Coronary Heart Disease vs. Coronary Artery Disease: Understanding the Similarities and Key Differences
Unraveling the similarities and distinctions between coronary heart disease and coronary artery disease to empower your heart health decisions.
Coronary heart disease (CHD) and coronary artery disease (CAD) are among the most common terms used when discussing conditions related to the heart and its blood supply.
While these terms are often used interchangeably in medical settings, understanding their distinctions, types, causes, symptoms, risk factors, and treatments can help you make more informed choices for your heart health.
Overview
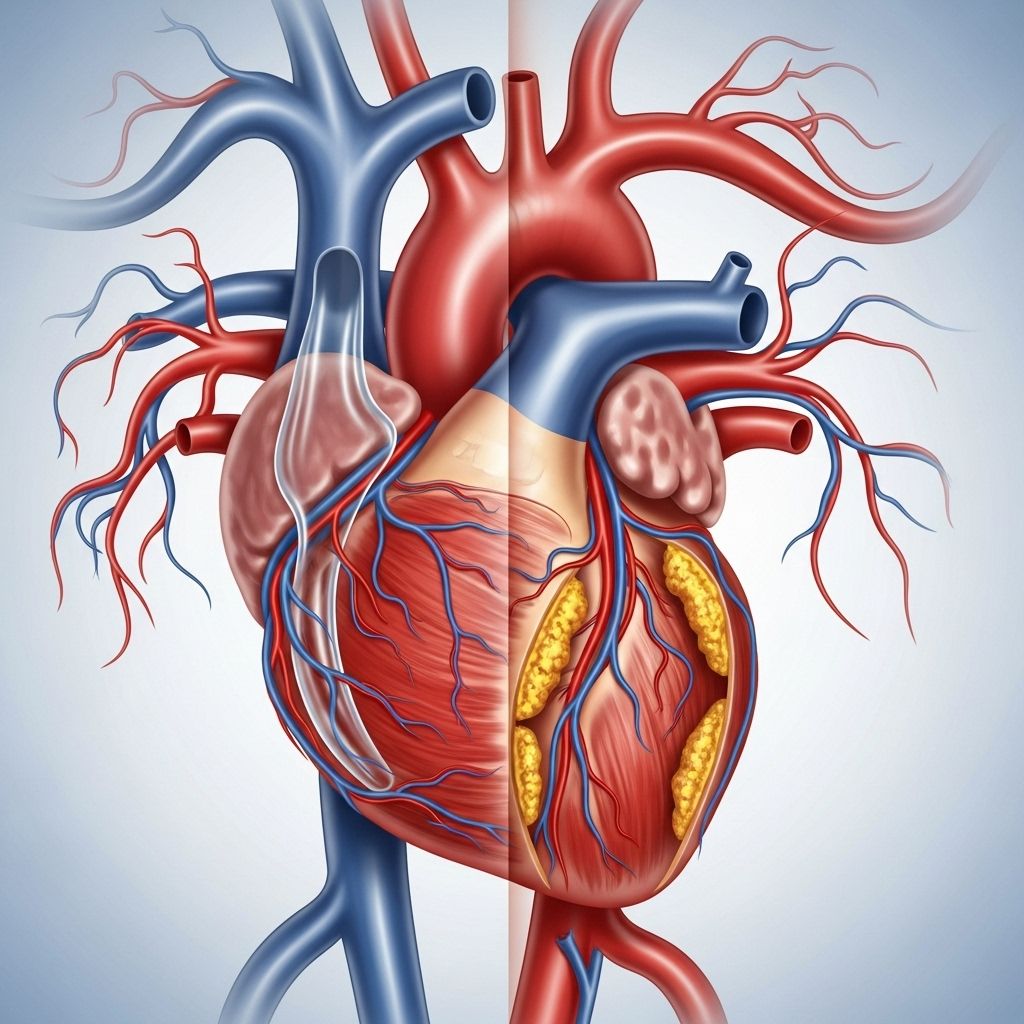
Both CHD and CAD involve the buildup of plaque in the arteries that supply oxygen-rich blood to the heart muscle. This process, called atherosclerosis, can narrow or block arteries, leading to a reduction in blood flow. Insufficient blood supply can eventually result in conditions such as angina (chest pain), heart attacks, or even heart failure.
- Coronary artery disease (CAD): An umbrella term that refers to all disorders resulting from plaque buildup in the coronary arteries, including CHD and other related conditions.
- Coronary heart disease (CHD): A type of CAD specifically characterized by the direct effect of plaque buildup on the heart, usually leading to issues like heart attacks and angina.
Below, we break down these conditions further, examining their overlap, unique features, and the latest recommendations for risk reduction and management.
