Coronary Artery Dissection (SCAD): Causes, Symptoms, and Treatment
Understanding SCAD: symptoms, diagnosis, treatment options, and outlook for this rare, often misdiagnosed heart condition.
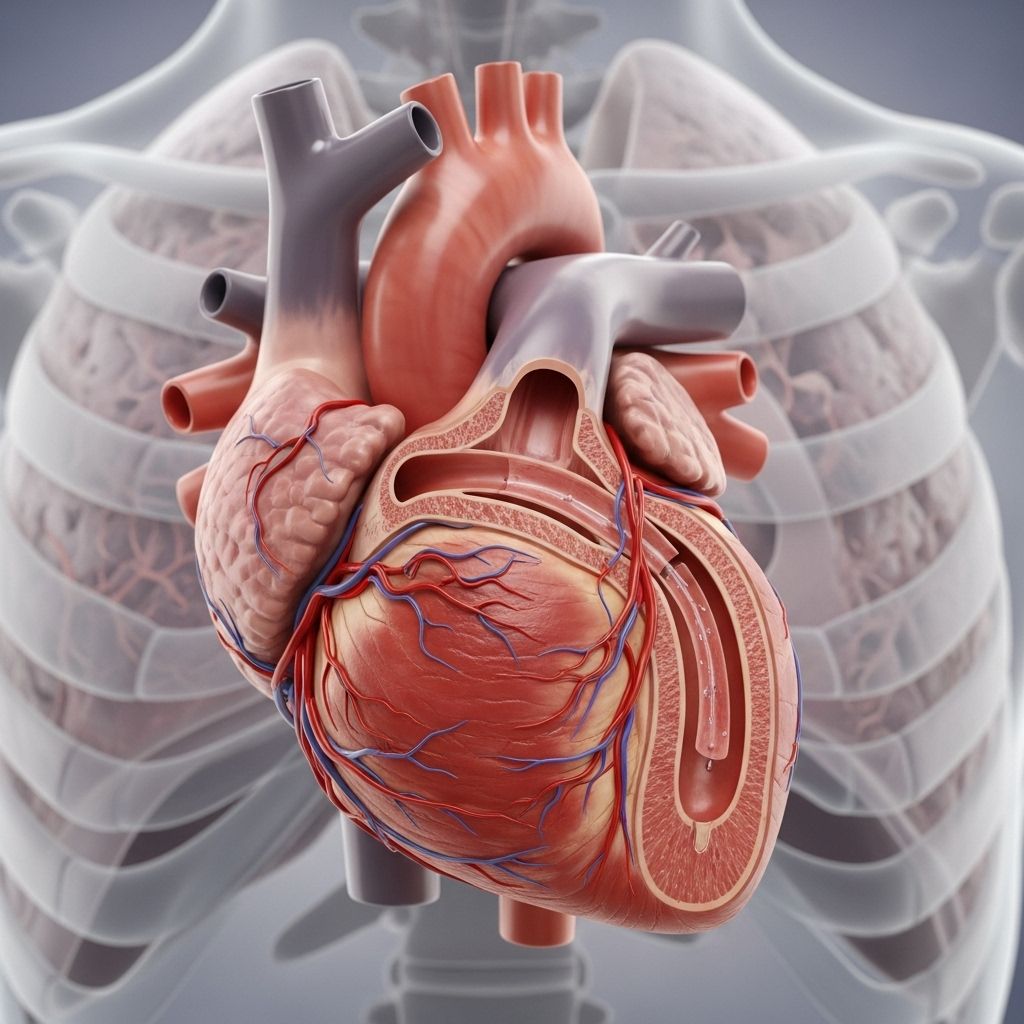
Spontaneous coronary artery dissection (SCAD) is a rare yet serious condition involving a tear or separation in the layers of a coronary artery wall. This event can restrict blood flow to the heart, potentially triggering a heart attack, a major cardiac emergency, or even sudden cardiac death. Despite its seriousness, SCAD is frequently misdiagnosed, largely because its symptoms often mimic those of a typical heart attack and because it commonly occurs in people not considered at high risk for heart disease.
Understanding SCAD
SCAD disrupts one or more of the three layers of a coronary artery. When a tear occurs, blood seeps between the layers, forming a blockage that can partially or completely restrict blood flow. This is distinct from blockages caused by cholesterol-rich plaques seen in traditional coronary artery disease. SCAD’s unique features mean timely recognition, accurate diagnosis, and appropriate management are critical for improving patient outcomes.
