Understanding Constipation After Diarrhea: Causes, Treatments, and Prevention
Explore the causes and solutions for experiencing constipation after a bout of diarrhea, including tips for prevention and management.
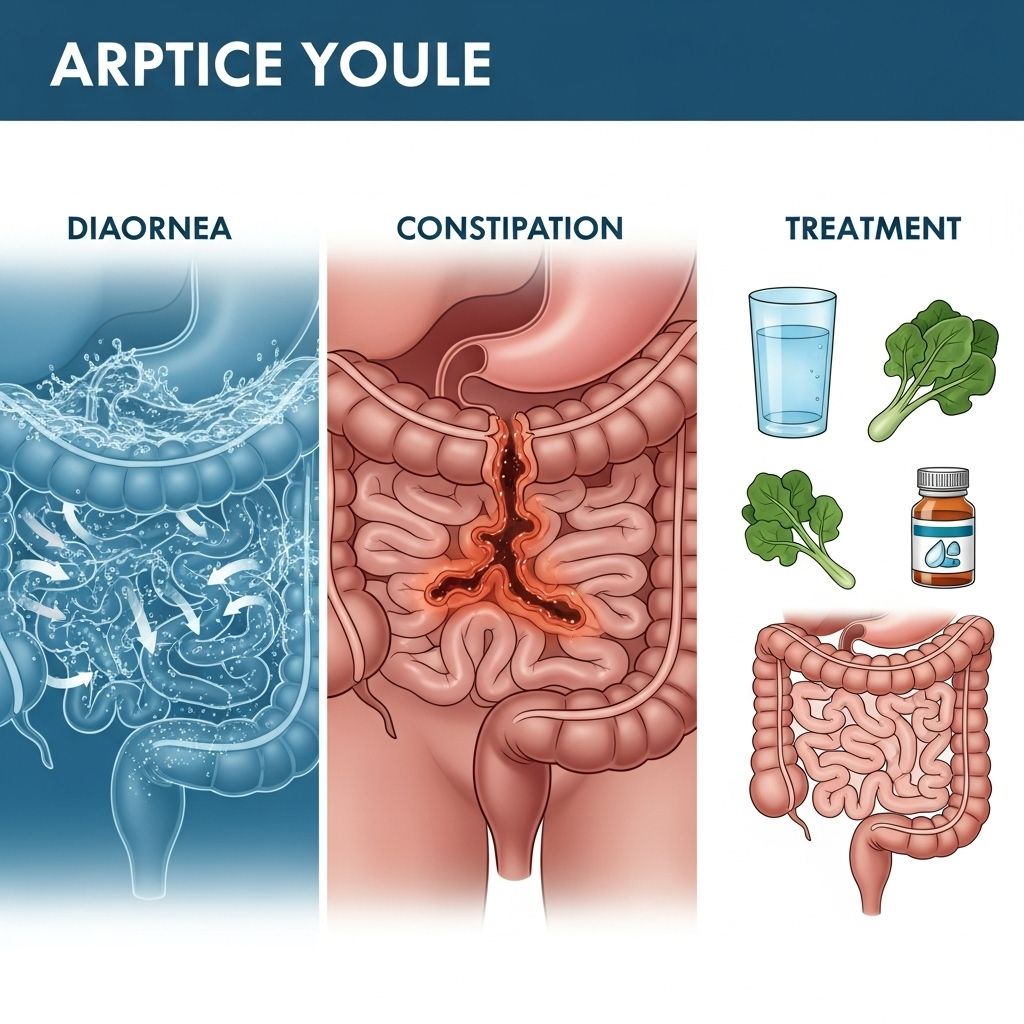
Constipation After Diarrhea: Understanding the Digestive Shift
It might seem paradoxical, but moving from one digestive extreme to another—experiencing constipation after a bout of diarrhea—is a surprisingly common phenomenon. This transition can feel confusing and uncomfortable, but understanding the underlying causes and knowing how to respond can help you manage symptoms and maintain gastrointestinal health. This comprehensive guide covers the reasons behind this shift, symptom patterns, prevention tips, treatment options, and much more.
What Does It Mean to Have Constipation After Diarrhea?
**Constipation after diarrhea** means your bowel movements shift from being unusually loose or frequent to becoming infrequent, hard, or difficult to pass. While these symptoms may seem unrelated, there are several common mechanisms and factors that can cause this pattern.
- Diarrhea typically involves watery or loose stools and may occur several times a day.
- Constipation involves difficulty passing stools, infrequent bowel movements (often fewer than three per week), or stools that are hard, dry, and lumpy.
Transitioning from diarrhea to constipation can be caused by a variety of factors, including infections, medications, dietary changes, or underlying digestive conditions.
Common Causes of Constipation After Diarrhea
Several situations can explain why constipation sometimes follows diarrhea. Understanding the possible causes can help you and your healthcare provider identify the best treatment approach.
1. Changes in Diet or Fluid Intake
- Recovering from diarrhea might lead you to change your diet—such as eating less, avoiding certain foods, or following a bland diet. Some people may inadvertently reduce their fiber or fluid intake, which can contribute to constipation.