What is Coronary Artery Disease (CAD)?
CAD is the most common type of heart disease globally and the leading cause of heart attacks. It develops when one or more of the major blood vessels that supply your heart (the coronary arteries) become damaged or diseased due to a buildup of fatty deposits or plaques.
- Atherosclerosis: The central process in CAD, where cholesterol and other substances accumulate in artery walls and form plaques. This narrows the arteries over time and restricts blood flow to heart tissue.
- As plaque accumulates, it can also rupture. This triggers the formation of blood clots that can further slow or block blood flow, potentially causing a heart attack.
When blood flow to the heart muscle is reduced or blocked, the heart may become starved of oxygen and nutrients, resulting in pain or serious injury to heart tissue.
Key Facts about CAD:
- This disease often develops over many years, sometimes beginning in childhood.
- Many people may not notice symptoms until the disease is very advanced or until a heart attack occurs.
What is Coronary Heart Disease (CHD)?
CHD is a condition directly stemming from CAD. It specifically describes what happens when the heart’s blood supply is restricted due to plaque buildup in the coronary arteries. Essentially:
- All cases of CHD are forms of CAD.
- CHD may be considered the clinical outcome of CAD when blood supply to the heart is seriously impaired.
- CHD commonly manifests as angina (chronic chest pain) or heart attacks (acute events).
Key Difference Table: CHD vs CAD
| Aspect | Coronary Artery Disease (CAD) | Coronary Heart Disease (CHD) |
|---|---|---|
| Definition | Buildup of plaque in coronary arteries, restricting blood flow to the heart muscle | Clinical consequence of CAD where the heart’s function or tissue is impaired |
| Scope | Umbrella term; includes all disorders of coronary artery plaque buildup | Specific result of CAD affecting heart health, often with symptoms |
| Symptoms | Possible angina, shortness of breath; may be asymptomatic for years | Usually angina, heart attack, heart failure |
| Usage | Describes the disease process | Describes the clinical outcome on the heart |
Types of Coronary Artery Disease
CAD can manifest in several distinct patterns, each affecting heart health differently. The main types include:
- Stable Ischemic Heart Disease: Reduced blood flow causes predictable chest pain, usually during exertion or stress.
- Acute Coronary Syndrome (ACS): An umbrella term that includes conditions such as unstable angina and heart attacks, which result from sudden and severe reductions in blood flow.
- Silent Ischemia: Loss of blood flow to heart tissue without noticeable symptoms, often uncovered only through medical testing.
Signs and Symptoms
Symptoms for CHD and CAD are closely related. People may experience some or all of the following:
- Angina: Chest pain or discomfort, often described as a squeezing, pressure, or heaviness in the chest. It might also radiate to the arms, neck, jaw, or back.
- Shortness of breath: Especially during physical activity or stress.
- Fatigue: Unusual tiredness may develop, particularly with activity.
- Heart attack: In some cases, the first sign of CAD or CHD is a heart attack, with symptoms including:
- Pain or pressure in the chest
- Pain in the arms, back, neck, jaw, or stomach
- Shortness of breath
- Nausea or vomiting
- Cold sweats
- Lightheadedness or dizziness
Note: Some people, particularly women and older adults, may experience atypical or mild symptoms, making diagnosis more challenging.
Causes and Risk Factors
The primary underlying cause of CAD and CHD is atherosclerosis—the accumulation of cholesterol-rich deposits (plaques) on the inner walls of coronary arteries. Over time, this leads to narrowed arteries and diminished blood supply to the heart muscle.
Major Risk Factors
- High LDL (“bad”) cholesterol
- Low HDL (“good”) cholesterol
- High blood pressure (hypertension)
- Diabetes or insulin resistance
- Obesity or being overweight
- Smoking
- Family history of heart disease
- Age: Increased risk for men after 45, for women after 55
- Physical inactivity
- Poor dietary habits (high saturated fat, salt, sugar)
- Excessive alcohol consumption
- Chronic stress
Notably, many individuals have more than one risk factor, and cumulative risks can greatly increase the chance of developing CHD or CAD. Multiple studies also show that atherosclerosis can begin in childhood, highlighting the importance of early prevention.
Diagnosis of CAD and CHD
Your healthcare provider may use several tests to evaluate for CAD or CHD. These can include:
- Electrocardiogram (ECG or EKG): Measures the electrical activity of the heart to detect signs of ischemia or heart attack
- Stress tests: Assesses the heart’s function and blood supply under physical exertion
- Coronary angiography: Uses X-ray imaging and contrast dye to visualize blockages in coronary arteries
- CT and MRI scans: Provide detailed images of the heart and its blood vessels
- Blood tests: Measure cholesterol and other markers of heart disease risk
Treatment Options
The goal of treating CAD and CHD is to improve blood flow to the heart muscle, reduce symptoms, and lower the risk of future events like heart attacks. Treatment plans are usually tailored to the individual and may include lifestyle changes, medications, and sometimes surgical procedures.