- SCAD most often affects:
- Women (especially under age 50)
- Postpartum individuals (weeks or months after childbirth)
- People with few or no typical heart disease risk factors
Symptoms of SCAD
SCAD typically presents with symptoms very similar to a heart attack, which may include:
- Chest pain — pressure, tightness, heaviness, or discomfort
- Rapid heartbeat or palpitations
- Pain or discomfort radiating to the arms, shoulders, jaw, neck, back, or stomach
- Shortness of breath or difficulty breathing
- Excessive sweating (cold sweat or clamminess)
- Nausea or vomiting
- Dizziness or lightheadedness
- Unusual or extreme fatigue
- Fainting or loss of consciousness
- Headache (less common)
These symptoms may develop suddenly and should be taken seriously. If you or someone you know experiences these warning signs, seeking immediate medical attention is critical.
Who Is at Risk?
While the exact cause of SCAD remains unclear, certain risk factors and associations have been identified:
- Female sex — About 90% of cases occur in women
- Age — Most patients are between 30 and 50 years old
- Postpartum period — The risk is higher after childbirth, especially in the first several months
- Fibromuscular dysplasia (FMD) — A condition that causes abnormal growth in artery walls
- Connective tissue disorders — Such as Marfan syndrome or Ehlers-Danlos syndrome
- Extreme emotional or physical stress
- Intense exercise
- Hormonal changes or use of oral contraceptives
- Other vascular conditions — Including certain autoimmune or inflammatory diseases
Unlike atherosclerotic heart disease, traditional risk factors such as high cholesterol, high blood pressure, or smoking are less frequently found in people who experience SCAD.
Causes and Triggers of SCAD
SCAD occurs when one of the three layers of a coronary artery wall develops a tear (dissection), which allows blood to pool and form a blockage. The causes are multifactorial and not fully understood but can include:
- Genetic predisposition — Family history may play a role
- Hormonal influences — Including those of pregnancy, childbirth, or hormonal therapy
- Underlying vascular diseases
- Severe emotional or physical stress — Such as intense exercise, labor and delivery, or extreme grief
- Unknown/idiopathic — In several cases, no clear trigger can be identified
It’s important to note that SCAD is not caused by lifestyle factors or blockages from cholesterol plaques, distinguishing it from more common forms of heart disease.
How Is SCAD Diagnosed?
Diagnosing SCAD can be challenging because it often affects people not considered at risk for heart disease and because its symptoms mimic other cardiac conditions. The diagnostic process may involve:
- Medical history and physical exam
- Electrocardiogram (ECG or EKG): Records the heart’s electrical activity. May reveal patterns consistent with a heart attack, but sometimes can be normal in SCAD patients.
- Blood tests: Especially for Troponin levels, a protein released when the heart muscle is damaged.
- Coronary angiogram: An imaging procedure using dye and X-rays to visualize coronary arteries and identify tears or blockages.
- Non-invasive imaging: May include computed tomography (CT) angiography or magnetic resonance imaging (MRI) if a coronary angiogram is deemed unsafe (e.g., during pregnancy).
- Advanced imaging: Specialized techniques like optical coherence tomography (OCT) or intravascular ultrasound (IVUS) can provide detailed images of artery walls and confirm the diagnosis.
- Echocardiogram: An ultrasound of the heart used to assess its function and identify potential complications.
It’s very important that SCAD is considered in patients, especially young or middle-aged women, who present with heart attack symptoms without traditional risk factors. Delayed or missed diagnosis can lead to poorer outcomes or recurrent episodes.
Treatment Options for SCAD
There is no single standard treatment for SCAD; management depends on the extent of the artery dissection, the area of the heart affected, and the patient’s symptoms. The main goals are to restore and maintain blood flow, support cardiac function, and reduce the risk of recurrence.
Acute Phase Care
- Hospitalization: Most patients are admitted and closely monitored, especially in the first 5 days after diagnosis when the risk of recurrence is highest.
- Medications: May include:
- Aspirin and other antiplatelet drugs — to reduce blood clot formation
- Beta-blockers — to reduce heart workload and lower the risk of future events
- Statins: In select cases, but not always required unless there’s coexisting cholesterol disease
- Other medications: To manage symptoms or underlying conditions
- Revascularization (rare, for select cases):
- Percutaneous coronary intervention (PCI) or bypass surgery — only if blood flow is severely compromised and symptoms cannot be managed by medications. These procedures carry additional risks in SCAD and are only performed if absolutely needed.