- Trying the BRAT diet (bananas, rice, applesauce, toast), while helpful for settling an upset stomach, can sometimes result in harder stools if followed for an extended period.
2. Medications
- Some anti-diarrheal medications (like loperamide) work by slowing down gut movement, potentially resulting in constipation if overused.
- Painkillers, antacids containing calcium or aluminum, antidepressants, and iron supplements can also cause constipation.
3. Digestive System Adjustment
After an episode of diarrhea, the intestines and colon may need time to return to normal function. During recovery, the bowel can temporarily slow down, leading to constipation.
4. Stomach or Gut Infections
- Stomach bugs (viral or bacterial infections) can initially cause diarrhea by irritating the lining of the gut.
- After the infection subsides, the digestive system may slow down, sometimes swinging to constipation as a result of inflammation or changes in gut bacteria.
Other infection symptoms might include:
- Fever
- Loss of appetite
- Chills or body aches
- Vomiting
- Abdominal pain
5. Underlying Digestive Disorders
Frequent transitions between diarrhea and constipation can signal a more persistent underlying condition.
• Irritable Bowel Syndrome (IBS)
- IBS, especially the mixed type (IBS-M), can cause alternating symptoms of diarrhea and constipation.
- Symptoms may include abdominal pain, fatigue, bloating, gas, and mucus in the stool.
- Triggers can be stress, dietary sensitivities, or gut microbiome shifts.
• Inflammatory Bowel Disease (IBD)
- IBD, such as Crohn’s disease or ulcerative colitis, refers to autoimmune-driven inflammation of the digestive tract.
- Chronic inflammation may lead to fluctuating bowel movements, including bouts of diarrhea followed by constipation.
- Additional symptoms: persistent abdominal pain, rectal bleeding, weight loss, and fatigue.
6. Paradoxical (Overflow) Diarrhea
This occurs when liquid stool leaks around a hardened mass of feces in the colon—mimicking diarrhea despite underlying constipation.
- More common in chronic constipation or severe blockage (fecal impaction).
- Often seen in older adults or people with neurological or mobility issues.
Symptoms Associated with Shifts from Diarrhea to Constipation
The transition between diarrhea and constipation involves several distinctive symptoms. Being aware of these can help clarify what you’re experiencing.
- Sudden change in stool frequency or consistency
- Sense of incomplete evacuation (not feeling ‘done’ after a bowel movement)
- Dark, hard, dry stools after runny or loose ones
- Bloating, abdominal pain, or discomfort
- Feeling of fullness, nausea, or loss of appetite
- Straining during bowel movements
- Possible blood or mucus in stool (see a doctor if present)
Why Does This Happen? Exploring the Physiology
The digestive tract is a coordinated, muscular tube that moves food and waste through complex patterns of contraction and relaxation. Both diarrhea and constipation occur when these rhythms are disrupted:
- Diarrhea: Intestinal contents move too quickly for water to be absorbed, resulting in liquid stools.
- Constipation: Contents move too slowly, allowing more water to be absorbed and resulting in drier, harder stools.
A bout of diarrhea can temporarily disturb the gut’s natural bacteria (the microbiome) and inflammation in the gut wall may slow transit time as healing occurs, leading to a period of constipation.
Risk Factors for Experiencing Both Constipation and Diarrhea
- Preexisting digestive disorders (IBS, IBD, chronic constipation)
- Older age
- Recent or frequent use of antibiotics
- Dietary changes or poor hydration
- Medications that affect gut motility
- Psychological stress
Diagnosing the Underlying Cause
If you experience recurring patterns of alternating constipation and diarrhea, it’s essential to identify any underlying conditions. Your healthcare provider may recommend:
- Medical history review and symptom journaling
- Physical examination
- Blood or stool tests to check for infections or inflammation
- Colonoscopy or imaging studies for persistent or severe cases
- Food diary to track potential dietary triggers
How to Treat Constipation After Diarrhea
Treatment strategies depend on the cause, frequency, and severity of your symptoms. Most occasional cases can be managed at home, but persistent or severe symptoms need medical attention.
General Management and Home Remedies
- Hydrate: Drink plenty of water and clear fluids, such as herbal teas or broths, to prevent further dehydration and help the colon soften stools.
- Gradually reintroduce fiber: Once diarrhea resolves, gradually add soluble fiber (oats, bananas, applesauce) to bulk and soften stools. Avoid excess fiber too soon if the digestive tract is still sensitive.
- Gentle movement: Light activity, such as walking, can stimulate normal gut movement.
- Monitor use of anti-diarrheal medicines: Avoid excessive use of medications like loperamide if constipation develops.
- Probiotics: Consider adding probiotic-rich foods or supplements to help restore gut flora imbalance post-diarrhea.
When to Use Medication
- Occasional use of stool softeners or mild laxatives may help relieve constipation, but avoid regular use without medical advice.