Lifestyle Modifications
- Heart-healthy diet: Emphasize fruits, vegetables, whole grains, lean proteins, and healthy fats; minimize saturated and trans fats, salt, and added sugars.
- Regular physical activity: Aim for at least 150 minutes of moderate aerobic exercise per week.
- Weight management: Achieve and maintain a healthy weight.
- Smoking cessation: Quitting smoking rapidly reduces risk.
- Stress reduction: Practice relaxation techniques, such as meditation or yoga.
Medications
- Antiplatelet drugs (e.g., aspirin): Reduce the risk of blood clots in arteries.
- Statins: Lower LDL cholesterol.
- Beta-blockers: Reduce heart rate and blood pressure.
- ACE inhibitors/ARBs: Lower blood pressure, reduce strain on the heart.
- Nitrates: Help dilate blood vessels and relieve angina symptoms.
- Diabetes management medications: Essential for those with diabetes.
Surgical and Interventional Procedures
- Angioplasty and stenting: A catheter is used to open blocked arteries and insert a stent to keep them open.
- Coronary artery bypass graft (CABG) surgery: Healthy arteries or veins from elsewhere in the body are used to bypass blocked coronary arteries.
Prevention Tips
Preventing coronary artery disease and coronary heart disease relies on proactive lifestyle measures, risk factor awareness, and regular health check-ups. Here are key strategies:
- Eat a balanced, nutrient-rich diet rich in plant foods.
- Engage in moderate-intensity exercise most days of the week.
- Quit smoking and avoid secondhand smoke.
- Manage chronic health conditions like diabetes and high blood pressure.
- Keep cholesterol and triglyceride levels in a healthy range.
- Manage stress through healthy coping mechanisms.
- Maintain a healthy weight.
- Limit alcohol consumption.
Frequently Asked Questions (FAQs)
Are coronary artery disease and coronary heart disease the same thing?
No, but they are closely related. Coronary artery disease (CAD) refers to the underlying process of plaque buildup in coronary arteries, while coronary heart disease (CHD) specifically describes the consequences of that buildup—the effects on the heart, such as chest pain or heart attack. In practice, the terms are often used interchangeably by healthcare professionals due to their close association.
What puts me most at risk for developing CAD?
Major risk factors include high LDL cholesterol, high blood pressure, diabetes, smoking, obesity, family history, older age, and physical inactivity.
What are typical warning signs of a heart attack?
The most common warning signs are chest pain or discomfort, shortness of breath, pain radiating to the shoulder, arm, back, or jaw, nausea, lightheadedness, or breaking out in a cold sweat. These symptoms require immediate medical attention.
Can coronary artery disease be reversed?
While advanced plaque buildup (atherosclerosis) is generally not reversible, lifestyle changes and management of risk factors can slow progression, stabilize plaques, and sometimes even partially reduce them, especially when aggressively managing cholesterol through statins and other measures.
When should I see a doctor?
If you have risk factors for heart disease, experience chest pain, shortness of breath, or other concerning symptoms, schedule an appointment for evaluation. Emergency medical help should be sought immediately if you suspect a heart attack.
Takeaway
Understanding the distinctions and similarities between coronary artery disease and coronary heart disease empowers you to better monitor your heart health and work with your healthcare provider on prevention, diagnosis, and effective treatment strategies. Maintaining a heart-healthy lifestyle remains your best defense against both conditions.
References
- https://www.usavascularcenters.com/blog/heart-disease-vs-arterial-disease-whats-difference/
- https://www.healthline.com/health/heart-health/coronary-heart-disease-vs-coronary-artery-disease
- https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease/coronary-artery-disease
- https://www.mayoclinic.org/diseases-conditions/coronary-artery-disease/symptoms-causes/syc-20350613
- https://www.cdc.gov/heart-disease/about/coronary-artery-disease.html
- https://www.nhlbi.nih.gov/sites/default/files/publications/FactSheetKnowDiffDesign2020V4a.pdf
- https://www.nhlbi.nih.gov/resources/know-differences-cardiovascular-disease-heart-disease-coronary-heart-disease
- https://www.nhs.uk/conditions/coronary-heart-disease/
- https://ufhealth.org/conditions-and-treatments/coronary-heart-disease
Read full bio of Sneha Tete