Long-Term Management
- Heart-healthy lifestyle:
- Regular follow-up with a cardiologist
- Gradual return to physical activity as recommended by your care team
- Avoiding extreme physical or emotional stress when possible
- Managing other risk factors (blood pressure, diabetes, etc.) if present
- Cardiac rehabilitation: A supervised program with tailored exercise, education, and emotional support can be beneficial for recovery and confidence.
- Support for mental health: Anxiety, depression, or trauma symptoms are common after a SCAD event. Access to psychological support or counseling is recommended.
What Is the Outlook for People With SCAD?
Most people recover well after a SCAD event, but ongoing follow-up is essential because:
- There is a risk of recurrence (approximately 15–30% may experience another SCAD episode over their lifetime).
- Heart function and degree of artery healing will determine individual recovery and activity levels.
- Early and accurate diagnosis, appropriate treatment, and comprehensive follow-up care are key to the best possible outcome.
SCAD vs. Traditional Heart Attack: Key Differences
| Feature | SCAD | Typical Heart Attack (Atherosclerotic) |
|---|---|---|
| Main Cause | Arterial wall tear, spontaneous | Plaque buildup, artery narrowing (atherosclerosis) |
| Patient Profile | Often young/middle-aged women, postpartum | Often older adults, both genders, traditional risk factors |
| Symptoms | Chest pain, shortness of breath, similar to heart attack | Chest pain, shortness of breath, similar presentation |
| Treatment | Mainly medical management, monitored recovery, revascularization only if needed | Frequent use of stents, bypass, and aggressive cholesterol management |
| Recurrence | Risk remains, especially in early months/years | Risk reduced with ongoing risk factor control |
Tips for Coping and Living With SCAD
- Build a strong partnership with your healthcare team; attend all follow-up appointments.
- Participate in cardiac rehabilitation if recommended.
- Reach out to SCAD support groups or communities for emotional connection and practical advice. Shared experiences can help reduce anxiety and support long-term well-being.
- Be aware of the symptoms of recurrence, and seek immediate care if they develop.
- Communicate any changes in physical or emotional health to your care providers.
Frequently Asked Questions (FAQs)
What triggers a SCAD event?
SCAD can occur spontaneously, but common triggers include extreme physical or emotional stress, intense exercise, childbirth, or underlying vascular disorders. In many cases, no obvious trigger is identified.
Is SCAD the same as a heart attack?
SCAD is a cause of heart attack — particularly in young and middle-aged women who do not have traditional risk factors. While the symptoms are similar, the underlying mechanism (artery wall tear) is different from cholesterol plaque blockages seen in most heart attacks.
How is SCAD different from coronary artery disease?
Coronary artery disease typically involves atherosclerosis (plaque buildup narrowing arteries). SCAD is caused by a tear or separation in the artery wall, not by plaque deposits. This distinction is important for appropriate treatment.
Can SCAD recur?
Yes. About 15–30% of people with SCAD experience another episode, especially during the early months or years after the initial event. Careful follow-up and management are crucial to reduce risks.
What are the chances of full recovery?
Most people with SCAD can return to normal activities over time, though recovery speed and extent depend on the severity of the initial event and heart function. Cardiac rehabilitation and psychological support can improve confidence and quality of life.
What should I do if I think I’m having SCAD?
Call emergency services immediately. Early treatment is key to minimizing heart damage and improving the outlook. Do not try to drive yourself to the hospital if symptoms are severe.
Additional Resources
- Speak to your healthcare provider for referral to a specialist in SCAD if you have questions or concerns.
- Check for SCAD community resources or patient advocacy organizations for support.
References
- https://www.heartandstroke.ca/heart-disease/conditions/spontaneous-coronary-artery-dissection
- https://beatscad.org.uk/SCAD-for-Patients/Symptoms-and-Diagnosis
- https://www.rwjbh.org/treatment-care/heart-and-vascular-care/diseases-conditions/spontaneous-coronary-artery-dissection/
- https://stanfordhealthcare.org/medical-conditions/blood-heart-circulation/spontaneous-coronary-artery-dissection/symptoms.html
- https://my.clevelandclinic.org/health/diseases/17503-spontaneous-coronary-artery-dissection-scad
- https://www.heart.org/en/health-topics/heart-attack/about-heart-attacks/coronary-artery-dissection-not-just-a-heart-attack
- https://www.svhhearthealth.com.au/conditions/spontanous-coronary-artery-dissection
- https://www.bhf.org.uk/informationsupport/conditions/spontaneous-coronary-artery-dissection
Read full bio of medha deb