- Do not combine anti-diarrheal and laxative medications without consulting a healthcare provider.
Treating Underlying Disorders
- Address triggers or manage chronic disorders like IBS or IBD in partnership with your healthcare provider.
- Review and adjust medications that may contribute to your symptoms.
Dietary Tips for Recovery and Prevention
- Eat small, frequent meals as you recover from diarrhea.
- Focus on easily digested foods: bananas, rice, steamed vegetables, lean proteins.
- Slowly add whole grains and fruits as tolerated.
- Avoid excessive dairy, caffeine, high-fat foods, or artificial sweeteners that may trigger symptoms in sensitive individuals.
How to Prevent Shifts Between Diarrhea and Constipation
Prevention strategies depend on the specific causes, but these tips can help maintain regularity and digestive comfort:
- Maintain a balanced, fiber-rich diet, increasing intake slowly if your gut is sensitive.
- Stay well hydrated at all times, especially during illness or dietary transitions.
- Exercise regularly to support gut motility.
- Manage stress with relaxation techniques, deep breathing, or mindfulness.
- Keep a food and symptom diary if you suspect certain foods trigger your symptoms.
When to Seek Medical Help
Most cases of constipation following diarrhea resolve on their own. However, medical evaluation is needed if you experience any of the following:
- Symptoms last longer than one week
- Blood or mucus in your stool
- Unexplained weight loss
- Severe or persistent abdominal pain
- Dehydration, dizziness, or rapid heartbeat
- Symptoms in young children, older adults, or people with chronic conditions
Potential Complications
Untreated chronic bowel problems can sometimes lead to complications:
- Fecal impaction: Large, hard stool blockages that may require medical removal
- Overflow (paradoxical) diarrhea: Liquid stool leaks around impacted feces
- Hemorrhoids: Swollen veins in the rectum from straining
- Anal fissures: Small tears from passing hard stool
- Long-term inflammation: Increases risk of digestive complications
Frequently Asked Questions (FAQs)
Q: Is it normal to have constipation after diarrhea?
A: Yes, it is relatively common to experience constipation following diarrhea, typically due to changes in diet, medication use, or as a result of the gut recovering from an infection or inflammation.
Q: How long does constipation after diarrhea last?
A: It usually resolves within a few days, but if it lasts longer than a week or is accompanied by severe symptoms, consult your healthcare provider.
Q: Could this pattern indicate IBS or another digestive disorder?
A: Alternating diarrhea and constipation can be a symptom of IBS, especially IBS-M, or a sign of other conditions like IBD. If you have frequent cycles, discuss with a healthcare provider.
Q: What foods or drinks can help recovery?
A: Hydrating fluids, bananas, applesauce, oatmeal, steamed carrots, and plain rice are easy on the digestive system during recovery. Gradually add fiber-rich foods to prevent constipation.
Q: Should I use over-the-counter laxatives after diarrhea?
A: Use laxatives only under the advice of a healthcare professional, especially after digestive disturbances, to avoid aggravating symptoms or causing dependency.
Q: When should I see a doctor for constipation after diarrhea?
A: If you notice blood in your stool, unexplained weight loss, severe abdominal pain, dehydration, or if symptoms persist longer than a week, seek medical attention.
Summary Table: Causes and Remedies
| Cause | How it Leads to Constipation After Diarrhea | Suggested Remedy |
|---|---|---|
| Dietary Change | Reduced fiber/fluid after diarrhea | Gradually reintroduce fiber and fluids |
| Medications | Antidiarrheals slow gut movement | Discontinue or limit use, consult doctor |
| Gut Infections | Disrupted gut function during recovery | Hydrate, gentle foods, monitor symptoms |
| IBS/IBD | Cycle of inflammation & gut motility issues | Medical management, identify triggers |
| Paradoxical Diarrhea | Liquid leaks around impaction | Medical intervention may be needed |
Takeaway
Experiencing constipation after diarrhea is a common digestive issue, usually temporary and treatable with dietary adjustments, hydration, and gentle movement. However, persistent or recurrent symptoms, especially when accompanied by warning signs, should prompt consultation with a healthcare professional. Maintaining awareness of your digestive patterns and triggers is key to managing and preventing these uncomfortable swings.
References
- https://www.medicalnewstoday.com/articles/constipation-after-diarrhea
- https://www.healthline.com/health/diarrhea/paradoxical-diarrhea
- https://my.clevelandclinic.org/health/diseases/4059-constipation
- https://health.ucdavis.edu/blog/cultivating-health/from-loose-to-locked-up-tips-for-diarrhea-and-constipation-relief/2024/09
- https://cdhf.ca/en/constipation-what-to-do-if-you-cant-poop/
- https://www.health.harvard.edu/topics/bowel-problems
- https://www.healthline.com/health/video/20-natural-laxatives
- https://my.clevelandclinic.org/health/diseases/4342-irritable-bowel-syndrome-ibs
- https://www.kidshealth.org.nz/constipation-in-children
Read full bio of Sneha Tete












