- Heart palpitations
- Flushing, headaches, and nausea
Certain related steal syndromes may cause other symptoms:
- Subclavian steal syndrome: Headaches, dizziness, and loss of vision
- Arterial or vascular access steal syndrome: Hand pain, differences in pulses, and blood pressure between arms
Often, symptoms are triggered or worsened by exertion, when the heart or affected area needs more blood than the altered vessels can deliver. In milder cases, symptoms may be absent or vague, delaying diagnosis.
Diagnosis: How Is It Detected?
Coronary steal syndrome can be challenging to identify because its symptoms overlap with many other cardiac and vascular disorders. Diagnosis typically involves a combination of clinical evaluation and imaging tests.
Key diagnostic strategies include:
- Cardiac Stress Test (with or without exercise): Detects reduced blood flow or chest pain (ischemia) as heart demand increases.
- Vasodilator Challenge: Administered during a stress test to provoke symptoms by widening vessels and observing “steal” effects.
- Coronary Angiography: Injection of contrast dye into coronary arteries, visualized with X-rays, to identify blockages and abnormal flow.
- Computed Tomography (CT) Scan: Produces cross-sectional images to map arterial blockages and flow patterns.
- Doppler Ultrasound: Uses sound waves to check for reversed or abnormal blood flow, especially in subclavian arteries.
- Positron Emission Tomography (PET) Scan: Measures blood flow after administering radioactive tracers.
For a suspected case, doctors may order multiple tests to confirm coronary steal syndrome and rule out other cardiac problems.
Treatment Options
Treatment aims to restore balanced blood flow to the heart muscle and alleviate symptoms, depending on the severity, underlying cause, and the presence of risk factors.
Common Treatment Options
- Medication Adjustments: Discontinuing or changing vasodilators if implicated in worsening symptoms.
- Anti-anginal Therapy: Using medicines, such as nitrates or beta-blockers, to manage chest pain and lower heart workload.
- Management of Risk Factors: Controlling cholesterol, blood pressure, diabetes, and eliminating smoking.
- Surgical Intervention: Surgery or minimally invasive procedures might be needed to bypass or open blocked arteries (angioplasty, CABG, or repair of congenital vessels).
- Endovascular Procedures: Placement of a stent or coil to close abnormal vessels (e.g., arteriovenous fistulas).
The choice of treatment is tailored based on the individual’s anatomy, severity of symptoms, comorbidities, and risk of complications.
Living and Coping with Coronary Steal Syndrome
Living with coronary steal syndrome involves not only acute treatment, but also ongoing management and lifestyle adaptations to protect heart health. This includes:
- Regular follow-up: Routine visits to your cardiologist to monitor heart function and detect new or worsening symptoms early.
- Adherence to Medication: Taking prescribed medications diligently and reporting side effects promptly.
- Lifestyle Modifications:
- Maintaining a heart-healthy diet (low in saturated fats and sodium)
- Engaging in doctor-approved physical activity
- Managing stress through relaxation techniques or counseling
- Quitting smoking and limiting alcohol
- Controlling weight, blood pressure, cholesterol, and diabetes
- Recognizing Warning Signs: Seeking medical attention for sudden or worsening chest pain, severe shortness of breath, or fainting spells.
Outlook and Prognosis
The long-term outlook for people with coronary steal syndrome varies based on the cause, the speed and success of treatment, and overall cardiac health. Many people respond well to treatment, especially when the underlying blockage or abnormality can be corrected or effectively managed.
If left untreated or unrecognized, severe coronary steal syndrome can increase the risk of complications such as heart attack or chronic heart failure. Early diagnosis, careful management, and attention to heart-healthy living are crucial to maintaining the best possible outcome.
Frequently Asked Questions (FAQs)
Q: What is the main difference between coronary steal syndrome and subclavian steal syndrome?
A: Coronary steal syndrome affects blood flow within the heart, while subclavian steal syndrome occurs when blood is diverted from brain circulation to the arm due to subclavian artery narrowing. Both involve blood being “stolen” from its intended destination, usually due to arterial blockages but impact different organs.
Q: Is coronary steal syndrome reversible?
A: In many cases, restoring arterial flow through surgery, stenting, or treating the underlying issue can reverse symptoms. Effectiveness depends on the underlying cause and timely intervention.
Q: Can lifestyle changes alone fix coronary steal syndrome?
A: Lifestyle changes are important for long-term heart health and may reduce risk factors but cannot always fix anatomic or mechanical causes such as artery blockages or congenital vessel abnormalities. Medical or surgical treatment is often required for significant cases.
Q: How common is coronary steal syndrome?
A: Coronary steal syndrome is considered rare. However, related “steal” syndromes, such as subclavian steal, occur more frequently in people with significant atherosclerosis or previous vascular procedures, especially those aged over 55 or with other heart or vascular risk factors.
Q: What are the warning signs that should lead to urgent medical attention?
A: New, severe, or persistent chest pain (especially at rest), fainting, severe shortness of breath, or neurological symptoms such as vision loss or limb weakness warrant immediate medical evaluation.
References
- Information summarized and adapted from Healthline, Cleveland Clinic, GetLabTest, and Thoracic Key resources on coronary steal and related syndromes.
References
- https://www.getlabtest.com/news/post/understanding-coronary-steal-syndrome
- https://www.healthline.com/health/heart/all-about-coronary-steal-syndrome
- https://my.clevelandclinic.org/health/diseases/subclavian-steal-syndrome
- https://thoracickey.com/steal-syndromes-2/
- https://www.osmosis.org/learn/Coronary_steal_syndrome
- https://www.ahajournals.org/doi/10.1161/JAHA.121.021000
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4020528/
- https://pubmed.ncbi.nlm.nih.gov/37264699/
Read full bio of medha deb